INTRODUCTION
Behçet's syndrome is an inflammatory, chronic and systemic disease whose etiology remains unknown, with higher incidence in men aged between 30 and 40 years(1,2). This disease is frequently found in Mediterranean countries and in Asia, with highest prevalence in Turkey, and was characterized by Hulusi Behçet through the triad: recurrent oral, genital ulcerations and uveitis.
Manifestations in several other organs have been described, with vasculitis being the main pathological finding(1). The disease diagnosis is based on the criteria proposed by the International Study Group for Behçet's Disease(3). The prognosis is determined by the involvement of the cardiovascular, gastrointestinal and central nervous systems(2). Although the vascular compromise occurs in 25% to 30% of cases in Behçet's disease, this is the greatest cause of mortality related to the disease(4,5).
The chest involvement manifests as several findings that may be demonstrated by imaging studies. The knowledge on such findings is useful in the disease diagnosis.
The present report is aimed at describing the radiological and clinical findings observed in a case of Behçet's disease. This paper was approved by the Research Ethics Committee of the authors' institution (opinion CEP/FHEMIG: 069/2010).
CASE REPORT
A male, 30-year-old patient was referred to the authors' institution because of findings observed at chest radiography, for specialized diagnosis. The patient reported the onset of dry cough, weight loss, fever, hyporexia, adynamia and some episodes of hemoptysis for two months. Later, he presented progressive dyspnea. Additionally, he reported the presence of recurrent oral and genital ulcerations since his adolescence. At clinical examination, acneiform nodules and cicatricial lesions were observed on the patient's skin surface.
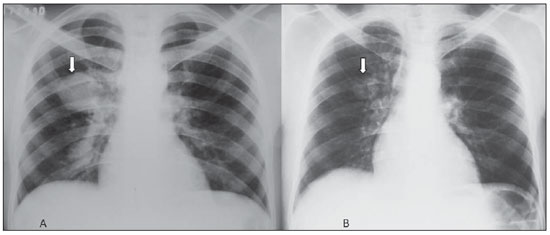
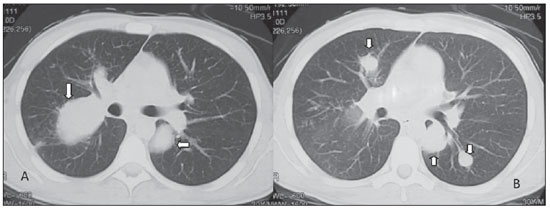
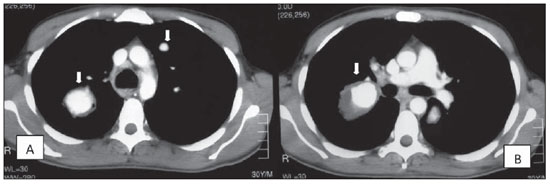
Posteroanterior chest radiography demonstrated the presence of a well defined mass with soft tissue density and regular contour in the region of the right pulmonary hilum, whose dimensions were significantly reduced after specific treatment with corticoid and immunosuppressive drugs (Figure 1). Chest computed tomography, before and after intravenous administration of iodinated contrast medium, demonstrated aneurysmal dilatation of the right interlobar artery, measuring approximately 50 mm in its greater axial axis, with diffuse contrast enhancement of the lumen, and with the presence remarkable parietal thickening (Figure 2). Other smaller aneurysmal formations with similar morphological characteristics were bilaterally observed, presenting varied sizes and predominance in central regions and in the upper and middle thirds of the lungs (Figures 1 and 3). Anatomical alterations were not observed in the mediastinal region.
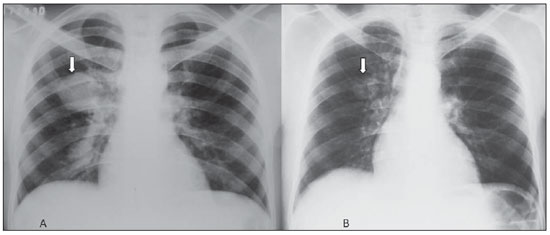
Figure 1. Posteroanterior chest radiographs demonstrating a hilar mass at right (arrow on A), and the mass with decreased dimensions after treatment (arrow on B).
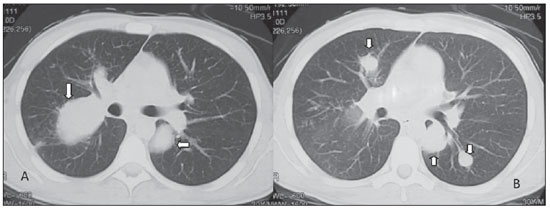
Figure 2. Chest computed tomography, lung window, demonstrating aneurysmal dilatations characterized by nodular formations in the upper (arrows on A), middle and lower left lung lobes (arrows on B).
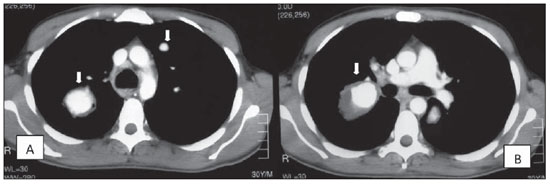
Figure 3. Contrast-enhanced chest computed tomography, on mediastinal window, at the level of the upper lung lobes (A) and of the bronchial bifurcation (B), demonstrating aneurysmal dilatation of the right interlobar artery and of segmental branches at left (arrows).
