Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 45 nº 1 - Jan. /Feb. of 2012
Vol. 45 nº 1 - Jan. /Feb. of 2012
|
ORIGINAL ARTICLE
|
|
Patient preferences toward colon cancer screening: a comparison between computed tomography colonography and conventional colonoscopy |
|
|
Autho(rs): Marcos Vinicius Alvim Soares Maia1; Augusto Castelli von Atzingen2; Dario Ariel Tiferes3; Sarhan Sydney Saad4; Elisabeth Deak5; Delcio Matos6; Giuseppe D’Ippolito7 |
|
|
Keywords: Colonoscopy; Virtual colonoscopy; Computed tomography colonography; Computed tomography; Patients’ preference; Patients’ satisfaction. |
|
|
Abstract: INTRODUCTION
The detection and consequential resection of early-stage colorectal carcinomas or precursor adenomatous lesions may considerably reduce morbidity and mortality from colorectal cancer; nevertheless, the levels of colorectal cancer screening adherence among the general population still remain below the desirable rates(1—3). Although the screening coverage has grown in the period between 1987 and 1992(4), the adherence to the guidelines adopted by the main clinical societies is still very far from being satisfactory(5). It is known that the success of a screening program fundamentally depends on socioeconomic factors, on the acceptance by both the medical community and the population, besides the adoption of effective public policies(6—9). On the other hand, new advanced technology strategies may determine either an acceptance or non-acceptance of the screening program by the target-population based on the perception regarding costs and some procedure-related discomfort(6). Most commonly, fecal occult blood testing, sigmoidoscopy, barium enema, and colonoscopy are utilized for detection of colorectal polyps and carcinomas(2). Either colonoscopy or barium enema can be performed for a complete colon study. Colonoscopy is more effective than barium enema in the detection of polyps and, additionally allows the performance of biopsy and removal of suspected lesions(4). However, colonoscopy is an invasive method and presents some disadvantages such as pain and discomfort reported by patients, frequently requiring sedation and analgesia. Additionally, colonoscopy is associated with a risk of perforation (although it is small — up to 0.9%)(4), and possibility of difficulty in advancing the scope, with consequential failure in visualizing the entire colon in 5% to 15% of patients (the so called incomplete colonoscopy)(5). In the last decades, computed tomography colonography (CTC) or virtual colonoscopy has emerged as an alternative to optical colonoscopy in the colorectal carcinoma screening, and has recently been adopted by several medical societies(8). CTC is a tomographic study based on multiple thin axial sections producing two-dimensional and three-dimensional images including endoluminal views of the colon similar to those obtained by colonoscopy(9). It is a rapid and effective procedure (generally it takes less than ten minutes to be completed), in addition to its reproducibility and high accuracy, being well tolerated by the patients, since it does not require the use of drugs to be performed, and is minimally invasive utilizing only rectal probing and air insufflation(10—12). The patient does not undergo any kind of sedation and can return to his/her daily activities immediately after the procedure completion(7). In the last decade, CTC has been introduced and progressively adopted for colorectal cancer screening and in cases of patients with incomplete colonoscopy, with promising results still to be widely publicized. Considering that the CTC sensitivity for detecting polyps > 6 mm is similar to that of colonoscopy(10) and that the inherent complications rate is lower(9), a significant factor of adherence to CTC would be its acceptance by the patient as this method is more easily tolerated than the other diagnostic methods, such as colonoscopy. Thus CTC could be incorporated into the arsenal of diagnostic tools for colorectal cancer screening. The pain and discomfort tolerance is intrinsically connected with sociocultural and economic factors(13), thus conclusions drawn by other studies developed in different contexts should not be fully taken as definitive. In the Brazilian literature no data is found on the level of tolerance among patients submitted to CTC. The present study has proposed an evaluation of the level of acceptance and preference between CTC and colonoscopy among patients submitted to colorectal cancer screening, and considering discomfort involved in the intestinal preparation and degree of bowel distention. MATERIALS AND METHODS The present study is a secondary, prospective, cross-sectional, unicenter clinical research approved by the Committee for Ethics in Research of the authors' institution. CTC was performed in 50 patients (27 women and 23 men) with ages ranging between 36 and 82 years (mean 61.06 years), referred by the Gastroenterology Clinic, with pre-scheduled colonoscopy according to the routine of the Unit of Digestive Endoscopy, in the period from September/2010 to October/2011. All the patients