Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 2 - Mar. / Apr. of 2012
Vol. 45 nº 2 - Mar. / Apr. of 2012
|
ICONOGRAPHIC ESSAY
|
|
Imaging evaluation of congenital cystic lesions of the biliary tract |
|
|
Autho(rs): Luis Ronan Marquez Ferreira de Souza1; Flávio Batista Rodrigues2; Lucas Vieira Tostes2; Graziella Borges Barreto2; Mateus Saldanha Cardoso3 |
|
|
Keywords: Magnetic resonance imaging; Choledochal cyst; Bile ducts. |
|
|
Abstract: INTRODUCTION
Congenital choledochal cysts are anomalies involving cystic dilatation of any segment of the biliary tract, and are most frequently identified in the common bile duct. The clinical presentation of such condition is characterized by a triad of signs and symptoms including abdominal pain, presence of palpable mass and jaundice(1). An accurate diagnosis is hardly achieved because this triad presents in only one third of patients(2). In adult individuals, besides the low incidence, the symptoms are usually nonspecific, and abdominal and right flank pain are most frequently reported, whether in association or not with previous cholecystectomy( 3,4). Because of such a clinical nonspecificity, this condition is included in the differential diagnosis of the most common biliary tract diseases(1). Imaging methods such as magnetic resonance imaging (MRI) and ultrasonography (US) are indicated for an early diagnosis of these cysts and their possible complications, besides aiding in a definitive surgical planning. PATHOGENESIS Although the pathogenesis of congenital choledochal cysts is discussable, it is considered that most probably such abnormality results from abnormal development of the pancreaticobiliary ductal system(5), as from the fourth gestational week. Such an abnormal development of the pancreaticobiliary ductal system is characterized by the extraduodenal junction of the choledochus with the pancreatic duct, out from the influence of the Oddi's sphincter. The formed duct is longer and is located in a higher position, which causes pancreatic juice reflux with consequential destruction of the mucosa, fibrosis and ductal dilatation( 1). However, congenital anomalies of the pancreaticobiliary junction are more frequently found that choledochal cysts. So, most probably, cysts development occurs due to an association of multiple factors, and not only because the abnormal development of the ductal system. DIAGNOSIS Ultrasonography is the primary method to be utilized in the evaluation of the biliary tree, considering its noninvasiveness, swiftness, low cost and wide availability. At ultrasonography, a well defined cystic lesion with variable echogenicity (generally hypoechoic) is observed. The relationship between the lesion and the gallbladder and the biliary tree, as well as the cleavage planes, must be carefully assessed. Color Doppler can be useful in the differentiation of adjacent vascular structures such as the portal vein. During endoscopic retrograde cholangiopancreatography (ERCP), the endoscope is passed and the Vater's papilla is characterized. Once the choledochus or pancreatic duct is reached, a contrast agent is injected into the biliary tract and the radiographic recording is concomitantly performed. Such imaging method was considered as the gold standard until the 70's decade, but currently it is most frequently utilized immediately before the surgical intervention(5) As ERCP images of patients with cystic lesions in the biliary tract are analyzed, it is possible to observe relevant alterations in the lesion pathogenesis(6). One of them is related to the location of the junction between the choledochus and the main pancreatic duct, which is far from the duodenum, creating a long common canal. Typically, such a junction forms an acute angle of 5º–30º but in cases of cystic lesions this angle is greater and may be > 90º. Because of the necessity of general anesthesia, ERCP is not indicated for the diagnosis in children. Additionally, the possibility of causing pancreatitis and the limitation of the method in the proximal evaluation of the biliary tree, which tends to be abnormal, constitute negative points to be taken into consideration. Magnetic resonance cholangiopancreatography (MRCP) represents an alternative for investigating the biliary tree anatomy, because it is noninvasive, does not