INTRODUCTION
Osteoid osteoma is a small and relatively common benign bone tumor, with well defined clinical, radiological and pathological characteristics(1—3). It is most prevalent in the 10-25 year old age group. Most patients present the classical bone pain symptom that worsens at night and improves with the use of aspirin or other non-steroidal anti-inflammatory drugs. Diaphysis and metaphysis of long bones, particularly the femur and tibia constitute the most common sites of osteoid osteomas.
In cases of intra-articular involvement, the clinical manifestations are nonspecific and the radiographic findings may be subtle, becoming a diagnostic challenge. Patients with osteoid osteoma of the elbow frequently present pain, chronic synovitis, joint effusion, limitation in range of motion and flexion contracture simulating inflammatory arthropathy. At radiography, reactive sclerosis may be minimal or absent, leading to a significant delay in the diagnosis or even to misdiagnosis(4—6).
The present study is aimed at highlighting clinical and radiological findings which allow early diagnosis and appropriate management in cases of osteoid osteoma of the elbow.
MATERIALS AND METHODS
In the databanks of the Sarah hospitals in the cities of Brasília, DF, and Belo Horizonte, MG, Brazil, 142 patients with histologically confirmed diagnosis of osteoid osteoma were identified. Among them, seven patients presenting elbow lesions were selected and had their records and imaging studies reviewed.
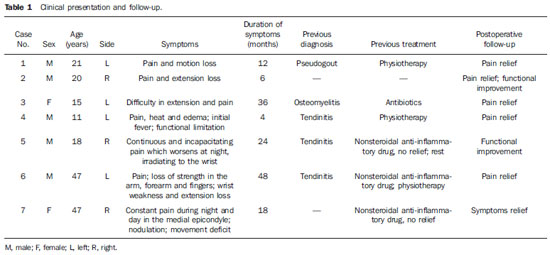
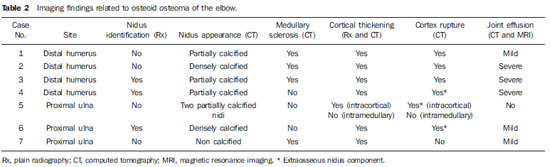
The following clinical data were collected: sex, age, affected side, presence of pain, fever, edema, functional limitation, symptoms duration, previous diagnoses and treatments, and response to use of nonsteroidal anti-inflammatory drugs and surgical treatment (Table 1).
All the seven patients were submitted to plain radiography and computed tomography (CT). Three patients were also underwent magnetic resonance imaging (MRI) in a 1.5 T equipment. The radiographs were utilized to evaluate the presence of nidus, sclerotic halo, cortical thickening and periostitis. Appearance and location of the nidus, sclerosis signs, cortical thickening and rupture, besides the presence of joint effusion, were analyzed at CT. MRI was useful in the assessment of changes in signal intensity in the bone marrow, identification of the nidus, presence of joint effusion, synovitis and abnormalities in adjacent soft tissues. The imaging findings are described on Table 2.
The study was approved by the Committee for Ethic in Research of the Institution.
RESULTS
Out of a total of 142 patients diagnosed with osteoid osteoma, seven (4.9%) presented lesions in the elbow. Five of these patients were male, and two were female (2.5:1 ratio), with ages ranging between 11 and 47 years (mean = 25 years). The distal humerus was affected in four cases while the proximal ulna was affected in three cases, and four cases involved the left elbow and three, the right elbow. Pain and limitation in the range of motion were the most common symptoms, found in all analyzed cases. One patient also presented fever, articular heat and joint edema.
Among the seven studied patients, five (71.4%) had previously received other clinical diagnosis. The previously raised diagnostic hypotheses were the following: tendinitis (three patients), pseudogout (one patient) and osteomyelitis (one patient). The mean duration of symptoms was 21 months. The previous treatments consisted of utilization of non-steroidal anti-inflammatory drugs for three patients, without symptoms relief in two of them; physiotherapy for two patients; and use of antibiotics in one case.