responded to a specific questionnaire before and after undergoing CTC and after undergoing colonoscopy. Inclusion criteria were the following: patients aged over 18 years and under suspicion of colorectal disease. Exclusion criteria were the following: patients aged under 18 years, pregnant women, patients presenting acute diverticular disease in the last two weeks, previous colon surgery, patients without clinical conditions to undergo the required previous colon preparation and those without cognitive requirements for answering the questions. The questionnaire evaluated the bowel preparation e respective adverse effects, as well as the level of discomfort expected and experimented by the patient before and after examination, according to a 3-point scale (little discomfort, mild discomfort, and a lot of discomfort). After colonoscopy, the patient was asked to compare the discomfort from colonoscopy with that from CTC, establishing his/her preference for a determined diagnostic method. The preparation for CTC was identical to the one utilized for colonoscopy. In the night before the examination, all the patients took two bisacodyl tabs, besides 1,500 ml of water with ten macrogol sachets added of 50 ml hydrosoluble iodinated contrast agent. The bowel preparation was considered as appropriate in cases where a complete colon cleasing was achieved, with the smallest possible amount of fecal residues and fluids, thus allowing greater confidence for the radiologist and an easy browsing through the virtual colonoscopy software (Figure 1). 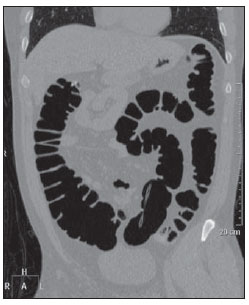 Figure 1. Coronal image reconstruction demonstrating excellent bowel distention of the whole colon frame. All the studies were performed in a 64-row multidetector helical CT equipment (Brilliance; Philips Medical Systems, Best, Netherlands) with a virtual colonoscopy software, collimation 64 × 0,625 mm, rotation time 0.5 second, 2 mm slice thickness, 1 mm reconstruction interval, pitch 1.1, low radiation dose, (120 kV e 50 mAs), covering the region from the diaphragm to the pubic symphysis. No antispasmodic or any other drugs were utilized. During the CTC scan, air was insufflated through the rectum by means of a rectal probe, according to the patient's tolerance and the image quality requirements, to achieve appropriate insufflation and bowel distention. All the images acquisitions were performed with the patients in ventral and dorsal decubitus. All the patients underwent colonoscopy immediately after CTC, with an adult videocolonoscope system (Olympus CF-VL; Olympus Optical do Brasil, São Paulo, Brazil) and under sedation (meperidine and midazolam). After colonoscopy, a new questionnaire was administered with the objective of knowing the patients' preference for either colonoscopy or the previous CTC. By analysing the variables responsible by the CTC scan quality, such as the degree of colon distention (1: no distention; 2: appropriate distention; 3: excellent distention) and the amount of residual fluid (present in more or lesser than 50% of the colon lumen), the authors sought to correlate the level of discomfort reported by the patients with their preference (Figures 2, 3 and 4). 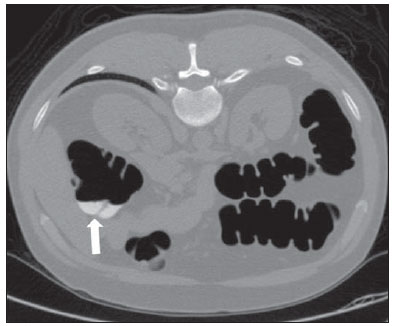 Figure 2. Patient in ventral decubitus, with presence of an amount of residual fluid in < 50% of the colon lumen (arrow). 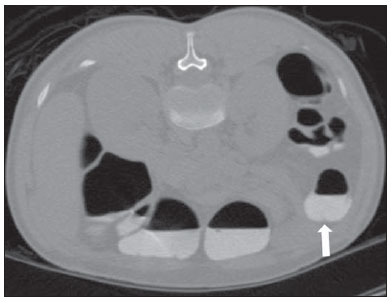 Figure 3. Image of a patient in ventral decubitus, demonstrating the presence of an amount of residual fluid in > 50% of the colon lumen (arrow). 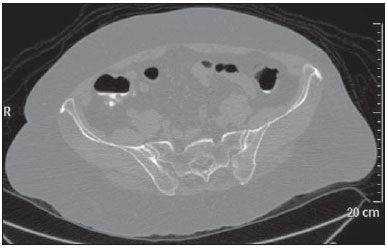 Figure 4. Example of image acquired with inappropriate distention (incomplete colon distention). Statistical analysis The categorical data were summarized in terms of absolute frequency (number of patients) and relative frequency (percentage). The changes significance was evaluated by the McNemar test for comparison of variables admitting a same type of response. The Fisher exact test was utilized to analyze the association between any two categorical variables in order to transform the data into a 2 × 2 table for the testing. Statistical significance was established for p values < 0.05. The statistical software Minitab®, version 16.1 was utilized for data analysis. RESULTS The bowel preparation was considered appropriate in 44 patients (88%). Six patients (12%) presented inappropriate bowel preparation because of no ingestion or partial ingestion of oral contrast agent. Side effects of bowel preparation were rarely observed and reported by only one patient (2.0%) who presented vomiting during the period of bowel preparation. Discomfort during CTC After undergoing colonoscopy, 36 (72%) patients reported little discomfort, 13 (26%) reported mild discomfort, and one (2%) patient reported less-than-expected discomfort, while 29 patients expected mild discomfort and during examination reported little discomfort. Sixteen patients (32%) reported that the discomfort was as expected, six of them initially expecting little discomfort and ten, mild discomfort. Only three (6%) patients reported greater-than-expected