The diagnosis of Behçet's disease was established on the basis of the presence of oral and recurrent genital ulcers in association with acneiform and cicatricial skin lesions.
DISCUSSION
According to the classification developed by the International Study Group for Behçet's Disease, the presence of recurrent oral ulcers and any two of the following alterations genital ulcers, typical ocular lesions (uveitis, retinal vasculitis), characteristic skin lesions (nodule-like erythema, acneiform and/or cicatricial lesions) , or a positive pathergy test define the diagnosis of Behçet's disease(3).
Chest involvement is observed in 8% of patients and may manifest through a wide range of alterations in the mediastinum, leading to complications such as fibrosing mediastinitis; in the pulmonary parenchyma, where infarction, atelectasis, hemorrhage, diffuse airspace nodules, pneumonia and fibrosis may be observed; in the pleura and mainly in the vascular system(46).
Pulmonary vasculitis observed in Behçet's disease compromises great and medium caliber vessels (according to the Chapel Hill classification criteria for vasculitis), most frequently affecting the venous system in 85% of cases, in the form of thrombophlebitis(4,6). The main venous complications in Behçet's disease are superior vena cava syndrome and Budd-Chiari syndrome(4). Arterial alterations are less frequently observed. The destruction of elastic fibers caused by the inflammatory process of the vasa vasorum results in vascular lumen dilatation and development of aneurysms in 65% of cases(4). Behçet's disease is the main cause o pulmonary artery aneurysms which may occur either in the main segments or in segmental branches, and that can be seen at computed tomography, indicating a poor prognosis(4,5). Such aneurysms may regress with specific medicamentous therapy utilizing corticoid and cyclophosphamide, but disease progression and recurrence are commonly observed in such patients(4,7).
In this case, the main differential diagnosis is Hughes-Stovin syndrome that presents quite similar radiological and histopathological findings; in this syndrome, however, the absence of oral and genital ulcerations is observed (4,6).
Chest radiography is the primary imaging method in the evaluation of Behçet's disease, demonstrating vascular and pulmonary alterations. Such a method is also important in the evaluation of the therapeutic response(4,5). Computed tomography plays a relevant role in the imaging diagnosis of Behçet's disease, particularly through the multidetector technology and therefore the study of vascular, mediastinal and parenchymal structures. Computed tomography angiography performed with such a technology is superior to magnetic resonance imaging, because of its greater spatial resolution, less imaging artifacts, besides the possibility of simultaneous evaluation of the pulmonary parenchyma (4,5). The knowledge on the alterations related to Behçet's disease is useful in the diagnosis, aiding in the determination of the cause of symptoms, particularly hemoptysis, and guiding in the choice of the appropriate treatment.
CONCLUSION
The presence of pulmonary artery aneurysms suggests the diagnosis of Behçet's disease as a primary hypothesis, besides being a sign of poor prognosis.
REFERENCES
1. Erkan F, Gül A, Tasali E. Pulmonary manifestations of Behçet's disease. Thorax. 2001;56:5728.
2. Iscan ZH, Vural KM, Bayazit M. Compelling nature of arterial manifestations in Behcet disease. J Vasc Surg. 2005;41:538.
3. Criteria for diagnosis of Behçet's disease. International Study Group for Behçet's Disease. Lancet. 1990;335:107880.
4. Ceylan N, Bayraktaroglu S, Erturk SM, et al. Pulmonary and vascular manifestations of Behcet disease: image findings. AJR Am J Roentgenol. 2010;194:15864.
5. Hiller N, Lieberman S, Chajek-Shaul T, et al. Thoracic manifestations of Behçet disease at CT. Radiographics. 2004;24:8018.
6. Chung MP, Yi CA, Lee HY, et al. Imaging of pulmonary vasculitis. Radiology. 2010;255:32241.
7. Calamia KT, Schirmer, M, Melikoglu M. Major vessel involvement in Behçet disease. Curr Opin Rheumatol. 2005;17:18.
1. Master, Fellow PhD degree in Health Sciences, Physician Assistant at Diagnostic Imaging Service, Hospital Júlia Kubitschek FHEMIG, Belo Horizonte, MG, Brazil.
2. MD, Specialist in Pneumology, Physician Assistant at Pneumology Service, Hospital Júlia Kubitschek FHEMIG, Belo Horizonte, MG, Brazil.
Mailing Address:
Dra. Andréa de Lima Bastos
Hospital Júlia Kubitschek Fundação Hospitalar do Estado de Minas Gerais (FHEMIG), Unidade de Diagnóstico por Imagem
Rua Doutor Cristiano Rezende, 2745, Bairro Flávio Marques Lisboa (Barreiro)
Belo Horizonte, MG, Brazil, 30620-470
E-mail: andblima@yahoo.com.br
Received February 24, 2011.
Accepted after revision June 21, 2011.
* Study developed at Hospital Júlia Kubitschek FHEMIG, Belo Horizonte, MG, Brazil.
 Vol. 44 nº 6 - Nov. / Dec. of 2011
Vol. 44 nº 6 - Nov. / Dec. of 2011