INTRODUCTION
Chordoid glioma of the third ventricle was first described in 1998 by Brat et al.(1), as a neoplasia located in the third ventricle, with the typical histological characteristic of chordoid neoplasias, but with peculiar immunohistochemical features related to positivity for glial fibrillary acidic protein (GFAP). Based on the histological, immunohistochemical and ultrastrutural characteristics of the tumor, as well as on its specific location, such authors considered this entity as a new tumor-like structure which was called "chordoid glioma".
In 2000(2), this disease was recognized by the World Health Organization(3) that nowadays considers it as a rare glioma with grade II malignancy, of uncertain histogenesis, predominantly affecting women (2:1), particularly adults in the age range between 30 and 60 years(4-6).
So far, few clinical cases - approximately 65(4) - have been published in the international scientific literature, so epidemiological, clinical, therapeutic and prognostic data about this disease can hardly be obtained.
CASE REPORT
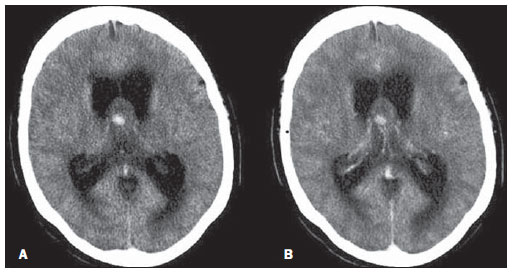
A 59-year-old woman with moderate holocranial headache, with no specific behavioral alterations. The patient was submitted to computed tomography (CT) which demonstrated the presence of a nodular, well delimited, round-shaped lesion measuring 2 cm in diameter, located at midline in the septum pellucidum, anteriorly to the thalami, determining obstruction of the interventricular foramina drainage, with consequential dilatation of the lateral ventricles (Figure 1).
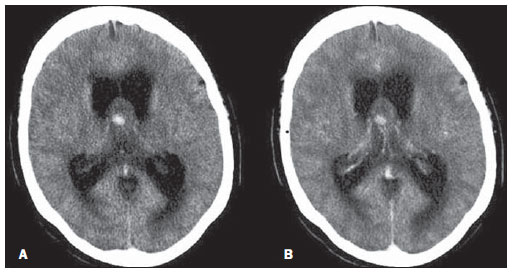
Figure 1. Computed tomography demonstrating the presence of a nodular lesion in the septum pellucidumwith an eccentric hyperattenuating focus (A) with no contrast enhancement in the post-contrast phase (B). There is obstruction of the liquor drainage, with lateral ventricles dilatation.
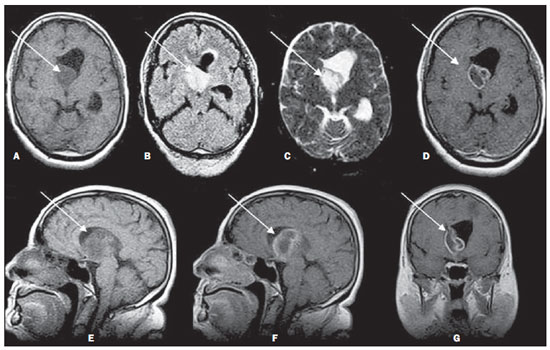
As an emergency approach for management of the obstructive hydrocephalus, the patient was submitted to ventriculoperitoneal shunting. At magnetic resonance imaging (MRI) performed immediately after the liquor drainage, the lesion could be visualized at the midline, projected onto the floor of the lateral ventricles, with hyposignal intensity on T1- and hypersignal intensity on T2-weighted and FLAIR sequences, with ring-shaped contrast enhancement (Figure 2).
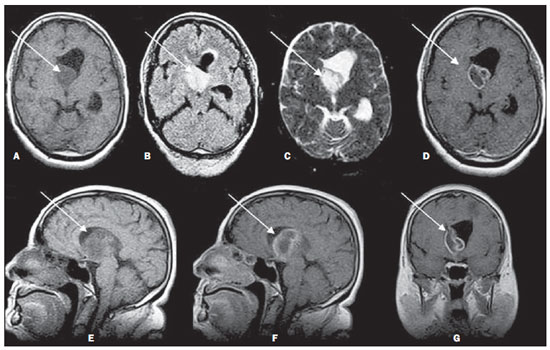
Figure 2. Magnetic resonance imaging performed after drainage of the right lateral ventricle. The lesion presents hyposignal intensity on T1-weighted (A: axial section; E: sagittal section), hypersignal intensity on FLAIR (B) and T2-weighted (C) images, with peripheral ring-shaped contrast enhancement (D: axial section; F: sagittal section, G: coronal section).
Histological study of a biopsy specimen revealed a tissue consisting of ovoid/polygonal cells with eosinophilic cytoplasm; e immunohistochemical analysis revealed immunoreactivity to GFAP and vimetin (VIM) and negativity to epithelial membrane antigen (EMA). The Ki67 was expressed in 20% of the tumor cells. Such findings have determined the diagnosis of glioma chordoid.