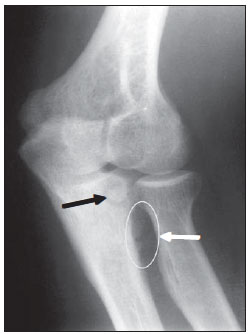
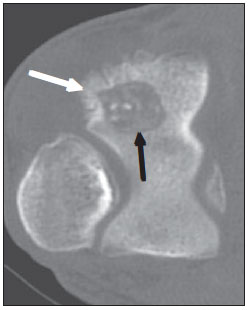
The radiographic studies demonstrated periosteal reaction and/or variable cortical thickening in all of the patients (Figure 1) but could not demonstrate the nidus in three of the patients (42.8%). CT clearly demonstrated the nidus and bony reaction in all analyzed cases (Figure 2). Cortical bone rupture was identified in six of the seven patients, and in three of those patients there was protrusion through the cortex with extraosseous component of the nidus (Figure 3). Two nidi were identified in one patient (Figure 4). As regards mineralization pattern within the eight nidi, calcification/ossification was absent in one case, was partial in five cases and dense in two cases (Figure 5). MRI could demonstrate the nidus, joint effusion, synovitis, bone edema and soft tissue edema in the three patients (cases 1, 2, and 4) who underwent such an examination (Figure 6). The effusion present in six patients was considered as mild in three cases and severe in the other three cases (Figure 3).
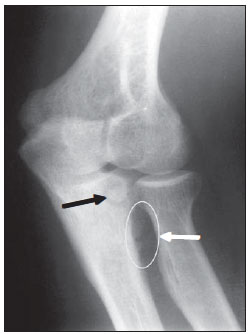
Figure 1.
Case 6. Radiography of left elbow – oblique view demonstrating the presence of periostitis (circle and white arrow) adjacent to the nidus (black arrow) located in the proximal ulna.
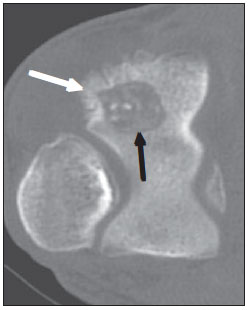
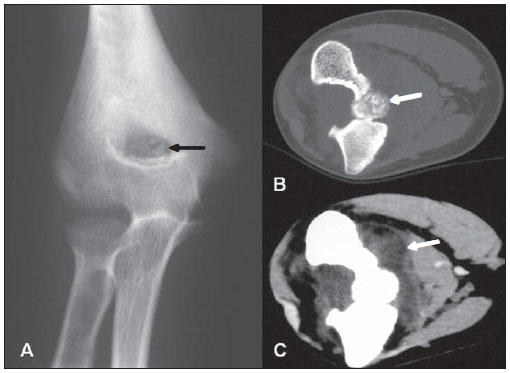
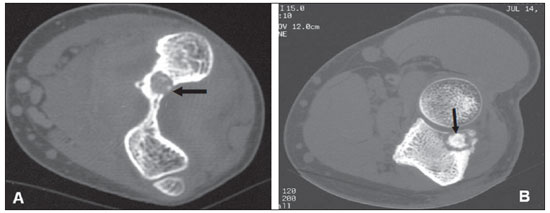
Figure 2.
Case 1. Axial computed tomography depicting osteolytic nidus (black arrow) including calcification foci, in association with periostitis (white arrow) in the posterolateral region of the distal humerus.
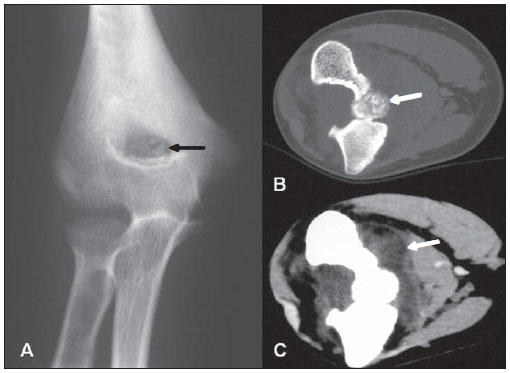
Figure 3.
Case 3. A: Radiography of left elbow – anteroposterior view depicting a partially calcified nidus (arrow) in the humerus coronoid fossa. B: Axial tomographic section with bone window showing the nidus (arrow) protruding on the ventral aspect of the humerus. C: Image in the same plane with soft tissue window demonstrating association with significant joint effusion (arrow).

Figure 4.
Case 5. Axial tomographic section revealing the presence of two nidi in the proximal ulna, one intramedullary (black arrow) and the other protruding through a cortex rupture (white arrow). Note the presence of minute medullary sclerosis adjacent to the lesion.
