Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 4 - July / Aug. of 2012
Vol. 45 nº 4 - July / Aug. of 2012
|
ORIGINAL ARTICLE
|
|
Evaluation of medical radiation exposure in pediatric interventional radiology procedures |
|
|
Autho(rs): Valéria Coêlho Costa Navarro1; Marcus Vinícius Teixeira Navarro2; Ana Figueiredo Maia3; Adriano Dias Dourado Oliveira4; Aline da Silva Pacheco Oliveira5 |
|
|
Keywords: Radiation protection; Interventional radiology; Pediatrics. |
|
|
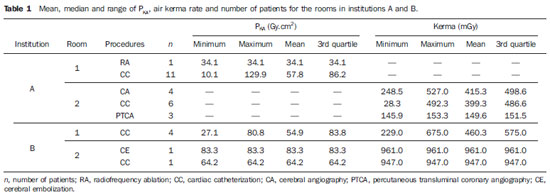
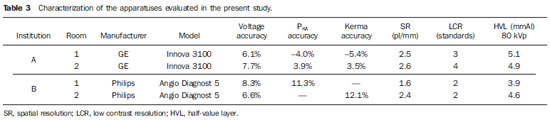
Abstract: INTRODUCTION
Interventional radiology comprises procedures with predominantly therapeutic objectives, utilizing a percutaneous approach and imaging guidance usually with fluoroscopy, but also computed tomography or magnetic resonance imaging(1). The number of invasive procedures utilizing interventional radiology in pediatrics has been increasing in recent years, as other medical specialties such as cardiology, hepatology and neurology have utilized this tool. Additionally, there is a strong trend towards the utilization of such technique in pediatrics considering that this is a group of patients at high surgical risk. Until not long ago, it was not possible to think about correction of complex cardiopathies, pulmonary venous drainage, correction of defects such as pulmonary and aortic stenosis, correction of urological disorders such as urolithiasis, among other indications, without a surgical intervention, a method that poses high mortality risk(2). Thus, interventional radiology is one of the applications of radiation in medicine whose benefits should exceed the risks, in compliance with the first and most fundamental principle of radiological protection, the principle of justification, even being the radiological practice with the highest levels of medical and occupational exposures, sometimes reaching the levels of deterministic effects. In such a context of possible high exposure levels, pediatric interventional radiology demands special attention, as children are more radiosensitive than adults because of high cell multiplication and longer life expectancy, with a risk for lethal cancer/ dose unit two to four times higher than for adults(3). As regards deterministic effects, there is a possibility of occurrence of severe radioinduced lesions, erythema, epilation, necrosis, sterility and cataract(4-8). Because of the above mentioned risks, studies have pointed towards the need for adopting specific approaches to optimize pediatric procedures by means of imaging quality assessment simultaneously with the investigation of radiation doses, with the purpose of maintaining them as low as possible(9-13). In the Brazilian State of Bahia, five hemodynamics centers perform pediatric procedures; but a demand of approximately 80% of such procedures is concentrated in the two hospitals involved in the present study, as the other three services only perform pediatric procedures in emergency situations. In order to ensure the representativeness of the sample, the information required for the present study was collected in these two services over a threemonth period. The low rate of pediatric procedures in the state is a consequence of the limited number of professionals qualified for the performance of such procedures. Thus, the present study was aimed at evaluating the pediatric exposure to radiation in interventional radiology procedures performed in two hospitals in the State of Bahia, Brazil, with a view of contributing to the construction of a scenario both at state and national levels, allowing for the knowledge of exposure levels and their optimization. MATERIALS AND METHODS The present study was undertaken in cooperation with two hospitals which perform pediatric procedures of interventional radiology in the city of Salvador, in the state of Bahia, Brazil. Each one of the A and B institutions have two rooms (1 and 2) available for pediatric procedures. The following apparatuses were utilized: Angio Diagnost 5 (Philips Medical Systems) in hospital A, and Innova 3100 (GE Healthcare) in hospital B. In the present study, the levels of radiation exposure in pediatric procedures performed between April and June 2011 were evaluated. The identity of both patients and institutions was not disclosed. It is important to highlight