INTRODUCTION
Ovarian torsion is one of the most common causes of abdominal pain of adnexal origin, occurring in young patients and requiring the earliest possible intervention in an attempt to preserve the viability of the involved ovary(1) This condition manifests with rotation of the ovary and respective pedicle around the ovarian suspensory ligament(2).
Initially, the torsion compromises the venous and lymph nodes drainage, causing edema and ovarian enlargement and, with the passage of time, the arterial circulation is also compromised, resulting in thrombosis, ischemia and finally hemorrhagic infarct(2).
Such clinical picture may be observed in children, because of the excessive adnexal mobility(3), or in adult women, almost always in association with the presence of a large-sized ovarian solid or cystic mass. The risk increases in cases where the mass measures between 8 and 12 cm(4).
Tumors are responsible for approximately 50% to 90% of cases of ovarian torsion in adult women(2) and, among them, mature cystic teratoma is most frequently involved(1). Amongst the non-tumor-related causes of torsion, follicular and corpus luteum cysts are highlighted as the most commonly involved lesions, contributing with up to 17% of ovarian torsion cases(2).
Ovarian enlargement caused by hyperstimulation in women submitted to assisted reproduction techniques has been recently added to the spectrum of causative factors of ovarian torsion(2).
Equally, pregnancies with gestational time up to twenty weeks (specifically between 10 and 12 weeks) also determine a higher incidence of ovarian torsion, probably because the ovary is pushed anteriorly by the pregnant uterus, which determines the torsion(1).
CLINICAL AND LABORATORY FEATURES
The most common clinical sign is intermittent, unilateral pelvic pain which may improve or worsen according to the patient's positioning. Approximately 70% of patients complain of gastrointestinal symptoms such as nausea and vomiting, which may induce confusion with appendicitis, intestinal obstruction or mesenteric ischemia; and such symptoms may remain for days or even weeks(5).
Because of the intermittent signs and symptoms, with patients presenting mild complaints, the diagnosis is delayed, limiting the possibility of preserving the ovarian viability(5).
Physical examination may demonstrate a palpable, unilateral adnexal mass in up to 70% of cases, which may present a rapid enlargement caused by the progressive vascular congestion(2). Fever is an uncommon finding, occurring only in the presence of complications such as necrosis of the involved adnexa(1).
As regards laboratory tests, quantitative beta-hCG testing plays a relevant role in ruling out the diagnosis of ectopic pregnancy that is one of the main differential diagnoses of ovarian torsion. Blood count usually presents normal results, with a subtle decrease in hemoglobin levels or onset of leukocytosis in the presence of necrosis, which is uncommon and useful in the differential diagnosis with acute inflammatory pelvic disease(1).
IMAGING FINDINGS
Generally, the diagnosis of ovarian torsion is well defined by ultrasonography (US) in association with Doppler. Sectional imaging methods are only indicated either in cases where the signs and symptoms are suggestive of other causes of abdominal pain such as appendicitis and diverticulitis (that is not an uncommon finding), or in the presence of contraindication for US (for example, transvaginal US in virgin women), or inconclusive US results(6). The sonographic findings have already been described and are widely known(7), thus the present study is focused on findings of ovarian torsion at computed tomography (CT) and magnetic resonance imaging (MRI).
The imaging findings depend on the time of evolution of the ovarian torsion, and the most common - but least specific sign is the increase in the involved ovary volume. Such specificity increases if a central stroma is demonstrated without follicles, the latter being peripherically located, which reflects the result from edema and hemorrhage(2). Such a finding can be appropriately characterized either by contrast-enhanced CT or MRI T2-weighted sequences withy fat saturation(2).
The detection of hemorrhage of the ovarian parenchyma is extremely valuable, and the extent of such abnormality depends on the ovarian torsion degree and duration. Thus hemorrhagic infarct only occurs at late stages of the process, and the presence of subacute hematoma is highly associated with infarct and secondary necrosis of the involved ovary(2).
At CT, the presence of an adnexal mass separated from the uterus is frequently observed, and, in the case of mature teratomas as causative factor, the presence of macroscopic fat components plays a relevant role to define the diagnosis(8) (Figure 1).