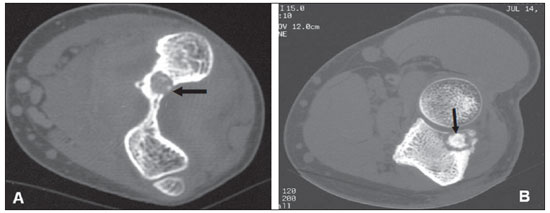
Figure 5. Nidus appearance at tomography. A: Partially calcified osteolytic lesion (arrow), smaller than 1 cm, adjacent to the olecranon fossa. B: Nidus located in the proximal ulna, including a densely calcified central focus surrounded by a hypodense halo (arrow).
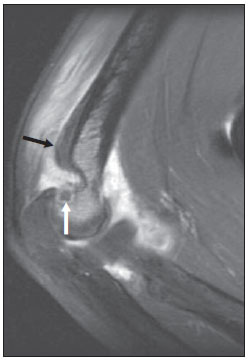
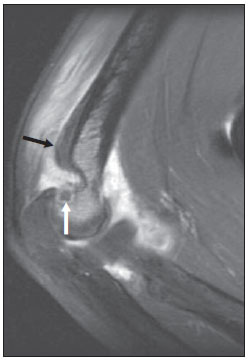
Figure 6.
Case 2. Sagittal, contrast-enhanced MRI T1-weighted s with fat saturation demonstrating a hypointense nidus (white arrow), medullary edema and edema in the triceps muscle, besides significant thickening and synovial enhancement. The solid periosteal reaction (black arrow) at the posterior margin of the distal metaphysis of the humerus occurs far from the nidus since the periosteum is not present within the articular capsule.
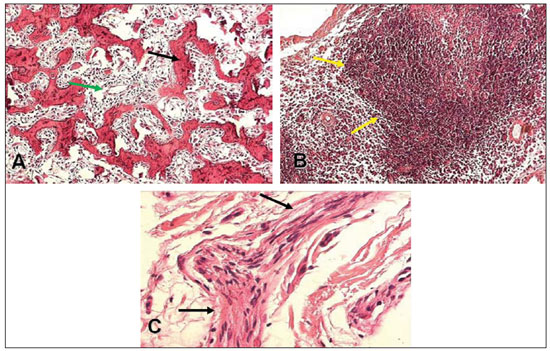
The histological diagnosis was based on the classical signs of an interwoven network of osteoid trabeculae with variable degrees of mineralization, consistent with nidus, surrounded by osteoblasts and some osteoclasts intermingled with highly vascularized mixed connective tissue (Figure 7A). The analysis of the synovial tissue demonstrated diffuse edema and focal mononuclear perivascular inflammatory cell infiltrate. In some cases, such infiltrate was dense and was associated with the presence of lymphoid follicles (Figure 7B). In one patient, prominent focal nerve fibers were found as part of the adjacent soft tissue reaction (Figure 7C).
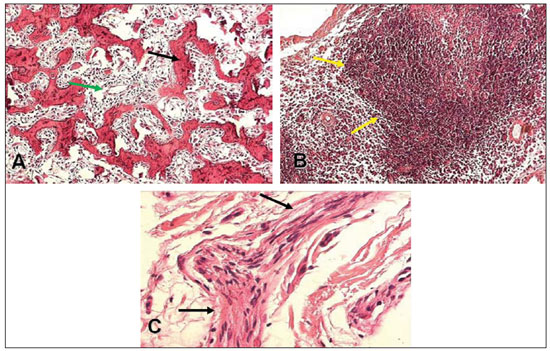
Figure 7. Histological sections. A: Nidus. Interwoven network of osteoid trabeculae (black arrow), intermingled with richly vascularized loose connective tissue (green arrow) – hematoxylin-eosin staining, 4× magnification. B: Follicular synovitis. Synovial tissue containing dense inflammatory mononuclear infiltrate, with development of lymphoid follicles (arrows) – hematoxylin-eosin staining, 10× magnification. C: Prominent peripheral nerve (arrows) in soft tissues adjacent to the osteoid osteoma nidus – hematoxylin-eosin staining, 10× magnification.
All the patients were submitted to open surgery with nidus resection, with symptom relief and/or functional improvement in all cases. The patients who presented the best degree of joint motion recovery were those whose symptoms duration was less than one year from admission. However, the patient who experienced symptoms for two years also presented significant improvement after the surgical treatment.
DISCUSSION
Osteoid osteoma is a relatively common bone lesion, corresponding to 10—12% of the benign bone tumors(7,8). It generally affects young individuals in the age range from 10 to 25 years, with 90% of the cases occurring between 5 and 30 years of age, with a mean of 21 years(9). Men are more frequently affected than women (2:1 to 4:1 ratio).
