INTRODUCTION
Thoracolumbar burst fracture was first described by Sir Frank Holdsworth, in 1963(1), as an injury typically resulting from fall from height or motor vehicle accidents, causing a significant axial load on the spine, leading to a failure by compression of the anterior, middle and posterior vertebral columns(2). Most burst fractures occur at the level of the thoracolumbar junction whose vulnerability is partially explained by the anatomic and biomechanical features of the region. Such an explanation is due to the radial shape of the thoracic cage and stability provided by the costotransverse ligaments in the thoracic spine which give a higher resistance to load in the coronal and sagittal planes, and to axial rotation. Such a protection degree and the relatively rigid shape contrast with the underlying lumbar spine – more flexible and less protected than the thoracic spine –, resulting in a fragile segment that is named thoracolumbar transition (T11-L2)(3). In a specific study developed by Avanzi et al.(2), 83% of injuries have occurred between T12 and L2, the first lumbar vertebra being the most affected, likewise in studies developed by other authors(4–7).
Currently, there is a consensus in the medical literature about the best approach to be adopted in the treatment of vertebral fractures types such as luxation, flexion/ distraction and wedge fractures, but not on the treatment of burst fractures, since most patients neither present neurological deficit nor meet direct instability criteria(2,3,8– 10). So, the decision making process about the best treatment to be adopted for thoracolumbar burst fractures is based on indirect vertebral instability criteria(2,5,11–13).
The main instability criteria adopted by spine surgeons to evaluate burst fractures are the following: extent of height loss of the anterior wall of the fractured vertebra, level of spinal canal compromise by bone fragments, degree of kyphosis, and degree of widening of interspinous and interpedicular spaces(2,11–14).
Based on such criteria which have already been defined by the literature, surgeons can determine the likelihood of vertebral collapse and progression to late neurological deficit, besides estimating the post-treatment residual pain, and also to change de fracture classification, considering that for each criterion there is a question to be answered before the definition of the treatment.
The motivation for developing the present study is the necessity of standardizing and diffusing the main treatment techniques and radiological findings, with basis on the main spinal instability criteria utilized by surgeons in the assessment of thoracolumbar burst fractures, with the objective of helping them to define the best form of management for these patients
MATERIALS AND METHODS
Radiological routine
In a systematic fashion, the authors started the radiological workup to evaluate patients with suspected thoracolumbar burst fracture utilizing posteroanterior (PA) and lateral views of spine radiography. Posteroanterior (PA) view allows the measurement of widening of interspinous and interpedicular spaces, according to the Neumann's method(13).
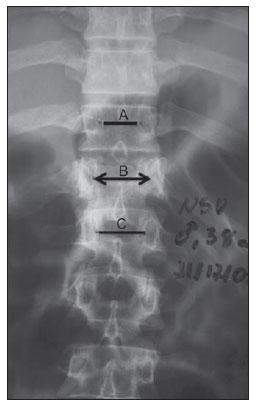
The calculation of the degree of widening of interpedicular space of the injured vertebra is based on the average of interpedicular spaces between the fractured vertebra and the immediately superior and immediately inferior vertebrae(2,12), corresponding to the rate of widening of the interpedicular space (Figure 1). The measurement of the interpedicular space was performed with a transparent ruler with a millimeter scale.
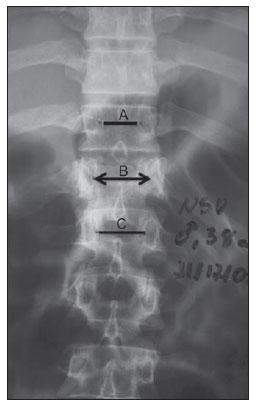
Figure 1. Calculation of interpedicular distance. Postero-anterior radiography of thoracolumbar spine demonstrating interpedicular distances at the level of the fracture (B) and between the injured vertebra and the immediately superior and immediately inferior vertebrae (A and C, respectively). The mean interpedicular distance is calculated by subtraction of the interpedicular distance at the level of the fractured vertebra on the average between the interpedicular distances of the vertebrae immediately superior and immediately inferior to the fractured vertebra, multiplied by 100, according to the following formula: {(A+C)/2 – B}/(A+C)/2 × 100. Example: A = 2.0 cm, B = 3.0 cm, C = 2 cm; so, {(2+2)/2} – 3/(2+2)/2 = –1/2 = 50%.