that both hospitals perform interventional procedures in adults and in children, and both face limitations in the number of professionals who perform pediatric procedures. Thus, their capacity to perform pediatric procedures is still limited, a fact which explains the small amount of data in the period. The procedures were categorized according to the medical specialty: 27 cardiological procedures and five brain procedures were studied, in a total of 32 procedures. Age and sex were the biometric data collected. In the statistical analysis, values of mean, median and range of air kerma distribution and air kerma area-product (PKA) were calculated. And, purposes of comparison adult reference level, the third quartile of the air kerma and PKA were calculated for pediatric procedures. The evaluations were performed by utilizing the indications from the gauges on the apparatuses themselves. In spite of the fact that all the apparatuses were equipped with transmission chambers with the possibility of indicating kerma and PKA, the indication of these two data was available only in rooms 1 and 2 of the institution B, while in the institution A, room 1, only the PKA indication was enabled, and in room 2, only the kerma indication was enabled. For the PKA assessment, the correction factor was initially calculated, taking as reference an external PKA meter manufactured by Iba Dosimetry. The meter was placed at the beam exit, over the equipment's head, and the results were corrected with basis on the obtained calibration factors. Thus, the PKA measurements in the present study are those indicated on the apparatuses, adjusted by the correction factor. The kerma values on the reference point indicated by the apparatuses, were corrected with basis on the values indicated by the Rapidose (Radcal Corporation) multimeter. Such multimeter was placed under the phantom CIRS NEMA XR21 configured as recommended by the manufacturer and in compliance with the IEC 601-2-43 item 203.5.2.4.5.101 (d). The meters utilized in the present study had calibration certificates valid until June 2012. The apparatuses of both institutions had their performance evaluated and, besides air kerma and PKA, the following parameters were verified: tube voltage, exposure time, half-value layer, filtration, spatial resolution, high contrast resolution, low contrast resolution, dynamic range and field size. As in only one service there was indication of scopy time and numbers of images, such parameters were not considered in the present study. RESULTS In the present study, 32 pediatric medical exposures were evaluated and categorized according to procedure, institution and room as shown on Table 1. The mean air kerma rate and PKA for each medical specialty are presented on Table 2. 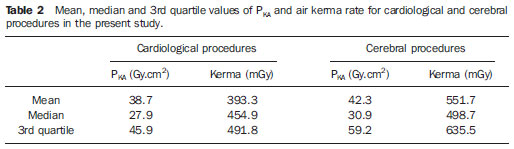 A summary of the parameters evaluated in the apparatuses is presented on Table 3. As regards the patients' age, the study sample comprised patients in the age range between 0 and 14 years. The age distribution is shown on Figure 1. 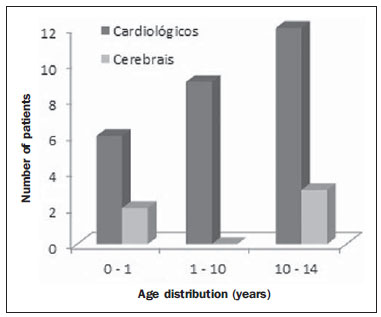 Figure 1. Distribution by age in the procedures categorized as cardiological and cerebral. In all age groups there were patients who were submitted to cardiological procedures, while no brain procedure was performed in patients in the 1 to 10 years age group. The age distribution by institution and by room is presented on Figure 2. 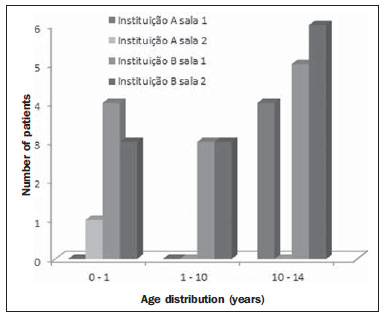 Figure 2. Age distribution by institution and by room. As regards sex, 41.9% of the patients were girls and 58.1% were boys. In the present study, techniques involving the brain - cerebral angiography and cerebral embolization - represented 16.1% of the procedures, while cardiological techniques - radiofrequency ablation, cardiac catheterization and transluminal coronary angioplasty represented 83.9% of the procedures. DISCUSSION In the present study, the evaluation of pediatric medical exposures for interventional cardiological and cerebral procedures, as compared with results of similar studies, demonstrated that the method utilized for PKA calculation was similar to that utilized by Bacher et al.(14) and Tsapaki et al.