The approach adopted after the diagnosis included only follow-up and management of the hydrocephalus, with no surgical intervention. There was recurrence of complaints regarding headache, vomiting, decrease in level of consciousness and also daily fever peaks at 38ºC, besides episodes of fine tremor of lips, upper and lower limbs, with electroencephalogram compatible with epileptoid pattern
DISCUSSION
The clinical symptoms commonly described by patients are attributable to the specific tumor location in the anterior region of the third ventricle and to the involvement of adjacent structures responsible for possible endocrine alterations, visual defects and behavioral alterations, as well as symptoms secondary to an obstructive hydrocephalus (headache and nausea)(4,6).
Chordoid glioma is an ovoid lesion located in the region of the third ventricle which, in most of cases, appears hyperdense at CT (65%) and isodense at MRI T1weighted sequences (63%). However, in the present case, hyposignal intensity was observed on T1-weighted, and hypersignal intensity on T2-weighted sequences, which is described by the literature in 16% and 42% of cases, respectively(4). The literature reports that both at CT and MRI, after the administration of contrast agent, the lesion presents homogeneous enhancement in 68% and 70% of cases(4), respectively, which has not been observed in the present case, since there was no enhancement at CT and at MRI there was ring-shaped enhancement.
Histopathologically, chordoid glioma presents cords of ovoid to polygonal cells with eosinophilic cytoplasm which were accurately identified in the present case. Immunohistochemical analysis demonstrated a strong structure diffusely positive for GFAP and VIM, as well as for EMA, reported respectively in 100% and 67% of the cases described so far(4).
Clinically, there is a controversy over the most appropriate treatment, but most of described cases were surgically approached, some of them with either complete or subtotal resection of the tumor, and others with only lesion biopsy(4,6), like in the present case. The rates of mortality and complications related to the surgical procedures, such as diabetes insipidus, cognitive disorders, pulmonary embolism and hypothalamic dysfunction, are high. Complete tumor resection has lead to postoperative death in 29% of cases, and, for the survivors, 67% o chances of complications. In the cases where there was an option for partial resection, such indices decreased to 14% and 50%, respectively. In the cases where only biopsy was performed, neither deaths nor complications were reported(4).
REFERENCES
1. Brat DJ, Scheithauer BW, Staugaitis SM, et al. Third ventricular chordoid glioma: a distinct clinicopathologic entity. J Neuropathol Exp Neurol. 1998;57:283-90.
2. Brat DJ, Scheithauer BW, Cortez SC, et al. Chordoid glioma of the third ventricle. In: Kleihues P, Cavenee WK, editors. Pathology and genetics of tumours of the nervous system. 2nd ed. Lyon: IARC Press; 2000. p. 90-1.
3. Brat DJ, Scheithauer BW. Chordoid glioma of the third ventricule. In: Louis DN, Ohgaki H, Wiestler OD, et al., editors. WHO classification of tumours of the central nervous system. 4th ed. Lyon: IARC Press; 2007. p. 90-1.
4. Liu WP, Cheng JX, Yi XC, et al. Chordoid glioma: a case report and literature review. Neurologist. 2011;17:52-6.
5. Desouza RM, Bodi I, Thomas N, et al. Chordoid glioma: ten years of a low-grade tumor with higth morbidity. Skull Base. 2010;20:125-38.
6. Ortega-Martínez M, Cabezudo JM, Bernal-García LM, et al. Glioma cordoide del III ventrículo. Nuevo caso y revisión de la literatura. Neurocirugia (Astur). 2007;18:115-22.
1. Biomedical Scientist Specialist in Imaging, Faculdade de Medicina de Botucatu - Universidade Estadual Paulista "Júlio de Mesquita Filho" (FMB-Unesp), Botucatu, SP, Brazil.
2. Assistant Professor, Docent at Faculdade de Medicina de Botucatu - Universidade Estadual Paulista "Júlio de Mesquita Filho" (FMB-Unesp), Botucatu, SP, Brazil.
3. Assistant Professor, Faculdade de Medicina de Botucatu - Universidade Estadual Paulista "Júlio de Mesquita Filho" (FMBUnesp), Botucatu, SP, Brazil.
4. Full Professor, Faculdade de Medicina de Botucatu - Universidade Estadual Paulista "Júlio de Mesquita Filho" (FMBUnesp), Botucatu, SP, Brazil.
Mailing Address:
Patrícia Sanches
Hospital das Clínicas da Faculdade de Medicina de Botucatu
Distrito de Rubião Júnior, s/nº
Botucatu, SP, Brazil, 18618-970
E-mail: pavasanches@yahoo.com.br
Received May 1st, 2012.
Accepted after revision July 5, 2012.
* Study developed at Faculdade de Medicina de Botucatu - Universidade Estadual Paulista "Júlio de Mesquita Filho" (FMBUnesp), Botucatu, SP, Brazil.
 Vol. 45 nº 5 - Sep. / Oct. of 2012
Vol. 45 nº 5 - Sep. / Oct. of 2012