INTRODUCTION
Soft tissue tumors comprise a great number of neoplasms, among them, mesenchymal tumors (the benign ones and sarcomas) and other tumors such as lymphomas, melanomas and metastatic carcinomas(1). Malignant mesenchymal tumors, called sarcomas, are characterized for being solid, with considerable heterogeneity in their anatomy, histological subtypes and degree of biological aggressiveness. The approach to be adopted is significantly influenced by the location and staging of the tumor(2).
Anatomopathological analysis allows the identification of tumor type, so it is essential for the therapeutic planning. The preoperative determination of grading and histological type of the sarcomas is critical to identify those patients at higher risk for metastasis, influencing the decision making on the the need for neoadjuvant treatment and surgery extent(3,4). The current parameters most utilized by pathologists for grading soft tissue sarcomas are the following: cellular differentiation, cellularity, amount of necrosis and number of mitoses(5).
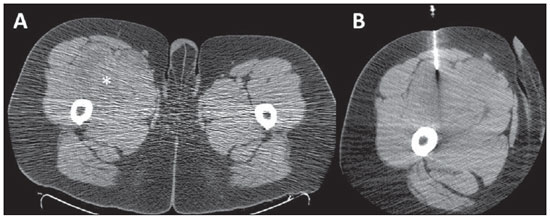
There are several techniques for obtaining soft tissue tumors specimens for histological analysis. Open surgical biopsy allows direct access to the tumor and generally the collection of larger amounts of material than in percutaneous biopsies, which tends to favor a correct diagnosis, increasing the capability of differentiating benign from malignant tissues. However, its main disadvantages are the high cost and morbidity, as it is the case in any open surgical procedure(6). For such reasons, percutaneous core needle biopsy (CNB) is many times utilized as a diagnostic method providing tissue fragments for histological analysis, with a low rate of complications. Percutaneous biopsies are usually guided by imaging methods such as ultrasonography (US) or computed tomography (CT), particularly in cases of deeply located tumors(7,8) (Figure 1). However, percutaneous biopsy results may underestimated tumor aggressiveness estimate, as only a small part of the tumor is analyzed(9).
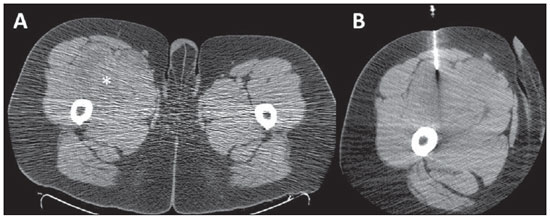
Figure 1. Percutaneous biopsy of an expansile mass in the thigh. A: Axial computed tomography section demonstrating the presence of heterogeneous illdefined mass in the anteromedial aspect of right thigh (asterisk). B: Percutaneous computed tomography-guided core needle biopsy directed to the most solid portion of the lesion. Anatomopathological results of biopsy demonstrated malignant fusocellular neoplasm, with morphological and immunohistochemical profile suggestive of synovial sarcoma with a high malignancy degree.
The main objectives of the present study were to evaluate the effectiveness of CTguided CNB of soft tissue tumors with respect to success in obtaining specimens for analysis, and comparing the diagnosis obtained by means of CNB with the anatomopathological result of the surgical specimen, when available.
MATERIALS AND METHODS
The present retrospective study reviewed records and diagnostic reports from patients with soft tissue tumors submitted to CT-guided CNB in a reference oncology center, in the period from April 22, 2003 to June 30, 2009. The present study was approved by the Committee for Ethics in Research of the institution before the commencement of data collection.
A standardized data form was retrospectively filled in for each patient included in the study. The collected information comprised epidemiological data, clinical data, imaging findings, CNB results, information on the surgery and respective anatomopathological report. For histological grading of the sarcomas, the World Health Organization (WHO) criteria based on a two-level reference classification ("low grade"
versus "high grade") were utilized. Whenever the utilized grading system was different, the conversion of such grading into the two-level system was performed, as recommended(10).
All the data were stored in a databank for statistical analysis by means of the SPSS software for Windows, version 17.0 (SPSS Inc.; Chicago, IL, USA). The descriptive analysis comprised the calculation of simple and relative frequencies of the studied variables. Sensitivity, specificity, predictive values and CNB accuracy were calculated for the differentiation between benign and malignant mesenchymal tumors. For the analysis of agreement between data regarding CNB results and surgical specimens analysis, the kappa test was utilized, with
p-value ranging between 0 and 1, indicating higher agreement as closer to 1.