require contrast injection and presents high accuracy in the identification of anatomical variations relevant for surgery(7). Additionally, MRCP allows the analysis of the proximal biliary tract and the evaluation of the liver and pancreas, facilitating other differential diagnoses, particularly in cases where the study is complemented with MRI of the upper abdomen. Computed tomography (CT) can also be utilized, particularly with those equipment which allow thinner section thicknesses such as multidetector apparatuses (multislice). With this method, the acquisition time is considerably shorter as compared with MRCP, which reduces motion artifacts. On the other hand, it is associated with inherent risks such as adverse reactions to contrast and excessive radiation resulting from repeated exposure at short intervals. At CT, choledochal cysts are seen as fluid collections, with density similar to the gallbladder and peripheral contrast enhancement of the cystic walls. CLASSIFICATION In the literature, the classification developed by Todani (Figure 1) is the most utilized for congenital choledochal cysts and involves the analysis of morphology, location and number of intra- and extrahepatic cysts by means of cholangiography. 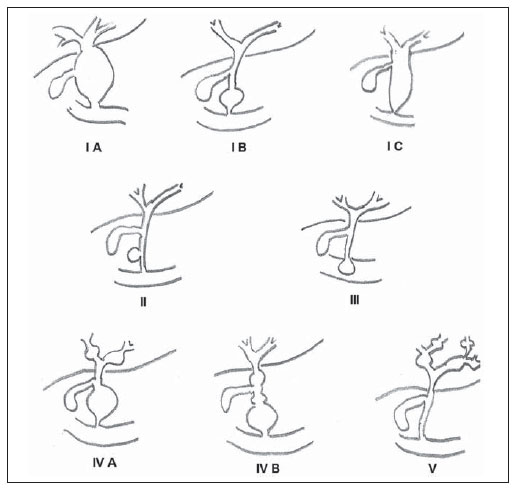 Figure 1. Todani's classification of congenital choledochal cysts. Type I cysts or classical choledochal cysts are restricted to extrahepatic bile ducts, and are further subdivided into three cyst subtypes as follows: Ia (diffuse) – diffuse dilatation of the choledochal duct and expansion through extrahepatic bile ducts (Figures 2 to 5); Ib (focal) – focal dilatation of the choledochal duct, with no anomalous pancreaticobiliary junction; Ic (fusiform) – fusiform dilatation of the choledochal duct associated with an anomalous pancreaticobiliary junction(2,8) (Figure 6). The prevalence is higher among children and, among the diagnosed cases, 7% of cysts are detected during pregnancy. Imaging findings, whether at US or other methods, demonstrate choledochus dilatations without any noticeable point of obstruction and with no intrahepatic ducts compromise. Pancreaticobiliary junction should be analyzed on thin section RMCP images for differentiation between cysts types Ia and Ic. At US, the cysts content appearance is variable and most frequently a finely heterogeneous pattern with sparse fine debris is observed.  Figure 2. Type Ia cyst. Right hypochondrium ultrasonography demonstrating cystic lesion with well defined limits containing thin septa and hyperrefringent echoes adjacent to the right hepatic lobe, in the gallbladder fossa. 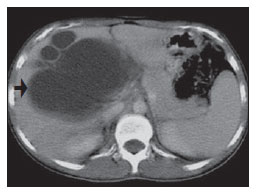 Figure 3. Type Ia choledochal cyst. Contrast-enhanced computed tomography demonstrating lobulated cystic lesion (arrow) with thin septa within the gallbladder fossa. The lesion is not enhanced after intravenous contrast injection.  Figure 4. Type Ia choledochal cyst. Abdominal magnetic resonance imaging – axial TSE T2- weighted sequence demonstrates cystic lesion with regular contours and hypersignal. Same patient on Figures 2 and 3. 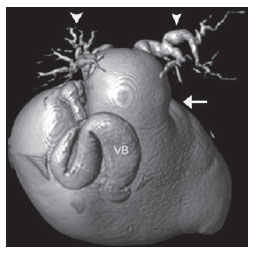 Figure 5. Type Ia choledochal cyst. Volume rendering image demonstrating gallbladder (GB) and giant choledochal cyst (arrow). 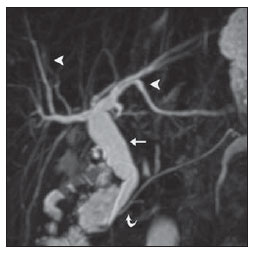 Figure 6. Type Ic choledochal cyst. MR-cholangiography image reconstruction demonstrating fusiform choledochal dilatation (straight arrow) associated with anomalous pancreaticobiliary junction (curved arrow). Note the absence of dilatation of intrahepatic bile ducts (arrowheads). Type II cysts are supraduodenal diverticula which may be found either in the common bile duct or in the common hepatic duct. Generally, these cysts arise from the lateral wall of the duct while the rest of the biliary tract remains normal(2,8) (Figures 7 to 9). At MRI, a small saccular dilatation can be observed near the gallbladder, with well defined limits, hypersignal on T2- weighted images, and communicating with the supraduodenal bile duct.  Figure 7. Type II choledochal cyst. MR-cholangiography image reconstruction demonstrating diverticulum (arrow) arising from the lateral wall of common hepatic duct, (Image kindly supplied by Doctor Carlos Matsumoto, Unifesp, São Paulo, SP, Brazil). 