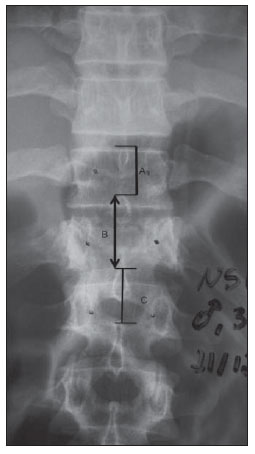
Also on the PA view, the Neumann's method(13) allows the measurement of the variation of the distance between the spinous processes which constitutes an indirect sign of injury to structures of the posterior spinal column. The method consists in marking the distance from the upper border of the spinous processes projected on PA radiographs. Variations of up to 7 mm in the distance is considered as normal, also allowing the calculation of the percentage of spinous processes widening, with 20% being considered as unstable posterior ligamentous complex, requiring surgical treatment (Figure 2).
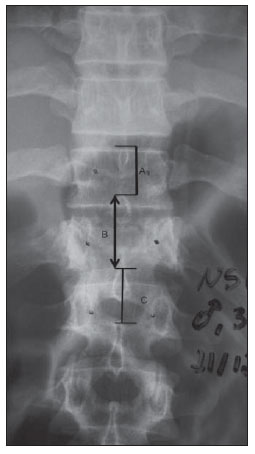
Figure 2. Calculation of the interspinous distance. Postero-anterior radiography of thoracolumbar spine demonstrating the distances between spinous processes at the level of the fracture (B) anda t the superior and inferior levels (A and C, respectively). The mean interspinous distance is calculated by subtraction of the interspinous distance at the level of the fractured vertebra on the average between the interspinous distances of the vertebrae immediately superior and immediately inferior to the fractured vertebra, multiplied by 100, according to the following formula: {(A+C)/2 – B}/(A+C)/2 × 100. Example: A = 2 cm, B = 3 cm, C = 3 cm; so, {(2+3)/2 – 3}/(2+3)/2 = –0.5/2.5 = 20%.
Continuing the radiological evaluation, the authors utilized the lateral view of the spine which allows the evaluation of the rate of height loss of the anterior wall of the vertebra affected by compression fracture. For this purpose, the authors utilized the method developed by Willén et al.(11), utilizing the average between the heights of the vertebral bodies immediately superior inand inferior to the fractured vertebrae to obtain the rate of height loss of the anterior wall of the fractured vertebra (Figure 3).

Figure 3. Calculation of vertebral bodies height. Lateral radiography of thoracolumbar spine demonstrating the height of the anterior wall of the fractured vertebral body (B) and of the vertebral bodies immediately superior and immediately inferior to the fractured vertebra (A and C, respectively). The average between the superior and inferior vertebral bodies is calculated by subtraction from the height of the fractured vertebral body, on the average between the heights of the superior and inferior vertebral bodies, multiplied by 100, according to the following formula:: {(A+C)/2 – B}/(A+C)/2 × 100. Example: A = 3 cm, B = 2 cm, C = 3 cm; so, {(3+3)/2 – 2}/(3+3)/2 = 1/3 = 33%.
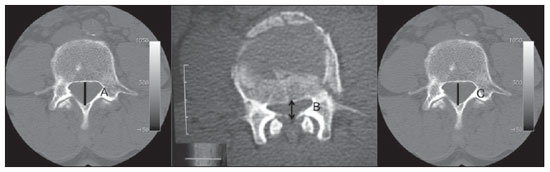
Continuing the imaging workup, the utilization of computed tomography may provide data regarding the fracture trace analysis and evaluation of the involvement of the vertebra components, with possibility of utilizing sagittal and coronal image reconstructions. Such method allows a highly accurate assessment of the vertebral canal compromise by bone fragments (retropulsion of the posterior wall of the vertebral body) by measuring the mid-sagittal diameter, as proposed by Trafton and Boyd, in 1984(12), and of the presence of lamina fracture.
The evaluation of the percentage of vertebral canal stenosis as proposed by Trafton and Boyd is based on the average between the values found on axial CT sections of the superior and inferior vertebrae adjacent to the affected vertebra. The evaluation of the neural canal narrowing produced by burst fracture was performed by measuring the mid-sagittal diameter of the canal on CT sections at the level of the affected vertebra, expressed as a percentage in comparison with the adjacent levels (Figure 4).