RESULTS
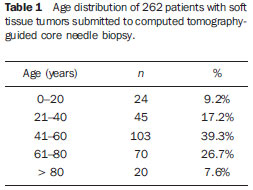
The present study included 262 patients, with a mean age of 51 years (ranging from 1 to 93 years), 132 (50.4%) men. Table 1 presents the age distribution of patients submitted to CNB. Most of the tumors were located in the trunk (
n = 127; 48.5%), followed by extremities (
n = 78; 29.8%), retroperitoneum (
n = 55; 21.0%) and head & neck (
n = 2; 0.8%).
Out of the 262 biopsies, appropriate specimens could be obtained in 215 cases (82,1%). Out of the 47 (18%) cases where the specimens were considered as being inappropriate, the histological result was absence of tumor in 33 cases (70%) followed by extensive necrosis in 8 cases (17%); collection artifacts in 3 cases (6%); inflammatory process in 2 cases (4%) and cellular debris intermingled with hemosiderin and red blood cells in one case (2%). The diagnoses of 23 of such patients was later obtained by tumor excision in 19 (83%) cases, open biopsy in 3 (13%) cases and additional CNB in 1 (4%) case. For the remaining 24 cases, no follow-up data was available.
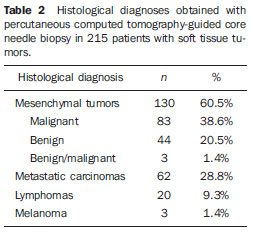
Table 2 presents the quantitative and percentage distribution of the histological results obtained by CNB.
Among the 44 benign mesenchymal neoplasms, it was possible to define the histological subtype by means of CNB in 34 cases (77.3%), with lipoma being the most frequent type (
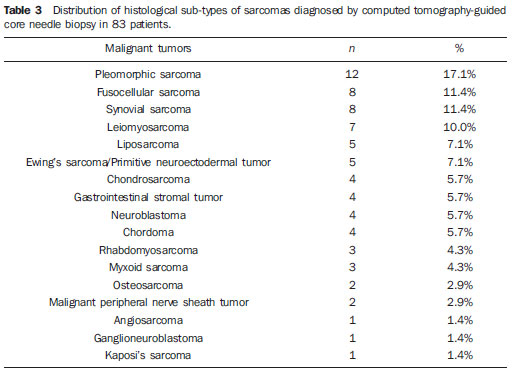
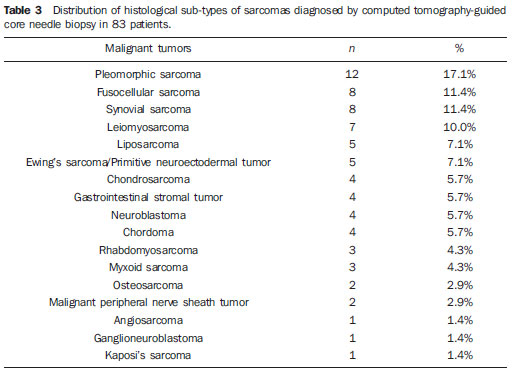
n = 17; 50%). As regards sarcomas, the histological sub-type was defined in 74 of the 83 cases (89.2%), with such cases being described on Table 3. Histological grading could be performed in 77 (92.8%) of the 83 patients with sarcomas, 60 (77.9%) of them being classified as high grade and 17 (22.1%) being classified as low grade.
Out of the 215 patients with tumors diagnosed by CNB, 116 (44.3%) underwent surgery for tumor excision and diagnosis confirmation. Among these cases, 74 had been classified as mesenchymal tumors at CNB - 19 benign and 55 malignant. Among the 19 tumors classified as benign at CNB, 17 were confirmed by the surgical specimens analysis and two results were discordant - one liposarcoma in a lesion classified as lipoma at CNB, and one synovial sarcoma in a lesion previously diagnosed as leiomyoma. Out of the 55 tumors classified as malignant by CNB, 2 (3.6%) presented discordant results in the surgical specimen analysis - one seminoma and one synovial cyst in two lesions classified as undifferentiated sarcomas at CNB.
Thus, CNB demonstrated 94.6% accuracy in the identification of sarcomas among the mesenchymal tumors, with sensitivity and positive predictive value of 96.4% and specificity and negative predictive value of 89.5%.
Out of the 77 patients with sarcomas whose histological grade could be determined by CNB, 49 were submitted to surgery, and only 4 (8.2%) of them presented difference in grading between CNB and surgical specimen analysis. All of such cases were classified as low grade at CNB and reclassified as high grade at the surgical specimen analysis. There was a significant agreement between CNB and surgical specimen analysis in the determination of the histological grade (high and low grade) (
p < 0.001; kappa = 0.75; CI 95%: 0.48- 1.00).
