INTRODUCTION
Ectopic pregnancy is one of the most common first trimester complications and one of the most frequent causes of presentation of patients with acute abdominal pain to emergency departments, with an increase in incidence from 0.37% in 1948 to 2% of pregnancies in 1992(1), and with a considerable mortality rate currently estimated to be between 9% and 20%(2).
Such a remarkable increase in prevalence over the last two decades may result from different factors such as utilization of ultrasonography (US) apparatuses with higher sensitivity and more advanced technological resources, increased incidence of endometriosis among the general population, or disseminated utilization of laparo scopy(2).
As a parallel to the increase in incidence of such condition, morbidity and mortality rates have decreased, probably as a result of more swift and timely diagnoses allowed by technological developments in imaging diagnosis methods(3) whose utilization became indispensable for characterizing this entity.
In 95% of cases, the fertilized egg implantation occurs within the uterine tubes; and in the other 5% of cases, in the ovaries, cervical canal, prior Caesarean section scar or peritoneal cavity(3).
There are several risk factors implied in the ectopic pregnancy etiopathogenesis which are summarized as follows(3):
- prior ectopic pregnancy;
- previous history of pelvic inflammatory disease;
- previous history of gynecologic surgery;
- infertility;
- use of intrauterine devices;
- previous history of placenta previa;
- personal smoking history;
- recent use of
in vitro fertilization;
- congenital uterine anomalies;
- endometriosis;
- exposure to diethylstilbestrol.
CLINICAL AND LABORATORY FINDINGS
The most frequent clinical presentation includes mild lower abdominal pain, irregular vaginal bleeding and duration of amenorrhea ranging between five and nine weeks(3).
The main laboratory marker of this condition is serum β-hCG, whose levels increase by at least twice within a 48-hour period in patients with topic pregnancy up to 9-11 weeks. From the 12th gestational week, β-hCG levels stabilize, tending to remain on a plateau, persisting up to about the 20th week, and thereafter start decreasing progressively(3).
On the contrary, in cases of ectopic embryo implantation, the increase in serum levels is slower. In cases where the increase is < 50% of the previous values, there is a high likelihood of gestation abnormality, either intrauterine (ongoing miscarriage) or extrauterine(4).
It is important to observe that 85% of ongoing ectopic pregnancies may present an increase of more than 60% in β-hCG levels(4). Equally, a plateau occurring before the 9
th gestational week, with values below the expected value for the period, also suggests the possibility of ectopic pregnancy(4).
It is important to note that β-hCG levels should be > 2.000 mUI/ml to allow transvaginal US to demonstrate the presence of an intrauterine gestational sac(5). In cases where such evaluation is performed by transabdominal US, β-hCG levels should be around 6.500 mUI/ml(4).
IMAGING FINDINGS
The utilization of US in the routine prenatal follow-up has allowed pregnancy monitoring at the first gestational trimester(6), and this method has been the main imaging tool both in the normal prenatal follow-up and diagnosis of first-trimester abnormalities, with diagnostic criteria well established in the literature for the main abnormalities in this period(7), besides being the method of choice as the first approach for pregnant patients in emergency departments(2). The sonographic aspect of ectopic pregnancy varies according to the gestational age and location(7).
Despite the unquestionable utility of US in patients who arrive at emergency departments with acute abdominal pain, computed tomography (CT) and magnetic resonance imaging (MRI) have progressively been utilized as a first diagnostic method(8). Thus, patients who eventually present unsuspected signs of ectopic pregnancy may be primarily submitted to CT and MRI.
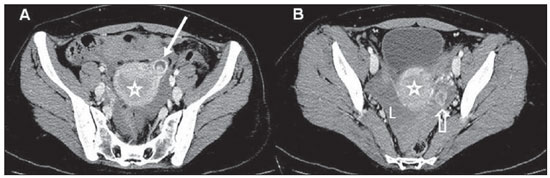
At CT, the main finding corresponds to a heterogeneous, predominantly cystic, adnexal mass with clear cleavage planes with ovaries and uterus, either in association or not with peripheral contrast enhancement. Common associated findings include presence of free fluid in the peritoneal cavity, many times with presence of intermingled hyperdense foci compatible with hematic content(9) (Figure 1).