discomfort during CTC. The discomfort sensation experienced by the patients during CTC was significantly smaller than expected, according to the McNemar test (p < 0.001). Evaluation of the relation between patients' preference towards the diagnostic method and the degree of colon distention and presence of residual fluid Forty-three patients (86%) preferred CTC to colonoscopy and only six patients preferred optical colonoscopy. One of the patients (2%) did not report any preference. The patients' preference for one or other method does not seem to be related to the degree of colon distention (p = 0.999) and the residual intestinal fluid amount (p = 0.310), according to the Fisher exact test. Evaluation of the relation between experienced discomfort with CTC and colon distention and residual fluid No statistically significant relation was observed between CTC-related discomfort and the degree of colon distention (p = 0.320). Also, no statistically significant relation was observed between discomfort and residual fluid amount (p = 0.414). DISCUSSION Screening programs constitute the primary means to reduce the morbimortality associated with colorectal cancer. Colonoscopy, together with fecal occult blood testing and carcinoembryonic antigen, have been the main colorectal cancer screening tools(2). The main advantage of colonoscopy is the possibility of performing biopsy and polypectomy as necessary. Limitations are related to the higher cost as compared with other methods(8), some morbidity and the patients' apprehension and insecurity in relation to the sedation and discomfort(14,15). Additionally, despite being considered as a reference method in the detection of colon lesions, some studies in the literature have reported failure in the detection of large adenomas in up to 12% of cases(14). CTC has been proposed as a feasible alternative method, with effectiveness similar to colonoscopy and advantages related to scanning rapidity and lower invasiveness, not requiring sedation so the patient can return to his/her daily activities immediately after the procedure(8,10). Several studies have compared CTC with conventional colonoscopy in terms of patients' acceptance. A recent study demonstrated that 72% of patients submitted to CTC and colonoscopy preferred the first one(16). Another study developed in Missouri, USA, involving patients submitted to CTC and colonoscopy in a single day who responded to a questionnaire similar to the one described in the present study, reported that 68% of the patients considered CTC as a more convenient method and that it would preferred for future follow-up(17). In the literature review, the authors have found only one study reporting higher acceptance of colonoscopy(18). The reason for such a preference seems to be related to the environment where the procedures were performed, with a closer contact between staff and patients(18). In the present study, the interaction with the radiologist to clarify eventual doubts before, during and after the CTC have given the patients more confidence and security, possibly increasing the preference for CTC. A question to be considered in this type of research is the patient's awareness of the limitations of CTC in terms of biopsy and polyp resection capability as compared with colonoscopy. Thus such information could change the patients' preference, relativizing the experienced discomfort, provided that the probability of occurrence of a clinically significant colon lesion was expressive. Studies approaching colorectal cancer screening indicate a rate of detection corresponding to 5—6% for large polyps (> 10 mm), and to 8% for small polyps (6—9 mm)(15). The prevalence of advanced adenomas under the risk of malignant transformation is of 0.5%(15), i.e., probably in one in every twenty colonoscopy, polyp resection will be required. According to a recent consensus, patients with two polyps < 10 mm should undergo follow-up with CTC after three years instead of being immediately submitted to polypectomy that is recommended if large polyps (> 10 mm) or three small polyps are present(19). In the present study, the authors could establish the patients' preference towards CTC, despite the relatively small size of the sample that should be expanded in further studies. Additionally to the small size of the sample, the study presents other limitations, as follows: a) the evaluation is subjective and may be influenced by the researcher, which the authors managed to avoid by allowing the patients to answer the questions by their own handwriting; b) the closeness between the radiologist involved in the research and the patient during the several phases of the study may have contributed to generate empathy and a tendency to consider the CTC more comfortable. On the other hand, the present results have demonstrated that the patients' preference is not connected with the colon distention at CTC and the efficiency of bowel preparation. The fact that the air insufflation was carefully done, not exceeding the patient's tolerance, but not compromising the quality of the diagnostic evaluation, must have contributed to this result. The bowel preparation was effective in most of the cases (88%), with rare side effects, being well tolerated by the patients. CONCLUSION The results of the present study allow us to conclude that the patients prefer CTC to colonoscopy and that there is no statistical relationship between colon distention, quality of bowel preparation (residual fluid) and the patient's preference or degree of discomfort. CTC may be considered as an alternative to diagnostic colonoscopy, with advantages related to the convenience and acceptance of the method by the patients. REFERENCES 1. Brasil. Ministério da Saúde. Instituto Nacional de Câncer. Estimativa 2010: incidência de câncer no Brasil. Rio de Janeiro, RJ: INCA; 2009. 