(8). In the evaluation of kerma, the authors utilized a method similar to that utilized for PKA, since other methods such as dosimetric films or thermoluminescent dosimetry were not available. The present results demonstrated PKA values between 57.8 and 64.2 Gy.cm2, while the maximum and minimum values were, respectively, 10.1 and 129.9 Gy.cm2. On the other hand, the mean PKA values obtained by Tsapaki et al.(8) for cardiac catheterization in a study involving 20 countries in Africa, Asia and Europe, with a pediatric population representing approximately 2% of the study sample, were between 0.1 and 36.7 Gy.cm2. Also, according to the study developed by Bacher et al.(14) to estimate the dose in a sample including 60 pediatric patients submitted to cardiac catheterization, the mean PKA value was 4.5 Gy.cm2, with maximum and minimum values of 0.4 and 20.4 Gy.cm2, respectively. As the above mentioned results are compared, the mean PKA values are between two and fourteen times higher and the maximum PKA value is approximately six times higher. As compared with the results found by Padovani & Quai(6) and by TECDOC1641(15) for procedures in adults, the PKA for cardiac catheterization was in the range of 12.0-67.0 Gy.cm2 and 5.1-221.0 Gy.cm2, respectively, which demonstrates that the results in the present study are similar to those found for adults and reported in the literature. It is important to highlight that such equivalence between the PKA ranges - pediatric and adult - may reflect the complexity of the studied pediatric procedures, as well as the need for optimization of the procedures in the mentioned institutions. As regards the kerma for cardiac catheterization, the mean results in the present study are between 399.3 and 947.0 mGy, while the minimum and maximum values were, respectively, 28.3 and 947.0 mGy. As such results are compared with those obtained by Bacher et al.(14) who obtained a mean value for cardiac catheterism of 23.9 mGy and interval between minimum and maximum values of 1.49 - 297.5 mGy, one observes that the results in the present study are much higher than those reported by the above mentioned authors, with the minimum value in the present study being above the mean value obtained by those authors. The mean kerma value obtained in the present study was 961.0 mGy for cerebral procedures, while the minimum and maximum values were respectively 248.3 mGy and 961.0 mGy. For PKA, the mean value was 83.3 Gy.cm2. In a similar study, Raelson et al.(16) obtained mean values between 103.8 and 340.3 Gy.cm2 for PKA and a mean value of 580.0 mGy for kerma. Rampado et al.(17), in a study on neurointerventional procedures in 18 pediatric patients, have obtained intervals between minimum and maximum values for kerma and PKA corresponding to, respectively, 88.0-1710.0 mGy and 16.7-343.0 Gy.cm2. As the results from the present study are compared with those reported by Raelson et al.(16) and Rampado et al.(17), one observes that the mean value for PKA in the present study is within the range of values reported by the mentioned authors, while, in the present study, the maximum kerma value is higher than that obtained by Raelson et al.(16) and lower than that obtained by Rampado et al.(17), a fact that may reflect the complexity of the cases under analysis. The cerebral techniques evaluated by Miller et al.(18) revealed third quartile values for cerebral embolization in adults in the range of 339.5-403.2 Gy.cm2 for PKA, well above the value found in the present study, which was 83.3 Gy.cm2, and third quartile values in the range of 4169.0-4441.0 mGy for kerma, also above the value in the present study, which was 961.0 mGy. As the analysis of dose by institution in the present study is considered, one observes that, for institution A, the maximum air kerma rate for cerebral procedures was 527.0 mGy, and for cardiac catheterization the maximum PKA value was 129.9 Gy.cm2. For the institution B, the maximum kerma and PKA values for cerebral procedures were 961.0 mGy e 83.3 Gy.cm2, respectively, while the results for cardiac catheterization were 675.0 mGy and 80.8 Gy.cm2 for kerma and PKA, respectively. In the present study, the groups were classified according to age and sex. As regards age, there was a prevalence of congenital cardiopathies in the neonatal (0-30 days) and in the infant (31 days-2 years) groups, indicating a predominance of cardiological procedures in these age groups(19). It is important to highlight that the body