Although it has been first described by Bergstrand in 1930, the term osteoid osteoma was introduced in the medical literature in 1935 by Jaffe who, based on the study of five cases, described such condition as a specific pathological entity(10).
The tumor may occur in almost all bones of the body; however the long bones are the site of origin in more than 70% of cases, with the femur and the tibia being most commonly affected (50—60%). In long bones, osteoid osteomas are usually located in the diaphysis or in the metaphysis. The epiphyseal and intra-articular locations are rarely observed(11), although some authors estimate their prevalence to be between 10% and 13%(6,9), the hip being the most common location. Ankle, elbow, wrist and knee are other less affected locations. The lesion is considered to be intra-articular in cases where it occurs at the extremity of long bones, around or within the joint, in a bone limited by the capsule, very close to it and to the synovia.
The etiology of this condition is unknown. Cytogenetic changes such as chromosome 22q deletion have been described in cases of osteoid osteoma(12), but further studies are necessary to definitively link such an entity to a clonal mutation. Familial occurrence is extremely rare. In a study developed in the authors' institution(3), osteoid osteoma was described in two brothers that had the same age when the symptoms onset led them to seek medical assistance. Both of them also had the lesion located in proximal femoral cortex (the most common site). Such findings suggest the presence of an associated genetic factor.
Immunohistochemical studies of neuronal antigens and associated with nerves have demonstrated that osteoid osteomas present nervous fibers in the reactive zone. Their innervation seems to be unique among bone tumors(13). The clinical symptom of intense pain in the affected area which worsens at night and in general improves after 30 minutes with the use of salicylates is present in 75% of the cases and suggests the diagnosis. The pain seems to be mediated by high levels of E2 prostaglandins released by the tumor which are inhibited by the use of non-hormonal anti-inflammatory drugs. The prominent focal nerve fibers found in the region of adjacent soft tissue reaction in one patient might be related to the disproportionate pain reported by such patient. This is in agreement with the previous description of nerves found in the peritumor tissue in a case of osteoid osteoma. In the intra-articular presentation, the response to utilization of nonsteroidal anti-inflammatory drugs for pain relief seems to be less effective than in the extra-articular presentation. Such a fact was observed in two of the three patients in the present study who utilized such type of drug.
The tumor presents a limited growth potential and a tendency toward spontaneous maturation in two to five years as the pain tends to decrease. The lesion can spontaneously regress, but the mechanism of such regression is not yet known.
Plain radiography is the imaging method utilized for initial evaluation. In cases of osteoid osteoma, the classical radiographic finding consists of a round or ovoid lytic lesion, called nidus (or nest), smaller than 2.0 cm, normally measuring 5 to 10 mm, in association with an area of bone sclerosis and/or reactive cortical thickening(14). Such finding may vary according to the affected bone, to the tumor site, symptom duration and the patient's age. The nidus may be uniformly radiolucent or including a variable amount of calcification/ossification. Bone maturation is more pronounced in lesions with a longer evolution.
The diagnosis is not difficult in cases where the typical clinical and radiographic findings are present. However, tumor presentation in unusual locations, like the intra-articular presentation, may be associated with atypical manifestations that compromise the diagnosis.
Osteoid osteoma can be classified into three types as follows: cortical, medullary and subperiosteal. Intra-articular tumors are normally of the medullary and subperiosteal types, which contributes to the absence or presence of limited sclerosis around the nidus, making its identification difficult at radiography.
Thin-section (0.5 to 2.0 mm) computed tomography and multiplanar reconstructions utilizing bone window is the method of choice to confirm the benign nature of bone reaction and to identify the nidus, particularly in cases where it is occult at radiography (Figure 8). CT is also very useful in cases where there is a suspicion of residual lesion. However, such a technique has the inconvenience of exposing the patient to ionizing radiation.

Figure 8. Case 1. A,B: Lateral and anteroposterior radiography of left elbow cannot demonstrate the nidus. C,D: Tomographic reconstructions in the sagittal and coronal planes of a single patient clearly demonstrate the lesion (arrows).