2. Levin B, Lieberman DA, McFarland B, et al. Screening and surveillance for the early detection of colorectal cancer and adenomatous polyps, 2008: a joint guideline from the American Cancer Society, the US Multi-Society Task Force on Colorectal Cancer, and the American College of Radiology. CA Cancer J Clin. 2008;58:130—60. 3. Weitzman ER, Zapka J, Estabrook B, et al. Risk and reluctance: understanding impediments to colorectal cancer screening. Prev Med. 2001;32:502—13. 4. Winawer SJ, Stewart ET, Zauber AG, et al. A comparison of colonoscopy and double-contrast barium enema for surveillance after polypectomy. National Polyp Study Work Group. N Engl J Med. 2000;342:1766—72. 5. Lieberman DA. Cost-effectiveness model for colon cancer screening. Gastroenterology. 1995;109:1781—90. 6. Vernon SW. Participation in colorectal cancer screening: a review. J Natl Cancer Inst. 1997;89:1406—22. 7. Pickhardt PJ, Choi JR, Hwang I, et al. Computed tomographic virtual colonoscopy to screen for colorectal neoplasia in asymptomatic adults. N Engl J Med. 2003;349:2191—200. 8. Cummings LC, Cooper GS. Colorectal cancer screening: update for 2011. Semin Oncol. 2011;38:483—9. 9. von Wagner C, Smith S, Halligan S, et al. Patient acceptability of CT colonography compared with double contrast barium enema: results from a multicentre randomised controlled trial of symptomatic patients. Eur Radiol. 2011;21:2046—55. 10. Graser A, Stieber P, Nagel D, et al. Comparison of CT colonography, colonoscopy, sigmoidoscopy and faecal occult blood tests for the detection of advanced adenoma in an average risk population. Gut. 2009;58:241—8. 11. Svensson MH, Svensson E, Lasson A, et al. Patient acceptance of CT colonography and conventional colonoscopy: prospective comparative study in patients with or suspected of having colorectal disease. Radiology. 2002;222:337—45. 12. Leard LE, Savides TJ, Ganiats TG. Patient preferences for colorectal cancer screening. J Fam Pract. 1997;45:211—8. 13. Winawer SJ, Fletcher RH, Miller L, et al. Colorectal cancer screening: clinical guidelines and rationale. Gastroenterology. 1997;112:594—642. 14. Heresbach D, Barrioz T, Lapalus MG, et al. Miss rate for colorectal neoplastic polyps: a prospective multicenter study of back-to-back video colonoscopies. Endoscopy. 2008;40:284—90. 15. Pickhardt PJ, Kim DH. Colorectal cancer screening with CT colonography: key concepts regarding polyp prevalence, size, histology, morphology, and natural history. AJR Am J Roentgenol. 2009;193:40—6. 16. von Wagner C, Knight K, Halligan S, et al. Patient experiences of colonoscopy, barium enema and CT colonography: a qualitative study. Br J Radiol. 2009;82:13—9. 17. Ristvedt SL, McFarland EG, Weinstock LB, et al. Patient preferences for CT colonography, conventional colonoscopy, and bowel preparation. Am J Gastroenterol. 2003;98:578—85. 18. Akerkar GA, Yee J, Hung R, et al. Patient experience and preferences toward colon cancer screening: a comparison of virtual colonoscopy and conventional colonoscopy. Gastrointest Endosc. 2001;54:310—5. 19. Zalis ME, Barish MA, Choi JR, et al. CT colono graphy reporting and data system: a consensus proposal. Radiology. 2005;236:3—9. 1. MD, Radiologist, Trainee at the Unit of Imaging Diagnosis, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 2. MD, Radiologist, Fellow PhD degree of Clinical Radiology, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 3. PhD, MD, Radiologist, Collaborator at Department of Imaging Diagnosis, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 4. Associate Professor, Division of Surgical Gastroenterology, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 5. MD, Assistant at Division of Surgical Gastroenterology, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 6. Full Professor, Division of Surgical Gastroenterology, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. 7. Private Docent, Department of Imaging Diagnosis, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. Mailing Address: Dr. Giuseppe D'Ippolito Rua Professor Filadelfo Azevedo, 617, ap. 61, Vila Nova Conceição São Paulo, SP, Brazil, 04508-011 E-mail: giuseppe_dr@uol.com.br Received December 20, 2011. Accepted after revision January 17, 2012. Study developed at Department of Imaging Diagnosis, Universidade Federal de São Paulo (Unifesp), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554