DISCUSSION
Soft tissue sarcomas are rarely found and the clinical/radiological differentiation between benign tumors and sarcomas is sometimes impossible. Furthermore, sarcomas may not be preoperatively suspected, with the diagnosis being confirmed only after the lesion resection. Enucleation (excisional biopsy) is acceptable in cases of benign lesions, but it is not appropriate for sarcomas, as the surgeon misses the opportunity to perform a more effective treatment, with better local management of the disease. Also, incisional biopsy is not routinely indicated for sarcomas because of the high rate of wound complications, which may compromise the local treatment(11). For this reason, CNB is the method of choice for preoperative investigation in patients with suspected soft tissue tumors(12). Fine needle aspiration biopsy is not recommended as a first-line diagnostic modality, however it can be utilized in selected cases, as in the suspicion of recurrence(12).
Imaging-guided CNB provides additional advantage for being capable of evaluating, at the collection moment, the best site for fragment collection, avoiding, for example, areas of necrosis and/or fibrosis. Narvani et al. have demonstrated that imaging-guided procedures improve the accuracy of CNB in 78% to 95%, specially in cases of small and deeply located lesions(13). Such procedure must be performed in a reference center, with specialized radiologists and pathologists, and the case must always be previously discussed with the surgeon for a better planning(12,14,15). During the procedure, the biopsy pathway must be planned in such a way that it can be resected at the moment of the definitive surgery, and several fragments from different areas should be collected for appropriate sampling of the tumor. According to Wu et al., at least four fragments must be collected in soft tissue tumors CNB in order to allow an appropriate histological diagnosis(16).
CT and US have been utilized to guide percutaneous biopsy of soft tissue tumors, with good results being reported in the literature(17-19). No study was found suggesting the superiority of either of the methods. One should select the method in which the lesion is best characterized and the one in which the radiologist is more experiented. In general, US is preferred for superficial lesions, while CT is utilized for deeper lesions.
In the present study, CNB provided appropriate specimens for analysis in 82% of the cases, allowing the differentiation between benign and malignant lesions, identification of the histological type of the tumors, and the histological grading in most of the cases. Such results confirm the accuracy of the method reported in literature, demonstrating that the sub-type and grading of the tumors can be determined in 80% to 95% of the CNBs(20). In the present study, sarcomas were the most prevalent soft tissue tumors, followed by metastatic carcinomas, benign mesenchymal tumors and lymphomas.
In the present casuistry, the diagnostic accuracy of CNB in the identification of sarcomas was high, with significant agreement in relation to the histological grading of the tumor by biopsy and by surgical specimen analysis. Such results were similar to those from other studies published in the literature. Ray-Coquard et al. have demonstrated 95% accuracy of CNB in the diagnosis of soft tissue sarcomas(21). Strauss et al. have evaluated 530 patients with soft tissue tumors submitted to CNB, reporting 426 mesenchymal tumors (225 malignant and 201 benign), and found 97.6% accuracy in the differentiation between malignancy and benignity, and 86.3% accuracy in the differentiation between high and low histological grade tumors(22).
Woon et al. have evaluated 94 patients submitted to surgery for soft tissue tumors and demonstrated that 95% of the patients preoperatively submitted to preoperative CNB had definitive one-stage surgery, as compared with 45% of those patients who were not submitted to biopsy(20).
CONCLUSION
CT-guided CNB demonstrated to be an effective diagnostic method in the evaluation of soft tissue tumors and in the histological grading of sarcomas, allowing for appropriate therapeutic planning.
REFERENCES
1. Weiss S, Goldblum J. Enzinger and Weiss's soft tissue tumors. 4th ed. St Louis, MO: Mosby; 2001.
2. Clark MA, Fisher C, Judson I, et al. Soft-tissue sarcomas in adults. N Engl J Med. 2005;353:701-11.
3. Mankin HJ, Hornicek FJ. Diagnosis, classification, and management of soft tissue sarcomas. Cancer Control. 2005;12:5-21.
4. Lopes A, Ferreira FO, Aguiar Junior S, et al. Sarcomas de partes moles no adulto. In: Kowalski LP, Guimarães GC, Salvajoli JV, et al., organizadores. Manual de condutas diagnósticas e terapêuticas em oncologia. 3ª ed. São Paulo, SP: Âmbito Editores; 2006. p. 681-90.
5. Nascimento A, Oliveira A. Patologia geral. In: Lopes A, organizador. Sarcomas de partes moles. Rio de Janeiro, RJ: Medsi; 1999. p. 41-68.