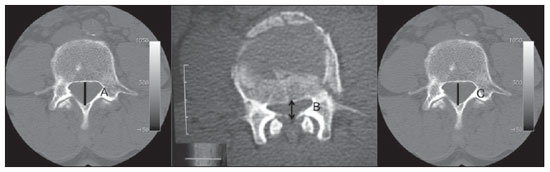
Figure 4. Calculation of anteroposterior distance of the vertebral canal. Computed tomography of vertebral spine demonstrating the anteroposterior diameter of the vertebral canal at the level of the fractured segment (B) and of the vertebral canal at the superior and inferior levels (A and C, respectively). The mean diameter of the vertebral canal at the level of the immediately superior and immediately inferior vertebras was calculated by subtraction from the diameter of the vertebral canal at the level of the fracture, on the average between the vertebral canal diameters of the superior and inferior segments, multiplied by 100, according to the following formula: {(A+C)/2 – B}/(A+C)/2 × 100. Example: A = 4 cm, B = 2 cm, C = 4 cm; so, {(4+4)/2 – 2}/(4+4)/2 = 2/4 = 50%.
At CT, it is also possible to evaluate the presence or not of laminar fracture, which may be related to the severity of the trauma and associated with a higher risk for neurological involvement (Figure 5)(10).

Figure 5. Lamina fracture. Axial computed tomography section demonstrating burst fracture of the last dorsal vertebra. Lamina fracture is highlighted at left (arrow).
There remains considerable difficulty in determining the best treatment for thoracolumbar burst fractures, generating debate in several medical schools. Because of such uncertainty, some authors have created instability criteria based on objective measurements to support the indication of the most appropriate treatment.
In the present article, the authors describe the main radiological methods and findings both at radiography and computed tomography, justifying the relevance of the utilization of objective measurements for both medical first responders and spine surgery specialists. Based on such standardization, the radiologists will be able to adopt such criteria in their reports, in practice, contributing to the indication of the treatment for these patients, since lesions considered as stable are likely to be conservatively treated with the use thoracolumbosacral orthoses, and fractures considered as unstable require surgery for stabilization with pedicle screws.
The measurement of the degree of interpedicular widening on PA radiographs is extremely relevant for allowing a correct classification of burst fractures (Denis classification for involvement of middle and anterior columns) which require greatest care and enhanced radiological investigation by means of computed tomography. In 1992, Mumford et al. described a direct relation between percentage of vertebral canal compromise and interpedicular widening visualized at plain anteroposterior radiography, suggesting that the interpedicular widening occurs in burst fractures. Such data is extremely relevant for the medical first responder because, after the identification of interpedicular widening in the fracture, its classification changes from wedge fracture to burst fracture, requiring enhanced care with the patient(7).
On the other hand, the degree of interspinous widening, also measured at PA radiography, indirectly evaluates the risk for severe posterior ligament injury, which might change the classification of the fracture from burst fracture to flexion/distraction fracture, determining the type of treatment to be adopted. The most utilized method for measuring interspinous widening is the one proposed by Neumann(13), considering a widening > 7 mm as pathological. Also, an interpedicular widening > 20% can be utilized as a reference value, as already reported in the literature(13). Magnetic resonance imaging is the gold standard for the diagnosis of posterior ligament injury, but this method is not widely available in many hospitals.
The evaluation of the intracanal fragment percentage is extremely important, since the degree of compromise may lead or not neurological involvement, directly depending on the percentage of decrease in the vertebral canal width. According to Meves & Avanzi, the neurological conditions of patients with burst fracture were directly associated with vertebral canal narrowing( 15). Trafton & Boyd(12) have reported that thoracolumbar spine fractures with narrowing of the middle-sagittal diameter = 50% resulting from retropulsed fragments associated with lamina fracture present a significant risk for neurological deficit.
Lamina fracture is other finding evaluated at computed tomography. Such a finding suggests that the impact of the trauma was distributed among the three columns, so increasing the probability of neurological involvement(5). Tisot & Avanzi(10) have observed that the mean percentage of vertebral canal narrowing caused by the presence of bone fragments was significantly higher in cases of association with lamina fracture. Such finding has represented an important data to be investigated at computed tomography (Figure 5) because of the association between lamina fracture and dural tears.
CONCLUSION
The authors highlight the extreme relevance of the radiologists' knowledge of the main criteria e measurements utilized by spine surgeons, as well as on the adoption of such data in the determination of treatment for thoracolumbar burst fractures, allowing their inclusion in the radiological workup and routine radiological reports.