Figure 1. Mature ovarian teratoma. Non-contrast-enhanced axial pelvic CT. The presence of a well defined nodular mass is observed in the adnexal region, with internal components presenting negative attenuation (–136 UH), confirming the fatty nature of the mass and the diagnosis of mature teratoma.
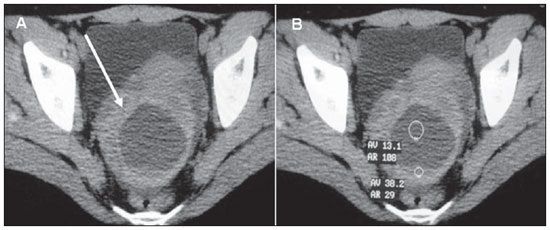
The uterus may present deviation toward the twisted side, and the following associated findings are frequently observed: ascites, obliteration of adjacent fat planes or even an enlarged ovary displaced from its regular positioning in the ovarian fossa(9,10) (Figure 2). Another quite useful sign is a twisted ovary located in the contralateral adnexal region, which may be observed on sequential images acquired before and after the torsion episode(8).
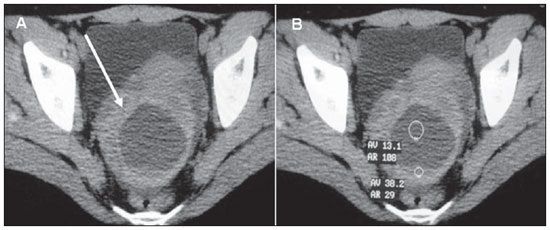
Figure 2. Ovarian torsion. Pelvic CT. The ovary presents enlarged dimensions and is located in the retrouterine region (arrow on A). The determining factor of the torsion is clearly demonstrated: a cyst with hemorrhagic content characterized by the presence of fluid level internally (density measurements on B) and by irregular contours and thickened borders. (A,B: non-contrast-enhanced pelvic CT, axial sections).
Additionally, the presence of ovarian hematoma resulting from hemorrhagic infarct can be appropriately characterized at non-contrast-enhanced CT, by the presence of foci with high density (30 to 50 UH), and, in case of densities > 60 UH there is a significant increase in the specificity for blood components(2).
The contrast-enhanced phase may demonstrate enlarged blood vessels around the adnexa, a finding consistent with the typical vascular congestion. Such vessels, as well as the corresponding tube and adnexum, may present a helical shape(3). However, the identification of the "wirl sign" representing the twisted ovarian pedicle around its axis is not frequent (less than one third of cases) and hardly definable ; however, when present, this is a pathognomonic finding of ovarian torsion(2).
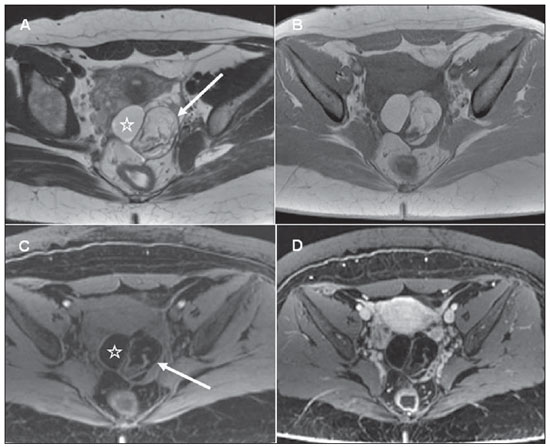
The MRI findings of ovarian torsion are very similar to those of CT, with the advantage of higher contrast resolution, identifying with equal clearness the presence of a mass with fat content by high signal intensity on T1-weighted sequences, and decreased signal intensity on the sequences acquired with fat saturation, which is compatible with mature teratoma(2) (Figure 3).
