INTRODUCTION
The utilization of information systems for the management of clinical images and data started being more effectively studied in the late 1980's, with the increase in the utilization of digital data acquisition processes in hospitals(1). Until then, every equipment was considered as being an isolated system, connected only to its own workstation and a printer. However, the increased utilization of data in digital format has led to the need for development of a computational structure which allowed a consistent and automatic exchange of images data in the hospital environment. The PACS (picture archiving and communicasystem) concept was developed to meet such a need. It is an archiving and communication system dedicated to imaging diagnosis that allows immediate access to medical digital images from any sector in a hospital(2). The PACS has quickly become the first option for the management of images in the clinical and hospital environments and, together with the radiology information system (RIS) and the hospital information system (HIS), comprise the basis for a filmless radiology service. A fundamental aspect of the workflow in a digital (filmless) radiology environment is the guarantee of the consistency of the data transmitted from one component to the next within the chain of events in the process dynamics. In order to guarantee such a consistency, the information distribution is carried out according to a hierarchical structure which relies on a top-down distribution, i.e., the information is propagated from a more general information system (HIS) to an intermediate system (RIS), until it reaches a more specific system (PACS). In order to make that possible, two requirements must be met: an appropriate (redundant and balanced) network structure and well defined communication standards. In digital radiology, the main communication standard is the DICOM (digital imaging and communications in medicine) system( 3). The DICOM is the global standard for the transfer of radiological images and other clinical data between computers. The current DICOM, published in 1993 and generally identified as 3.0, evolved from previous versions of a standard developed by the American College of Radiology (ACR) in cooperation with the National Electrical Manufacturers Association (NEMA) of the United States of America (ACR-NEMA 1.0, in 1985, and ACRNEMA 2.0, in 1988). The connectivity designed by the standard is very important with respect to the cost/benefit ratio for health services that utilize medical images.The DICOM users can provide radiology services between facilities located in different geographical regions, making use of already available information technology resources, while keeping costs down by means of new apparatuses and systems compatibility and interoperability(4).
Although technological developments have allowed a more extensive diffusion of image management systems in the medical field over the last years in such a manner that in some situations PACS is considered as a simple commodity(5), in a model of technological maturity(6) there are still some aspects that deserve greater investigation and development. Issues related to digital image acquisition processes(7), data distribution, visualization(8) and interpretation( 9) are still object of studies, particularly with respect to economic aspects and the utilization of freeware and open code(10,11) computational solutions. One should also highlight the integration of tools for aiding in diagnosis into the workflow of image management systems. Computer-aided diagnosis (CAD) can be defined as a diagnosis made by a radiologist who utilizes the result from automated quantitative analyses of radiographic images as a second opinion in the diagnostic decision making process(12). The purpose of CAD is to improve accuracy in diagnosis, as well as the consistency of radiological images interpretation, by utilizing the output from the computer as a reference(13–15). Today, the standard for the utilization of CAD systems is still based on the model of a standalone workstation, without the integration of the obtained results with the information system or with the PACS. The integration of image processing procedures into the PACS workflow has recently been the object of research in the field of information technology in medical imaging(13,16–18).
The present article describes a model for the integration of diagnosis aid tools into the image management environment with the objective of optimizing the visual analysis by the human observer (the radiologist) within the imaging diagnosis workflow. Such model has been developed with an open-source toolkit called dcm4che2. The data management follows the workflow defined by the post-processing workflow profile (PWF) of the Integrating the Healthcare Enterprise (IHE) and utilizes the DICOM secondary capture functionality.The dcm4che2 is an implementation of the high-performance DICOM standard developed in Java programming language, which supports the IHE integration profiles (http://www.dcm4che.org). The IHE is an initiative of the Radiology Society of North America (RSNA), aimed at promoting the systems integration in the healthcare environment.The objective is to improve the clinical practice efficiency and effectiveness by enhancing the data flow based on communication standards. The IHE establishes a technical framework which defines the way the standards are implemented in order to meet the needs of the clinical practice. It utilizes three basic concepts: players, transactions and integration profiles.The players are the functionalities that make the communication between the systems.Transactions are the messages exchanged between the systems. Integration profiles are groups of players and transactions that comprise a specific workflow(3).As a proof of concept, a system prototype to aid in the differential diagnosis of diffuse lung lesions with computed tomography was integrated with the images management system of the imaging diagnosis center of a hospital school.
MATERIALS AND METHODS
A computational testing environment was built to validate the model of integration between the computer aided diagnosis system (CAD) and the medical images management system (PACS). A locally developed computer code for classification of diffuse lung lesions at high resolution computed tomography was selected to play the role of a CAD solution. The selected medical images management system was the DICOM Conquest server (CONQUEST, 2010), and for the visualization of the CAD-PACS integration results, the medical image viewer K-PACS (K-PACS, 2010) was utilized. All the apparatuses in the environment were connected to a 100 Mbit/s local network (LAN).