6. Cormier JN, Pollock RE. Soft tissue sarcomas. CA Cancer J Clin. 2004;54:94-109.
7. Chojniak R, Isberner RK, Viana LM, et al. Computed tomography guided needle biopsy: experience from1,300 procedures. Sao Paulo Med J. 2006;124:10-4.
8. Heslin MJ, Lewis JJ, Woodruff JM, et al. Core needle biopsy for diagnosis of extremity soft tissue sarcoma. Ann Surg Oncol. 1997;4:425-31.
9. Hoeber I, Spillane A, Fisher C, et al. Accuracy of biopsy techniques for limb and limb girdle soft tissue tumors. Ann Surg Oncol. 2001;8:80-7.
10. Sobin L, Wittekind C. Tumores ósseos e de partes moles. In: TNM Classificação de tumores malignos. 6ª ed. Rio de Janeiro, RJ: INCA; 2004. p. 115-24.
11. Serpell JW, Pitcher ME. Pre-operative core biopsy of soft-tissue tumours facilitates their surgical management. Aust N Z J Surg. 1998;68:345-9.
12. Grimer R, Judson I, Peake D, et al. Guidelines for the management of soft tissue sarcomas. Sarcoma. 2010;2010:506182.
13. Narvani AA, Tsiridis E, Saifuddin A, et al. Does image guidance improve accuracy of core needle biopsy in diagnosis of soft tissue tumours? Acta Orthop Belg. 2009;75:239-44.
14. Thway K, Fisher C. Histopathological diagnostic discrepancies in soft tissue tumours referred to a specialist centre. Sarcoma. 2009;2009:741975.
15. Rydholm A. Improving the management of soft tissue sarcoma. Diagnosis and treatment should be given in specialist centres. BMJ. 1998;317:93-4.
16. Wu JS, Goldsmith JD, Horwich PJ, et al. Bone and soft-tissue lesions: what factors affect diagnostic yield of image-guided core-needle biopsy? Radiology. 2008;248:962-70.
17. Zornoza J, Bernardino ME, Ordonez NG, et al. Percutaneous needle biopsy of soft tissue tumors guided by ultrasound and computed tomography. Skeletal Radiol. 1982;9:33-6.
18. Soudack M, Nachtigal A, Vladovski E, et al. Sonographically guided percutaneous needle biopsy of soft tissue masses with histopathologic correlation. J Ultrasound Med. 2006;25:1271-7.
19. Issakov J, Flusser G, Kollender Y, et al. Computed tomography-guided core needle biopsy for bone and soft tissue tumors. Isr Med Assoc J. 2003;5:28-30.
20. Woon DT, Serpell JW. Preoperative core biopsy of soft tissue tumours facilitates their surgical management: a 10-year update. ANZ J Surg. 2008;78:977-81.
21. Ray-Coquard I, Ranchère-Vince D, Thiesse P, et al. Evaluation of core needle biopsy as a substitute to open biopsy in the diagnosis of soft-tissue masses. Eur J Cancer. 2003;39:2021-5.
22. Strauss DC, Qureshi YA, Hayes AJ, et al. The role of core needle biopsy in the diagnosis of suspected soft tissue tumours. J Surg Oncol. 2010;102:523-9.
1. PhD, Titular and Director, Department of Imaging, Hospital A. C. Camargo, Professor at Faculdade de Medicina da Universidade Nove de Julho, São Paulo, SP, Brazil.
2. Graduate Student of Medicine, Faculdade de Medicina da Universidade Nove de Julho, Scholar, Programa Institucional de Bolsas de Iniciação Científica (PIBIC), Hospital A. C. Camargo, São Paulo, SP, Brazil.
3. Fellow PhD degree of Oncology, Titular, Department of Imaging, Hospital A. C. Camargo, São Paulo, SP, Brazil.
4. PhD, Titular, Department of Anatomic Pathology, Hospital A. C. Camargo, São Paulo, SP, Brazil.
5. PhD, Titular, Department of Pelvic Surgery, Hospital A. C. Camargo, São Paulo, SP, Brazil.
6. PhD, Titular and Director, Department of Pelvic Surgery, Hospital A. C. Camargo, São Paulo, SP, Brazil.
Mailing Address:
Dr. Rubens Chojniak
Hospital A. C. Camargo - Departamento de Imagem
Rua Professor Antônio Prudente, 211, Liberdade
São Paulo, SP, Brazil, 01509-010
E-mail: chojniak@uol.com.br
Received March 2, 2012.
Accepted after revision August 24, 2012.
* Study developed at Hospital A. C. Camargo, São Paulo, SP, Brazil.
 Vol. 45 nº 5 - Sep. / Oct. of 2012
Vol. 45 nº 5 - Sep. / Oct. of 2012