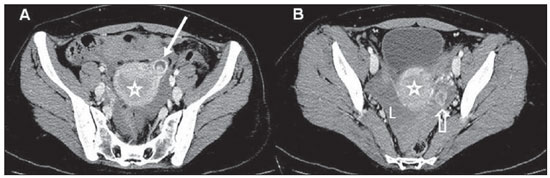
Figure 1. Ectopic pregnancy. Abdominal/pelvic CT. Image compatible with gestational sac in the left adnexal region (arrow on A), separated from the uterine image (stars on A and B) and from the ipsilateral ovary identified by visualization of the corpus luteum (hollow arrow on B). Also, note the presence moderate amount of fluid in the peritoneal cavity with foci of high density characterizing hematic content (L). (A,B: contrast-enhanced axial sections in the portal phase).
However, the presence of hemoperitoneum is not necessarily indicative of uterine tube rupture, but, the greater the amount of fluid, the higher is the probability of such complication(10).
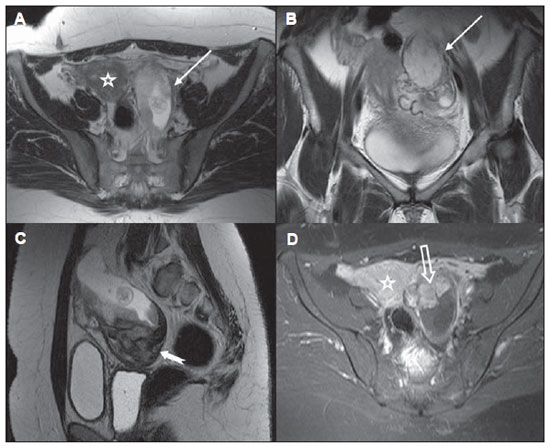
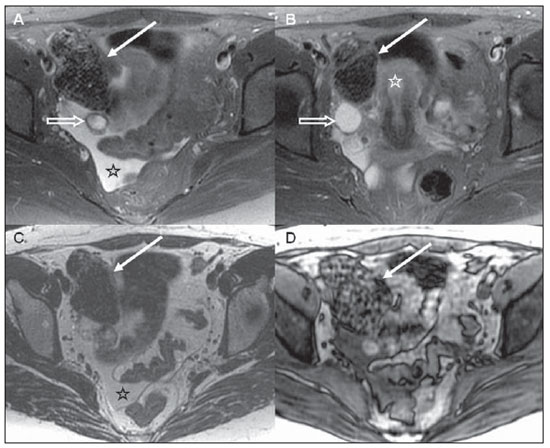
Because of the higher spatial and contrast resolution of pelvic structures, MRI can detect ectopic pregnancy more accurately than CT, with 95% sensitivity and 100% specificity for T2-weighted images(11). Findings include hematosalpinx, ascites with hematic content, and presence of adnexal mass/hematoma, as well as identification of a gestational sac in the adnexal region, with clear cleavage planes with uterus and ipsilateral ovary(8) (Figures 2 and 3).