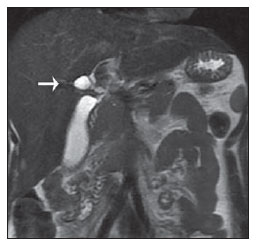 Figure 8. Type II choledochal cyst. Abdominal magnetic resonance imaging, coronal TSE T2-weighted image demonstrates the relation of a small saccular image (arrow) with hepatic duct and gallbladder. (Image kindly supplied by Doctor Carlos Matsumoto, Unifesp, São Paulo, SP, Brazil).  Figure 9. Type II choledochal cyst. MR-cholangiography image reconstruction demonstrating diverticulum (arrow) arising from lateral wall of common hepatic duct. (Image kindly supplied by Doctor Giuseppe D'Ippolito, Unifesp, São Paulo, SP, Brazil). Type III cysts (or choledochoceles) involve a dilatation of the intraduodenal common bile duct segment(2,8) (Figures 10 and 11). Choledochoceles clinically manifests, particularly in adults, as abdominal pain and jaundice complicated with cholangitis and pancreatitis. At MRI, a prominence of the major papilla is observed with a signal similar to the one of the biliary tract, projecting towards the wall of the second portion of the duodenum, determining a duodenal filling defect on contrastenhanced T2-weighted sequences. 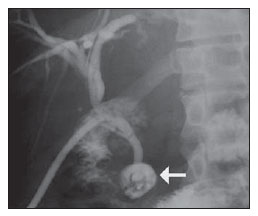 Figure 10. Type III cyst. Cholangiography through Kehr's drain demonstrates saccular dilatation of distal choledochus (arrow) adjacent to duodenal papilla (choledochoceles). (Image kindly supplied by Doctor Eduardo Crema, UFTM, Uberaba, MG, Brazil).  Figure 11. Type III cyst. MR-cholangiography image with volume rendering demonstrating other case of saccular dilatation of distal choledochus (arrow). Type IV cysts are represented by saccular formations in intra- or extrahepatic ducts, and are further subdivided into two subtypes, as follows: IVa – dilatation involving both intra- and extrahepatic bile ducts; and IVb – multiple saccular dilatations involving only extrahepatic bile ducts(2,8) (Figures 12 and 13). The main differential on imaging studies is the identification of more than one focus of saccular dilatation, with choledochal compromise and dilatation, which differentiates such cyst type from Caroli's disease. 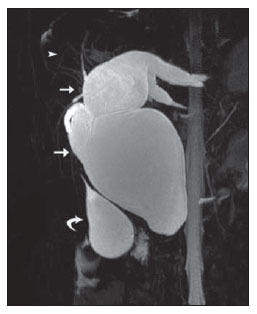 Figure 12. Type IV, MR-cholangiography image revealing marked intra- and extrahepatic bile duct dilatation (straight arrows). The intra-peripheral pathway (arrowhead) and gallbladder (curved arrow) are preserved. (Image source: Blasbalg R. Vesícula e vias biliares. In: Caldana RP, D'Ippolito G, editores associados. Gastrointestinal (Série Colégio Brasileiro de Radiologia e Diagnóstico por Imagem). 1ª ed. São Paulo, SP: Elsevier; 2011. p. 424).  Figure 13. Type IVb choledochal cyst. MR-cholangiography image reconstruction demonstrates multiple saccular formations only in extrahepatic ducts (straight arrow). Note the gallbladder (curved arrow) and the intrahepatic bile duct (arrowhead) with usual appearance. (Image kindly supplied by Doctor Giuseppe D'Ippolito, Unifesp, São Paulo, SP, Brazil). Type V cysts (or Caroli's disease) involve one or more segmental saccular dilatations of an intrahepatic bile duct which communicate to each other and affect large bile ducts(2,8) (Figures 14 and 15). It is a rare autosomal recessive disorder which causes varying degrees of inflammation, degeneration and dilatation of intrahepatic bile ducts resulting from a derangement in the normal embryological development. Caroli's disease clinically manifests with cholangitis, fever, pain in the hypochondrium and sometimes jaundice. Association with intrahepatic biliary calculi, cholangiocarcinoma and hepatic abscess is observed. A quite typical sign of Caroli's disease is the central dot sign, which corresponds to enhanced hepatic fibrovascular bundles (hepatic artery and portal vein), protruding into the lumen of dilated intrahepatic bile ducts. 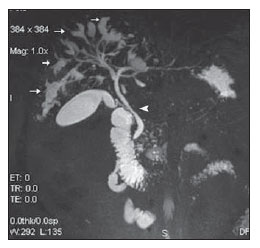 Figure 14. Type V cyst. MR cholangiography image presenting multiple cystic dilatations (arrows) communicating with intrahepatic biliary tree. The common choledochal duct (arrowhead) presents preserved caliber. (Image kindly supplied by Doctor Dr. Ricardo Vital, de Uberlândia, MG, Brazil). 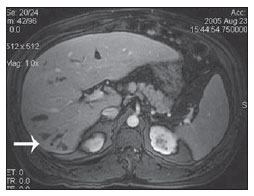 Figure 15. Type V cyst. Contrast-enhanced abdominal magnetic resonance imaging, 3D T1-weighted sequence with fat suppression demonstrating segmental dilatation of intrahepatic bile ducts (arrow). Furthermore, extremely rare cases of isolated dilatation of cystic duct are reported by Serena Serradel et al.