mass index cannot be disregarded as a routine information in the hemodynamics centers, as this is a contributing factor to be considered in the presence of high radiation doses, since the beam attenuation is related to the increase in the patient's body mass index(18). As the body mass index is related to the weight and height of the patient, such biometric data was not evaluated in the present study for not being available in the institutions. The differences observed between the institutions, as well as those between other studies, may be related to several other factors such as the complexity of each procedure, patients' weight and age, the level of the clinical staff or the utilized techniques. However, such parameters and correlations were not included as objectives of the present study, and, as the authors continue their investigations on pediatric interventional radiology, they will be evaluated. As regards the characterization of the apparatuses, in spite of the absence of specific Brazilian regulations on the assessment and performance of interventional radiology equipment, the Ordinance SVS/MS 453/ 98(20) establishes that interventional radiology is under its regulatory scope, with the fluoroscopy requirements being applicable to interventional radiology. All apparatuses included in the present study presented deviations < 10% in tube voltage indication, in compliance with the Ordinance SVS/MS 453/98(18). The deviations of the PKA and kerma indications were > 10% in two apparatuses. The visualization of the low contrast patterns should be capable of resolving, at least, three of the four patterns present in the phantom. Two of the four apparatuses were below the minimum level of visualization. All the apparatuses were equipped with the half-value layer > 2.6 mmAl, minimum value at 80 kVp, determined by Ordinance SVS/MS 453/98(20). Thus, based on the Brazilian regulations, it was possible to consider that all the apparatuses were compliant with respect to parameters of accuracy in the indication of tube voltage and half-value layer. However, as far as spatial resolution is concerned, all manufacturers indicate in their manuals, values between 4 and 5 pl/ mm. In the present study, the highest value was 2.6 pl/mm, and the lowest, 1.6 pl/mm, three times lower than the value informed by the manufacturer. The spatial resolution is an important parameter in the evaluation of imaging quality, which, in association with low contrast resolution, strongly influences the imaging quality; and their low performance values may increase examination time and, consequently, the medical exposures, on account of difficulties in the images visualization. CONCLUSION The present study results demonstrated exposure values up to 14 times those obtained in studies developed in other countries, with values similar to the results obtained for procedures in adults. Thus, it is possible to conclude that the high pediatric exposures indicate the need for constant optimization of procedures and assessment of exposures. The practice of not recording data on patients and procedures, such as biometric data, exposure time, kerma and PKA, hinders the performance of studies and the possibility of follow-up in those cases where the exposure levels are close to the deterministic effects threshold. Also, as the indication of scopy time and number of images were available in only one service, such parameters were not taken into consideration, which represented a limitation in the present study. The results of the present study are the first in the State of Bahia, and constitute a contribution towards delineating a scenario at state and national levels, with the prospect of contributing to the development of public policies, including specific regulations regarding interventional and pediatric radiology. Acknowledgements The authors wish to thank Instituto Federal de Educação, Ciência e Tecnologia da Bahia (IFBA), Universidade Federal de Sergipe (UFS), Instituto Nacional de Ciência e Tecnologia (INCT) em Metrologia das Radiações em Medicina and Instituto Nacional de Ciência Inovação e Tecnologia em Saúde (INCT-CITECS) for the technical and financial support. REFERENCES 1. World Health Organization. Efficacy and radiation safety in interventional radiology. Geneva, Switzerland: WHO; 2000. 