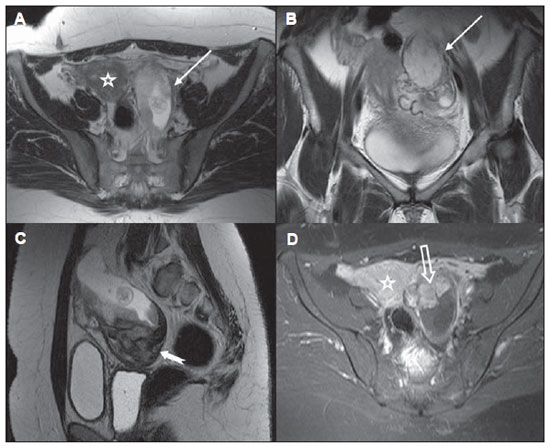
Figure 2. Ectopic pregnancy. Pelvic MRI. The presence of a gestational sac is observed in the left adnexal region (arrows on A and B), in association with a heterogeneous mass (arrow on C). Note the uterine and ovarian images (stars on A and D) separated from the adnexal mass, as well as the presence of placenta showing contrast enhancement (hollow arrow on D). (A: axial T2-weighted; B: coronal T2-weighted; C: sagittal T2- weighted; D: post-contrast axial T1-weighted images).
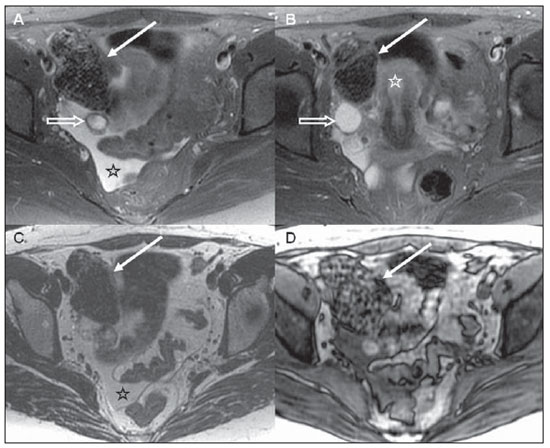
Figure 3. Ectopic pregnancy. Pelvic MRI. Expansile, heterogeneous mass in the right adnexal region (arrows on A to D), separated from the uterine (star on B) and ovarian (hollow arrows on A and B) images. Also, note the presence of moderate amount of free fluid in the pelvis, with intermediate signal intensity on T1-weighted images, suggesting hematic contents (stars on A and C). (A,B: axial T2- weighted image with fat saturation; C,D: axial T1-weighted, inphase and out-phase images).
The hematic content is represented by foci of high signal intensity on T1-weighted images with fat saturation, while T1- and T2-weighted images with fat saturation demonstrate contents with mixed signal intensity(8) (Figure 3).
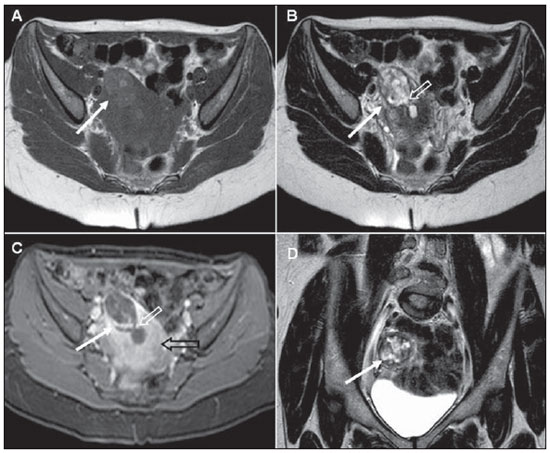
The fertilized egg implantation may occur in less common sites such as the cornual region. The corresponding findings may be seen on Figure 4.
