Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 5 - Sep. / Oct. of 2012
Vol. 45 nº 5 - Sep. / Oct. of 2012
|
CASE REPORT
|
|
Nodular calcified neurocysticercosis with signs of reactivation* |
|
|
Autho(rs): Gustavo Nunes Medina Coeli1; Rodrigo Ribeiro Tiengo2; Afonso Carlos da Silva3; José Otávio Meyer Fernandes4; Guilherme Carlos da Silva1; Leandro Urquiza Marques Alves da Silva1 |
|
|
Keywords: Neurocysticercosis; Reactivation; Cerebral calcifications. |
|
|
Abstract: INTRODUCTION
Cysticercosis is an infection caused by the larval/metacestoid stage of the Taenia solium parasite, triggering inflammatory reactions in several organs, with tropism toward to the central nervous system(1). The infection for development of cysticercosis occurs through the ingestion of eggs or gravid proglottids present in contaminated water or food(2). Once the cysticerci are established in the nervous tissue, they are fought by the host's immune system, going through varied degrees of degeneration, namely, vesicular stage, colloidal vesicular stage, granular nodular stage, and nodular calcified stage which is the end stage of degeneration(3,4). Magnetic resonance imaging is the imaging method capable of differentiating among such larval stages. In the present report, the authors describe the case of a patient under suspicion of reactivation of neurocysticercosis. CASE REPORT A female, 64-year-old patient was admitted to the emergency unit of Hospital Escola de Itajubá, in November/2010, in postictal state, with subtle decrease in consciousness level and without any motor deficit. The patient reported a diagnosis of neurocysticercosis 40 years ago, with tonic-clonic convulsive seizures. As time went by her symptoms improved, but she continued presenting episodes of scintillating scotomas, dizzness and headache which improved spontaneously with rest. At admission, the patient underwent non-contrast-enhanced computed tomography that demonstrated the presence of nodular calcified lesions surrounded by a hypoattenuating halo, with fading of the adjacent cortical sulci and fissures compatible with vasogênico edema (Figure 1B). The study was supplemented with brain magnetic resonance imaging that in addition to the areas of edema demonstrated ring-shaped enhancement of the calcified lesions (Figures 2 and 3). 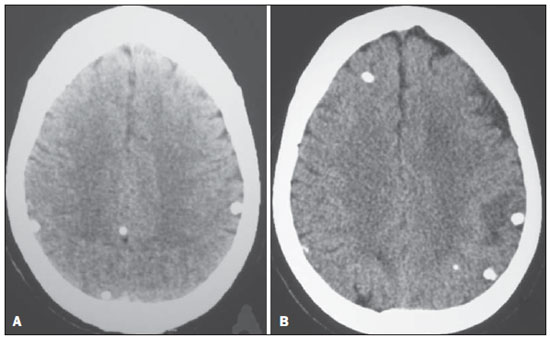 Figure 1. A: Non-contrast-enhanced axial computed tomography of skull, dated from 1989, demonstrating multiple calcified lesions, with no local expansile effect, compatible with the nodular calcified presentation of neurocysticercosis B: Most recent computed tomography image demonstrating calcified lesions, one of them with edematous halo in the left parietal lobe. 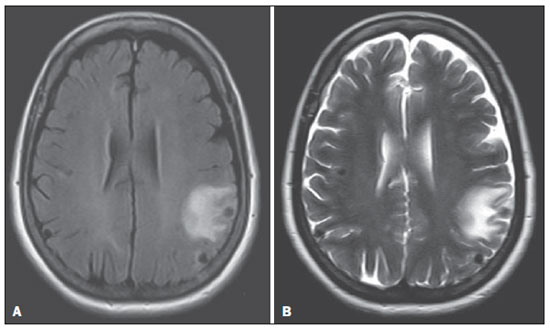 Figure 2. Axial FLAIR (A) and axial T2-weighted (B) magnetic resonance imaging, acquired in 2010, demonstrating multiple nodular lesions with hyposignal bilaterally in the parietal regions, the left-sided one with a hypersignal halo corresponding to vasogenic edema suggesting the presence of an acute process. 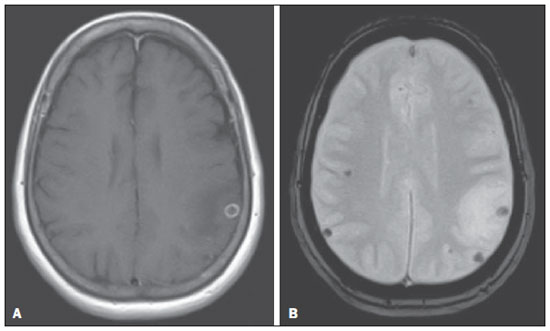 Figure 3. A: Post-contrast axial T1-weighted magnetic resonance imaging demonstrating that the left-sided parietal lesion surrounded dema presents ringshaped paramagnetic contrast uptake compatible with the ongoing inflammatory activity. B: Axial, T2-weighted gradient-echo magnetic resonance imaging which in correlation with computed tomography images confirms that multiple nodular lesions with hyposignal are calcified. Previous computed tomography images dated from 1989 demonstrated the presence of multiple calcified lesions without adjacent edema, compatible with nodular calcified presentation of neurocysticercosis (Figure 1A). As compared with the first computed tomography images, the current findings suggested reactivation of the calcified lesions. Upon imaging confirmation of the reactivation of neurocysticercosis, the patient remained in the hospital for nine days undergoing specific treatment with albendazole and drugs for management and prevention of seizures. The patient was discharged with no symptoms or sequelae, and is currently undergoing follow-up with a neurologist on an outpatient basis. DISCUSSION The study patient presented a form of disease considered as residual (granular calcified) with no clinical implication in most of cases so neglected as a possible cause of injuries. Before assuming the calcified stage, the parasite goes through a series of transformations, with different imaging findings. The cysticercus is considered as viable in the vesicular stage, i.e., lined by a transparent membrane containing liquid and the invaginated larva, with histologically intact areas of parasite tegument and other areas with inflammatory