2. Atik E. Cateterismo cardíaco intervencionista na cardiologia pediátrica. O posicionamento médico quanto às aplicações atuais e perspectivas. [Editorial]. Arq Bras Cardiol. 2002;79:443-5. 3. Pettersson HB, Fälth-Magnusson K, Persliden J, et al. Radiation risk and cost-benefit analysis of a paediatric radiology procedure: results from a national study. Br J Radiol. 2005;78:34-8. 4. Canevaro L. Aspectos físicos e técnicos da radiologia intervencionista. Rev Bras Fís Med. 2009;3:101-15. 5. Vano E, Sanchez R, Fernandez JM, et al. Patient dose reference levels for interventional radiology: a national approach. Cardiovasc Intervent Radiol. 2009;32:19-24. 6. Padovani R, Quai E. Patient dosimetry approaches in interventional cardiology and literature dose data review. Radiat Prot Dosimetry. 2005;117:217-21. 7. Rösch J, Keller FS, Kaufman JA. The birth, early years, and future of interventional radiology. J Vasc Interv Radiol. 2003;14:841-53. 8. Tsapaki V, Kottou S, Korniotis S, et al. Radiation doses in paediatric interventional cardiology procedures. Radiat Prot Dosimetry. 2008;132:390-4. 9. Aroua A, Besançon A, Buchillier-Decka I, et al. Adult reference levels in diagnostic and interventional radiology for temporary use in Switzerland. Radiat Prot Dosimetry. 2004;111:289-95. 10. Ubeda C, Vano E, Miranda P, et al. Radiation dose and image quality for paediatric interventional cardiology systems. A national survey in Chile. Radiat Prot Dosimetry. 2011;147:429-38. 11. Vano E, Ubeda C, Leyton F, et al. Radiation dose and image quality for paediatric interventional cardiology. Phys Med Biol. 2008;53:4049-62. 12. Silva MSR, Khoury HJ, Borrás C, et al. Dosimetria de pacientes e médicos em intervenções coronárias percutâneas em Recife, Pernambuco, Brasil. Radiol Bras. 2011;44:90-6. 13. Soares FAP, Pereira AG, Flôr RC. Utilização de vestimentas de proteção radiológica para redução de dose absorvida: uma revisão integrativa da literatura. Radiol Bras. 2011;44:97-103. 14. Bacher K, Bogaert E, Lapere R, et al. Patientspecific dose and radiation risk estimation in pediatric cardiac catheterization. Circulation. 2005;111:83-9. 15. International Atomic Energy Agency. Patient dose optimization in fluoroscopically guided interventional procedures. Final report of a coordinated research project. IAEA-TECDOC-1641. Vienna, Austria: IAEA; 2010. 16. Raelson CA, Kanal KM, Vavilala MS, et al. Radiation dose and excess risk of cancer in children undergoing neuroangiography. AJR Am J Roentgenol. 2009;193:1621-8. 17. Rampado O, Ropolo R. Entrances skin dose distribution maps for interventional neuroradiological procedures: a preliminary study. Radiat Prot Dosimetry. 2005;117:256-9. 18. Miller DL, Kwon D, Bonavia GH. Reference levels for patient radiation doses in interventional radiology: proposed initial values for U. S. practice. Radiology. 2009;253:753-64. 19. Miyague NI, Cardoso SM, Meyer F, et al. Estudo epidemiológico de cardiopatias congênitas na infância e adolescência. Análise em 4538 casos. Arq Bras Cardiol. 2003;80:269-73. 20. Brasil. Ministério da Saúde. Secretaria de Vigilância Sanitária. Diretrizes de proteção radiológica em radiodiagnóstico médico e odontológico. Portaria nº 453, de 1º de junho de 1998. Brasília, DF: Diário Oficial da União, 2 de junho de 1998). 1. Master, Fellow PhD degree, Postgraduate Programme in Physics, Universidade Federal de Sergipe (UFS), Professor at Instituto Federal de Educação, Ciência e Tecnologia da Bahia (IFBA), Salvador, BA, Brazil. 2. PhD, Professor at Instituto Federal de Educação, Ciência e Tecnologia da Bahia (IFBA), Salvador, BA, Brazil. 3. PhD, Professor at Universidade Federal de Sergipe (UFS), Aracaju, SE, Brazil. 4. MD, Hemodynamicist, Director for Quality at Sociedade Brasileira de Hemodinâmica e Cardiologia Intervencionista, Salvador, BA, Brazil. 5. Radiology Technologist, Scientific Initiation Student, Instituto Federal de Educação, Ciência e Tecnologia da Bahia (IFBA), Salvador, BA, Brazil. Mailing Address: Valéria Coêlho Costa Navarro Rua Apoema, 240, Condomínio Aldeia Jaguaribe, Piatã Salvador, BA, Brazil, 41613-044 E-mail: vccnavarro@gmail.com Received March 15, 2012. Accepted after revision July 2, 2012. Study developed in the Postgraduate Programme in Physics at Universidade Federal de Sergipe (UFS), Aracaju, SE, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554