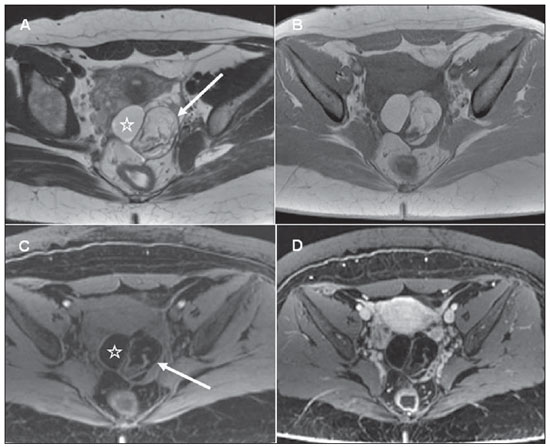
Figure 3. Ovarian torsion caused by a mature teratoma. Pelvic MRI. The left ovary is located in the retrouterine region. An adipose mass is demonstrated by the presence of foci of hypersignal on T2-weighted (A) and on T1-weighted (B) images, with decreased signal intensity on acquisitions with fat saturation (C), compatible with mature teratoma (star-shaped signs and arrows on A and C). (A: axial, T2-weighted image; B: axial T1-weighted image; C: axial T1-weighted image with fat saturation; D: axial T1-weighted images acquired with fat saturation after contrast agent injection).
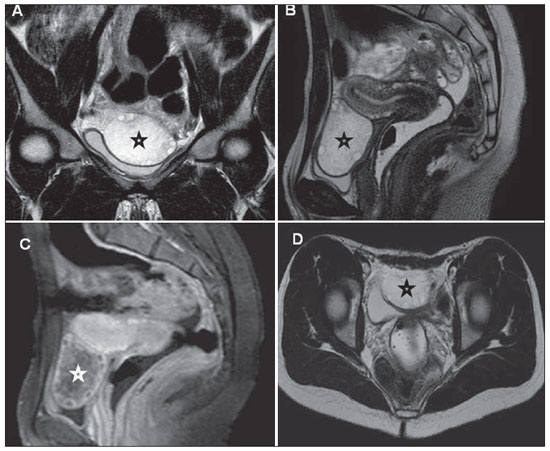
MRI can also demonstrate with higher clearness the enlarged ovary with edematous appearance, demonstrating increased signal intensity from the stroma on T2weighted images, as well as the peripheral follicles distribution (better characterized on T2-weighted sequences without fat saturation)(2) (Figure 4).
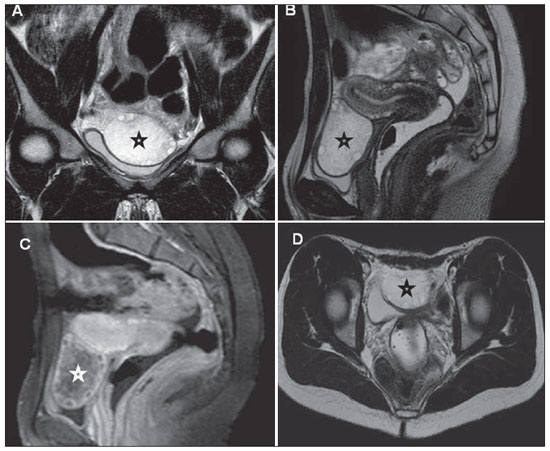
Figure 4. Ovarian torsion. Pelvic MRI. Right ovary located medially and anteriorly to the uterus, presenting enlarged dimensions and demonstrating multiple,peripherically distributed, small follicles (star-shaped signs). Also, anomalous, decreased and heterogeneous contrast-enhancement is observed in the compromised ovary (C). (A: coronal, T2-weighted image; B: sagittal, T2-weighted image; C: post-contrast sagittal T1-weighted image; D: axial, T2-weighted image).
Another useful sign to diagnose an ovarian torsion is the presence of foci of hemorrhagic infarct, whose high signal intensity is observed on T1-weighted sequences with fat saturation(10). This same finding may also be observed in other ovarian masses, but the presence of a halo of high signal intensity on T1-weighted images of an enlarged ovary, within the clinical context of acute abdominal pain, should raise such a hypothesis and indicate to the attending physician the necessity to proceed with the investigation(2).