REFERENCES
1. Holdsworth F. Fractures, dislocations and fracture- dislocations of spine. J Bone Joint Surg Br. 1963;45:6–20.
2. Avanzi O, Meves R, Caffaro MFS, et al. Correlação entre a abertura interpedicular e o comprometimento do canal vertebral na fratura toracolombar em explosão. Coluna. 2008;7:361–6.
3. Vaccaro AR, Kim DH, Brodke DS, et al. Diagnosis and management of thoracolumbar spine fractures. J Bone Joint Surg. 2003;85:2456–70.
4. Kim NH, Lee HM, Chun IM. Neurologic injury and recovery in patients with burst fracture of the thoracolumbar spine. Spine. 1999;24:290–3.
5. Vaccaro AR, Nachwalter RS, Klein GR, et al. The significance of thoracolumbar spinal canal size in spinal cord injury patients. Spine. 2001;26:371–6.
6. McDonough PW, Davis R, Tribus C, et al. The management of acute thoracolumbar burst fractures with anterior corpectomy and Z-plate fixation. Spine. 2004;29:1901–8.
7. Mumford J, Weinstein JN, Spratt KF, et al. Thoracolumbar burst fractures. The clinical efficacy and outcome of nonoperative management. Spine. 1993;18:955–70.
8. Wood K, Buttermann G, Mehbod A, et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit. A prospective, randomized study. J Bone Joint Surg Am. 2003;85-A:773–81.
9. McCormack T, Karaikovic E, Gaines RW. The load sharing classification of spine fractures. Spine. 1994;19:1741–4.
10. Tisot RA, Avanzi O. Fratura da coluna vertebral tipo explosão na área da cauda eqüina: correlação entre função neurológica e alterações estruturais no canal vertebral. Acta Ortop Bras. 2008;16:85–8.
11. Willén J, Lindahl S, Nordwall A. Unstable thoracolumbar fractures. A comparative clinical study of conservative treatment and Harrington instrumentation. Spine.1985;10:111–22.
12. Trafton PG, Boyd CA Jr. Computed tomography of thoracic and lumbar spine injuries. J Trauma. 1984;24:506–15.
13. Neumann P, Wang Y, Kärrholm J, et al. Determination of inter-spinous process distance in the lumbar spine. Evaluation of reference population to facilitate detection of severe trauma. Eur Spine J. 1999;8:272–8.
14. Whitesides TE Jr. Traumatic kyphosis of the thoracolumbar spine. Clin Orthop Relat Res. 1977;(128):78–92.
15. Meves R, Avanzi O. Correlation among canal compromise, neurologic deficit, and injury severity in thoracolumbar burst fractures. Spine. 2006;31:2137–41.
1. Orthopedist and Traumatologist, Specialist in Vertebral Spine Surgery, Physician Assistant, Group of Vertebral Spine – Hospital Vila Velha and Santa Casa de Misericórdia de Vitória, Vitória, ES, Brazil.
2. Radiologist, Musculoskeletal System Specialist, Chief Physician, Centro de Diagnóstico por Imagem (Center of Imaging Diagnosis), Vitória, ES, Brazil.
3. Master, Fellow PhD degree in Physiological Sciences, Physiotherapist, Group of Vertebral Spine – Santa Casa de Misericórdia de Vitória, Vitória, ES, Brazil.
4. Trainee of Musculoskeletal Radiology, Centro de Diagnóstico por Imagem, Vitória, ES, Brazil.
5. Orthopedist and Traumatologist, Specialist in Vertebral Spine Surgery, Physician Assistant, Group of Vertebral Spine – Hospital Meridional and Santa Casa de Misericórdia de Vitória, Vitória, ES, Brazil.
6. PhD of Health Sciences, Orthopedist, Specialist in Vertebral Spine Surgery, Chief Physician, Group of Vertebral Spine – Santa Casa de Misericórdia de Vitória, Hospital Meridional and Hospital Vila Velha, Vitória, ES, Brazil.
Mailing Address:
Dr. Rodrigo Rezende
Rua Desembargador Augusto Botelho, 209/801, Praia da Costa
Vila Velha, ES, Brazil, 29101-110
E-mail: grupodecoluna@santacasavitoria.org
Received July 5, 2011.
Accepted after revision January 27, 2012.
Study developed at Hospital Universitário da Santa Casa de Misericórdia de Vitória, Vitória, ES, Brazil.
 Vol. 45 nº 2 - Mar. / Apr. of 2012
Vol. 45 nº 2 - Mar. / Apr. of 2012