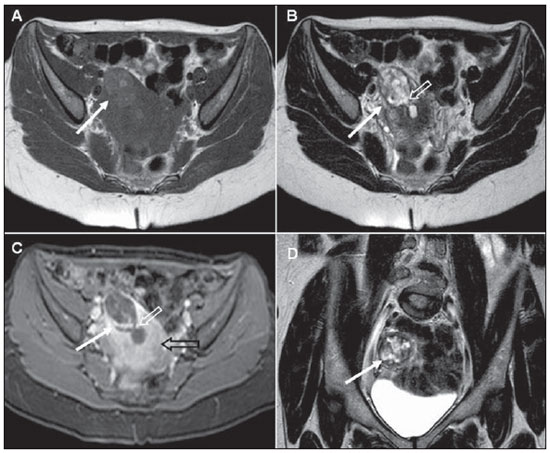
Figure 4. Cornual ectopic pregnancy. Pelvic MRI. The presence of a heterogeneous mass is observed in the cornual segment of the left uterine tube (white arrows on A to D). Note the communication with the uterine cavity (white hollow arrows on B and C). The myometrium is indicated by the black hollow arrow on C. (A,B: axial T1- weighted and T2-weighted images, respectively; C: post-contrast, axial T1-weighted image with fat saturation; D: coronal T2-weighted image).
In the present study, the authors have sought to illustrate the main CT and MRI findings of ectopic pregnancy. Such condition represents an important differential diagnosis for causes of abdominal pain of other origins, particularly in women of childbearing age. Thus, the increasing role played by CT and MRI in the evaluation of patients with acute abdomen of gynecologic origin raises the necessity for knowledge of findings of ectopic pregnancy by means of sectional imaging methods.
REFERENCES
1. Murta EFC, Tiveron FS, Barcelos ACM, et al. Análise retrospectiva de 287 casos de abdome agudo em ginecologia e obstetrícia. Rev Col Bras Cir. 2001;28:44-7.
2. Atri M, Leduc C, Gillet P, et al. Role of endovaginal sonography in the diagnosis and management of ectopic pregnancy. Radiographics. 1996;16:755-74.
3. Lin EP, Bhatt S, Dogra VS. Diagnostic clues to ectopic pregnancy. Radiographics. 2008;28:1661-71.
4. McWilliams GD, Hill MJ, Dietrich CS. Gynecologic emergencies. Surg Clin North Am. 2008;88:265-83,vi.
5. Levine D. Ectopic pregnancy. Radiology. 2007; 245:385-97.
6. Rolo L, Nardozza L, Araujo Jr E, et al. Correlação do volume da vesícula vitelínica obtida por meio da ultrassonografia tridimensional com a idade gestacional entre a 7ª e a 10ª semanas usando o método multiplanar. Radiol Bras. 2009;42:359-62.
7. Rios L, Oliveira R, Martins M, et al. Anormalidades do primeiro trimestre da gravidez: ensaio iconográfico. Radiol. Bras. 2010;43:125-32.
8. Dohke M, Watanabe Y, Okumura A, et al. Comprehensive MR imaging of acute gynecologic diseases. Radiographics. 2000;20:1551-66.
9. Furlan A, Fakhran S, Federle MP. Spontaneous abdominal hemorrhage: causes, CT findings, and clinical implications. AJR Am J Roentgenol. 2009;193:1077-87.
10. Lubner M, Menias C, Rucker C, et al. Blood in the belly: CT findings of hemoperitoneum. Radiographics. 2007;27:109-25.
11. Yoshigi J, Yashiro N, Kinoshita T, et al. Diagnosis of ectopic pregnancy with MRI: efficacy of T2*-weighted imaging. Magn Reson Med Sci. 2006;5:25-32.
1. Master, MD, Radiologist, Trainee at Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
2. Master, MD, Radiologist, Fellow PhD degree, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
3. MD, Radiologist at Centro Radiológico Campinas, Campinas, SP, Fellow, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
4. Associate Professor, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
Mailing Address:
Dr. Giuseppe D'Ippolito
Departamento de Diagnóstico por Imagem - EPM-Unifesp
Rua Napoleão de Barros, 800, Vila Clementino
São Paulo, SP, Brazil, 04024-002
E-mail: giuseppe_dr@uol.com.br
Received February 16, 2012.
Accepted after revision June 25, 2012.
* Study developed at Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
 Vol. 45 nº 5 - Sep. / Oct. of 2012
Vol. 45 nº 5 - Sep. / Oct. of 2012