The role of MRI in the evaluation of osteoid osteoma is controversial. The variable appearance of the lesion, extensive reactional changes in the bone marrow and in soft tissues may simulate a more aggressive lesion or one of a different nature(15), though such was not the impression of the authors on the three MRI studies. Based on the hypervascularization of the nidus, the dynamic study with gadolinium combined with high resolution images increases the nidus conspicuity, moreover in cases where the lesion is located in an atypical site and in those patients presenting with nonspecific clinical symptoms(16—18).
Bone scintigraphy utilizing technetium-99 presents a high sensitivity in the diagnosis of osteoid osteomas. The tumor presents a typical pattern known as "double-density" sign. Such a sign is characterized by intense activity/hyper-uptake centrally in the nidus region and less intense accumulation of the radioisotope in the periphery of the lesion, where the reactive sclerotic bone and perilesional edema are located. However, many times such sign is absent in cases of intra-articular lesions, as a generalized increase activity increase within the joint due to the presence of synovitis associated with osteoporosis and hyperemia.
In the literature, there are few reports on osteoid osteoma of the elbow, describing tumors in the head and tuberosity of the radius, in the olecranon and coronoid process of the ulna, in the capitulum and olecranon fossa of the humerus.
The intra-articular lesion is associated with pain, soft tissue edema and joint effusion. Synovitis may be intense and the patient may present with articular rigidity. Six out of the seven patients presented joint effusion. Osteopenia, uniform reduction of the articular space and osteo-hypertrophic changes may be observed(9). Clinically and radiologically, the condition may simulate a primary articular process resulting in diagnosis delay of months or even years. Patients presenting intra-articular lesion may progress with signs of osteoarthrosis secondary to synovitis and synovial proliferation with cartilage destruction. Muscle atrophy may affect the limb, particularly in the case of long-lasting tumors.
The differential diagnoses for osteoid osteoma of the elbow include: (inflammatory/infectious) monoarthritis, nonspecific synovitis, tendinitis/epicondylitis, osteochondritis dissecans, osteomyelitis/Brodie's abscess, eosinophilic granuloma, enostosis, stress fracture, chondroblastoma and osteoblastoma. Osteoid osteoma and osteoblastoma have the same histopathological characteristics; but osteoblastoma is larger than 2.0 cm, presents growth progression and tends to be more aggressive.
The results of the present study, in agreement with those from previous studies(5), show that the radiographic findings of sclerosis, cortical thickening and subtle periosteal reaction in elbow bones in association with the presence of joint effusion should raise the possibility of osteoid osteoma.
Complete nidus excision is curative and is the most traditional treatment method. However, minimally invasive techniques have been utilized as equally safe and effective alternatives for the treatment of osteoid osteomas, with low morbidity rates and faster recovery. Radiofrequency ablation is the most prominent of such techniques; alternating current radiofrequency is transmitted by means of an electrode needle positioned in the nidus, producing heat and causing irreversible cell damage/necrosis by means of thermal coagulation(19). Aiming at symptoms relief and functional improvement of their patients, the authors of the present study have opted for open surgery. Such an option was based on the difficulties in the preoperative diagnosis, on the raised hypotheses, as well as on the surgeon's experience. Additionally, the authors highlight the scarcity of reports on cases of osteoid osteoma of the elbow in the literature to guide them towards a specific treatment modality that might be adopted as a treatment standard.
CONCLUSION
Osteoid osteoma is a rare cause of elbow pain. The diagnosis of this tumor is difficult as, generally, the clinical manifestations and radiographic findings are not characteristic. It is important to consider the possibility of osteoid osteoma in young adult patients with pain, limitation of movement and signs of synovitis in the elbow with unknown etiology, refractory to conservative treatment and not related to systemic disease. CT is the imaging method of choice for identification of the nidus. The early diagnosis allows appropriate surgical treatment, reducing the related morbidity.
Acknowledgements
To Rede Sarah de Hospitais de Reabilitação, for the institutional support. To Drs. Antônio Lopes da Cunha Júnior, Sandra Alvarenga Coutinho Passos, Maria Henriqueta Freire Lyra, Jorge Henrique Calil and to the histology technician Cleides Campos de Oliveira, for their contribution in the present study.
REFERENCES
1. Fletcher CDM, Unni KK, Mertens F, editors. World Health Organization Classification of Tumours. Pathology & genetics. Tumours of soft tissue and bone. Lyon, France: IARC Press; 2002.
2. Picci P, Mirra JM. Osteoid osteoma. In: Mirra JM, editor. Bone tumors. Philadelphia, PA: Lea & Febiger; 1989. p. 226—48.