The presence of an abnormally contrastenhanced ovary represents another sign suggestive of the diagnosis. In general, a heterogeneous, minimal or absent enhancement indicates the progression of ovarian torsion to ischemia or necrosis; but the presence of a normal contrast-enhancement of the ovary does not rule out such possibility, since, even in those cases, the arterial supply may be preserved(2). Frequently, the anomalous contrast-enhancement may not be clearly defined at CT and, because of the uncertainty regarding possible development of cystic masses or follicular cysts, such difficulty can be easily and simply resolved with MRI by its greater capability of tissue differentiation(2) (Figure 4).
As previously mentioned, the gestation may be a determining factor of ovarian torsion, with the same imaging findings at MRI, among them enlarged ovary with edematous appearance demonstrating increased signal intensity on its stroma on T2weighted images, as well as peripheral distribution of follicles(1) (Figure 5).

Figure 5. Ovarian torsion in a pregnant patient. Abdominal and pelvic MRI. The right ovary is enlarged, with multiple, peripherically distributed follicles, characterizing the torsion (star-shaped signs on the three images). Note the normal appearance of the left ovary on C (arrow). (A,B: axial T1- and T2-weighted images, respectively; C: coronal T2-weighted image).
In the present study, the authors have sought to illustrate the main MRI and CT findings of ovarian torsion. Such a condition is included in the range of differential diagnosis with causes of abdominal pain of other origins frequently observed in the daily practice of emergency department physicians. In this context, the increasing role played by CT and MRI in the assessment of patients with acute abdomen demand radiologists' familiarity with imaging findings of the main gynecological causes of this condition, contributing to the already well established role of ultrasonography.
REFERENCES
1. McWilliams GD, Hill MJ, Dietrich CS 3rd. Gynecologic emergencies. Surg Clin North Am. 2008;88:265-83.
2. Duigenan S, Oliva E, Lee SI. Ovarian torsion: diagnostic features on CT and MRI with pathologic correlation. AJR Am J Roentgenol. 2012;198:W122-31.
3. Bellah RD, Griscom NT. Torsion of normal uterine adnexa before menarche: CT appearance. AJR Am J Roentgenol. 1989;152:123-4.
4. Stenchever MA, Droegemueller W, Herbst AL, et al. Comprehensive gynecology. 4th ed. Philadelphia, PA: Mosby; 2001.
5. Houry D, Abbott JT. Ovarian torsion: a fifteenyear review. Ann Emerg Med. 2001;38:156-9.
6. Hiller N, Appelbaum L, Simanovsky N, et al. CT features of adnexal torsion. AJR Am J Roentgenol. 2007;189:124-9.
7. Martins WP, Leite SP, Nastri CO. Ultrassonografia pélvica em crianças e adolescentes. Radiol Bras. 2009;42:395-401.
8. Bennett GL, Slywotzky CM, Giovanniello G. Gynecologic causes of acute pelvic pain: spectrum of CT findings. Radiographics. 2002;22:785-801.
9. Kimura I, Togashi K, Kawakami S, et al. Ovarian torsion: CT and MR imaging appearances. Radiology. 1994;190:337-41.
10. Ghossain MA, Buy JN, Sciot C, et al. CT findings before and after adnexal torsion: rotation of a focal solid element of a cystic adjunctive sign in diagnosis. AJR Am J Roentgenol. 1997;169:1343-6.
1. MD, Radiologist, Trainee at Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
2. MD, Radiologist, Fellow, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
3. MD, Radiologist at Centro Radiológico Campinas, Fellow, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
4. Associate Professor, Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
Mailing Address:
Dr. Giuseppe D'Ippolito
Departamento de Diagnóstico por Imagem - EPM-Unifesp
Rua Napoleão de Barros, 800, Vila Clementino
São Paulo, SP, Brazil, 04024-012
E-mail: giuseppe_dr@uol.com.br
Received December 5, 2011.
Accepted after revision February 24, 2012.
Study developed at Department of Imaging Diagnosis, Escola Paulista de Medicina - Universidade Federal de São Paulo (EPM-Unifesp), São Paulo, SP, Brazil.
 Vol. 45 nº 4 - July / Aug. of 2012
Vol. 45 nº 4 - July / Aug. of 2012