(9) and Yoon(10), who have suggested that, in the future, this abnormality should be included in the classification as type VI cyst. COMPLICATIONS Most common complications from choledochal cystic lesions include choledochal lithiasis, carcinoma of gallbladder and ductus choledochus, chronic cholangitis, biliary obstruction, esophageal varices, cyst rupture, portal vein thrombosis and hepatic abscess. Biliary stasis resulting from ductal stenosis, and pancreatic juice reflux as a consequence of the alteration of the junction of the choledochus ductus with the main pancreatic duct, induce chronic irritation of the gallbladder epithelium and bile ducts. The progression of the chronic process of epithelial irritation may lead to metaplasia and also to dysplasia(11). Malignant degeneration is most frequently observed in cyst types I, IV and V, requiring lifelong follow-up even after complete surgical excision of the cyst(1,3). Because of the risks and complications, surgical management of the choledochal cyst must be performed as soon as possible. Generally, there are two treatment options, namely, complete cyst resection and cyst drainage. Complete cyst excision is the treatment of choice, in spite of the disadvantage of requiring bile duct reconstruction. CONCLUSION The late diagnosis of congenital choledochal cysts results from the low frequency of this condition besides the nonspecificity of clinical signs and symptoms. Therefore, in the suspicion of a possible choledochal cyst, the time to the final diagnosis should be shortened with most appropriate imaging methods such as US and MRCP. The radiologist should classify the cysts, besides identifying possible association with other congenital abnormalities and their complications which could eminently make the surgical planning more difficult. REFERENCES 1. Edil BH, Olino K, Cameron JL. The current management of choledochal cysts. Adv Surg. 2009;43:221–32. 2. Mortelé KJ, Rocha TC, Streeter JL, et al. Multimodality imaging of pancreatic and biliary congenital anomalies. Radiographics. 2006;26:715–31. 3. Matos C, Nicaise N, Devière J, et al. Choledochal cysts: comparison of findings at MR cholangiopancreatography and endoscopic retrograde cholangiopancreatography in eight patients. Radiology. 1998;209:443–8. 4. Mabrut JY, Bozio G, Hubert C, et al. Management of congenital bile duct cysts. Dig Surg. 2010;27:12–8. 5. Babbitt DP, Starshak RJ, Clemett AR. Choledochal cyst: a concept of etiology. Am J Roentgenol Radium Ther Nucl Med. 1973;119:57–62. 6. Kim OH, Chung JH, Choi BG. Imaging of the choledochal cyst. Radiographics. 1995;15:69–88. 7. Lee HK, Park SJ, Yi BH, et al. Imaging features of adult choledochal cysts: a pictorial review. Korean J Radiol. 2009;10:71–80. 8. Todani T, Watanabe Y, Narusue M, et al. Congenital bile duct cysts: classification, operative procedures, and review of thirty-seven cases including cancer arising from choledochal cyst. Am J Surg. 1977;134:263–9. 9. Serena Serradel AF, Santamaría Linares E, Herrera Goepfert R. Cystic dilatation of the cystic duct: a new type of biliary cyst. Surgery. 1991;109(3 Pt 1):320–2. 10. Yoon JH. Magnetic resonance cholangiopancreatography diagnosis of choledochal cyst involving the cystic duct: report of three cases. Br J Radiol. 2011;84:e18–22. 11. Todani T, Watanabe Y, Fuji M, et al. Carcinoma arising from the bile duct in choledochal cyst and anomalous arrangement of the pancreatobiliary ductal union. Journal of Biliary Tract & Pancreas. 1985;6:525–35. 1. PhD, Professor at Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil. 2. Graduate Students of Medicine, Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil. 3. MD, Resident of Radiology and Imaging Diagnosis, Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil. Mailing Address: Dr. Luís Ronan Marquez Ferreira de Souza Disciplina de Radiologia e Diagnóstico por Imagem – UFTM Avenida Frei Paulino, 30, Bairro Abadia Uberaba, MG, Brazil, 38025-180 E-mail: luisronan@gmail.com Received July 22, 2011. Accepted after revision January 30, 2012. Study developed at the Division of Radiology and Imaging Diagnosis of Faculdade de Medicina da Universidade Federal do Triângulo Mineiro (UFTM), Uberaba, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554