3. Kalil RK, Antunes JS. Familial occurrence of osteoid osteoma. Skeletal Radiol. 2003;32:416—9.
4. Weber KL, Morrey BF. Osteoid osteoma of the elbow: a diagnostic challenge. J Bone Joint Surg Am. 1999;81:1111—9.
5. Moser RP Jr, Kransdorf MJ, Brower AC, et al. Osteoid osteoma of the elbow. A review of six cases. Skeletal Radiol. 1990;19:181—6.
6. Szendroi M, Köllo K, Antal I, et al. Intraarticular osteoid osteoma: clinical features, imaging results, and comparison with extraarticular localization. J Rheumatol. 2004;31:957—64.
7. White ML, Kandel R. Osteoid-producing tumors of bone. Semin Musculoskelet Radiol. 2000;4:25—43.
8. Dahlin DC, Unni KK. Bone tumors: general aspects and data on 8,542 cases. 4th ed. Springfield, IL: Thomas; 1987.
9. Allen SD, Saifuddin A. Imaging of intra-articular osteoid osteoma. Clin Radiol. 2003;58:845—52.
10. Jaffe HL. "Osteoid osteoma". A benign osteoblastic tumor composed of osteoid and atypical bone. Arch Surg. 1935;31:709—28.
11. Resnick D, Kyriakos M, Greenway GD. Tumors and tumor-like lesions of bone: imaging and pathology of specific lesions. In: Resnick D, Kransdorf MJ, editors. Bone and joint imaging. Philadelphia, PA: Elsevier/Saunders; 2005. p. 1120—6.
12. Baruffi MR, Volpon JB, Barbieri Neto J, et al. Osteoid osteomas with chromosome alterations involving 22q. Cancer Genet Cytogenet. 2001;124:127—31.
13. O'Connell JX, Nanthakumar SS, Nielsen GP, et al. Osteoid osteoma: the uniquely innervated bone tumor. Mod Pathol. 1998;11:175—80.
14. Cassard X, Accadbled F, De Gauzy JS, et al. Osteoid osteoma of the elbow in children: a report of three cases and a review of the literature. J Pediatr Orthop B. 2002;11:240—4.
15. Davies M, Cassar-Pullicino VN, Davies AM, et al. The diagnostic accuracy of MR imaging in osteoid osteoma. Skeletal Radiol. 2002;31:559—69.
16. Liu PT, Chivers FS, Roberts CC, et al. Imaging of osteoid osteoma with dynamic gadolinium-enhanced MR imaging. Radiology. 2003;227:691—700.
17. Zampa V, Bargellini I, Ortori S, et al. Osteoid osteoma in atypical locations: the added value of dynamic gadolinium-enhanced MR imaging. Eur J Radiol. 2009;71:527—35.
18. von Kalle T, Langendörfer M, Fernandez FF, et al. Combined dynamic contrast-enhancement and serial 3D-subtraction analysis in magnetic resonance imaging of osteoid osteomas. Eur Radiol. 2009;19:2508—17.
19. Motamedi D, Learch TJ, Ishimitsu DN, et al. Thermal ablation of osteoid osteoma: overview and step-by-step guide. Radiographics. 2009;29:2127—41.
1. Specialists in Pathological Anatomy, MDs, Surgical Pathologists at Hospital Sarah, Belo Horizonte, MG, Brazil.
2. Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MD, Radiologist at Hospital Sarah, Belo Horizonte, MG, Brazil.
3. Specialist in Orthopedics and Traumatology, MD, Orthopedist at Hospital Sarah, Belo Horizonte, MG, Brazil.
4. Specialists in Pathological Anatomy, MDs, Surgical Pathologists at Hospital Sarah, Brasília, DF, Brazil.
5. Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MD, Radiologist at Hospital Sarah, Brasília, DF, Brazil.
Mailing Address:
Dr. Rogério Teles de Melo
Avenida Amazonas, 5953, Gameleira
Belo Horizonte, MG, Brazil, 30510-000
E-mail: rogeriomelo@sarah.br
Received November 6, 2011.
Accepted after revision January 11, 2012.
Study developed at Departments of Surgical Pathology, Radiology and Orthopedics – The Sarah Network of Rehabilitation Hospitals, Hospital Sarah Belo Horizonte, MG, and Hospital Sarah Brasília, DF, Brazil.
 Vol. 45 nº 1 - Jan. /Feb. of 2012
Vol. 45 nº 1 - Jan. /Feb. of 2012