infiltrate, besides subtle gliosis. At this first stage, the immune response may range from tolerance to intense inflammatory reaction. Imaging findings are characterized by a cystic structure with scolex, generally non contrast-enhanced(3-5). The colloidal vesicular stage is characterized by necrosis of the larva, with thicker vesicle walls, and a cloudy or slightly gelatinous, whitish liquid. The scolex presents signs of hyaline degeneration. The relationship between the parasite tegument and the host is characterized by different forms of inflammatory reactions visualized on images as perilesional edema and ringshaped enhancement(3-5). The next stage is the granular nodular stage, where the size of the vesicle tends to decrease and its content becomes semisolid. In this stage, parasite remains can be visualized, the scolex is transformed into a mineralized granule and the inflammatory infiltrate is composed by mononuclear cells(3,4). Neuroradiological studies demonstrate a gradual decrease in edema, with onset of calcifications(5). Finally, in the nodular calcified stage, the parasite components cannot be identified, consisting in a mineralized solid nodule surrounded by a dense, non-modelled conjunctive tissue(3,4). At computed tomography or magnetic resonance imaging, it appears as a rounded, calcified nodule, without edema or contrast-enhancement(5). The nodular calcified stage is generally described as residual, but the ring-shaped contrast uptake and the perilesional vasogenic edema are compatible with the ongoing inflammatory process, in this context suggesting reactivation(5-8). Such data reinforce the difference in the pathologic meaning of lesions in this stage, enhancing the relevance of the present case since the patient had already calcified lesions previously documented by computed tomography for more than 20 years. Several hypotheses may explain such disease reactivation. Cerebral edema may be a result from the death of the parasite which was nonviable and not completely calcified(8). Another hypothesis refers to the release of insoluble and inaccessible antigens from dead cysticerci which, due to some still unknown reason, could be recognized by the host, triggering an inflammatory response(5,6). Some authors support the hypothesis that such a response may result from cross immunomediation by other agents(8). Regardless of the explanation, both physicians and radiologists must be aware that patients with calcified lesions of neurocysticercosis may present a new acute symptomatic condition in association with a perilesional inflammatory process. REFERENCES 1. Agapejev S. Epidemiology of neurocysticercosis in Brazil. Rev Inst Med Trop S Paulo. 1996;38:207-16. 2. Elias FM, Martins MT, Foronda R, et al. Oral cysticercosis: case report and review of the literature. 3. Lino-Júnior RS, Ribeiro PM, Antonelli EJ, et al. Características evolutivas do Cysticercus cellulosae no encéfalo e no coração humanos. Rev Soc Bras Med Trop. 2002;35:617-22. 4. Kimura-Hayama ET, Higuera JA, Corona-Cedillo R, et al. Neurocysticercosis: radiologic-pathologic correlation. Radiographics. 2010;30:1705-19. 5. Amaral L, Maschietto M, Maschietto R, et al. Unusual manifestations of neurocysticercosis in MR imaging: analysis of 172 cases. Arq Neuropsiquiatr. 2003;61:533-41. 6. Lino-Junior RS, Faleiros ACG, Vinaud MC, et al. Anatomopathological aspects of neurocysticercosis in autopsied patients. Arq Neuropsiquiatr. 2007;65:87-91. 7. Ooi WW, Wijemanne S, Thomas CB, et al. A calcified Taenia solium granuloma associated with recurrent perilesional edema causing refractory seizures: histopathological features. Am J Trop Med Hyg. 2011;85:460-3. 8. Sheth TN, Lee C, Kucharczyk W, et al. Reactivation of neurocysticercosis: case report. Am J Trop Med Hyg. 1999;60:664-7. 1. MDs, Residents in Radiology and Imaging Diagnosis, Hospital Escola de Itajubá, Itajubá, MG, Brazil. 2. Specialist in Radiology, Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), Physician Assistant, Department of Radiology and Imaging Diagnosis, Hospital Escola de Itajubá, Itajubá, MG, Brazil. 3. Geriatric Clinician, MD, Coordinator for the Program of Residency in Medical Practice, Hospital Escola de Itajubá, Itajubá, MG, Brazil. 4. MD, Neurologist, Hospital Escola de Itajubá, Titular Professor, Division of Clinical Neurology - Faculdade de Medicina de Itajubá (FMIt), Neuroradiologist at Clínica Sul Mineira Tomosul and Clínica Magsul, Itajubá, MG, Brazil. Mailing Address: Dr. Gustavo Nunes Medina Coeli Rua Oliveira Vieira de Souza, 456, Centro Prata, MG, Brazil, 38140-970 E-mail: gustavonmc@yahoo.com.br Received October 5, 2011. Accepted after revision May 7, 2012. * Study developed at Hospital Escola de Itajubá, Itajubá, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554