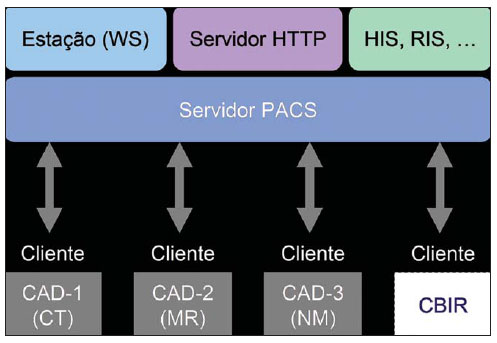
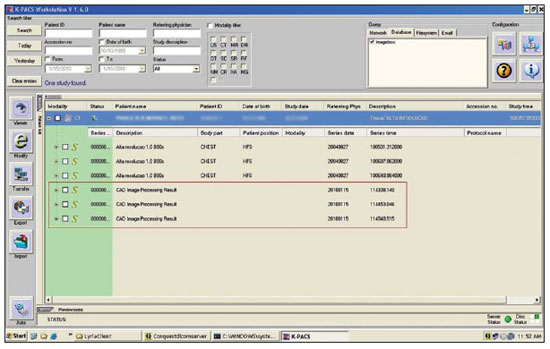
Based on a number of software packages defined by the integration model, a client computer code denominated Client- CAD was developed. Such a code acts as an intermediate entity between the PACS and the CAD, with the objective of integrating the two systems by means of the DICOM communication protocol. The Client- CAD also comprises a software component known as i-CAD, especially utilized to change the serial number of medical images in the digital format(19). Also, in a transparent manner, the Client-CAD provides interfaces that allow the coupling with specific image processing modules for other acquisition modalities, as shown on Figure 1.
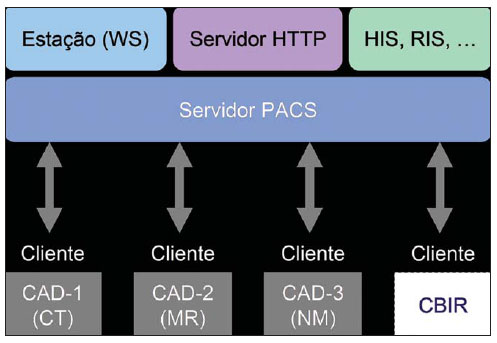
Figure 1.
Integration model architecture. Scheme presenting the integration model architecture and its main components. The CAD applications communicate with the PACS server by means of communication services supplied by the client Client-CAD.
In the testing environment, the CAD system was installed and ran on an individual computer with its own hardware and software resources. In order to allow a direct connection between the CAD and the PACS, the Client-CAD software was also installed in this very computer. Once activated, the client periodically interacts with the PACS through DICOM messages for data query and image retrieval. For example, the DICOM C-Find message expresses a query in a databank based on the information comprised in the standard's data dictionary, and may or may not comprise filters to provide more specific results.In the case of the herein described experiment, the client was configured to query only computed tomography (CT) studies, and the anatomic region of the CHEST. Therefore, as the PACS server receives a new chest HRCT study, the client requests to the PACS a copy of such study by sending image search and retrieval messages (query & retrieve). The retrieved images are then processed one at a time by the CAD system processing routine.
The CAD processing routine comprises five steps as follows: pre-processing, segmentation, characteristics extraction, classification and post-processing. In the preprocessing, the image data (pixels) are extracted from the DICOM file. In the next step, the lungs are segmented by means of an interactive algorithm for image thresholding( 20) and the resulting image is divided into 20 × 20-pixel regions of interest (ROIs). During the classification step, each ROI is defined as belonging to one of the seven approached interstitial lung lesion classes as follows: normal, ground glass attenuation, reticular, nodular, honeycombing, emphysema and consolidation. In the post-processing step, each ROI receives a color which identifies its characterization class and a new DICOM file is generated with the results from the processing.
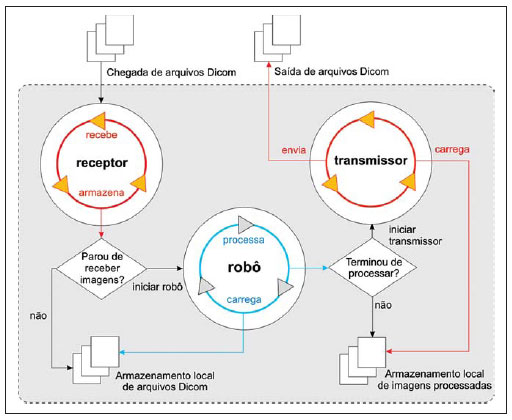
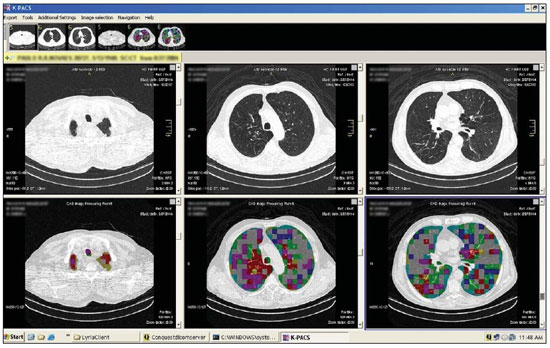
The CAD-PACS integration is completed as the client, by means of the i-CAD software component, modifies the serial number of the new DICOM file and sends it back to the PACS server. Figure 2 depicts the functioning principle of the Client- CAD code.
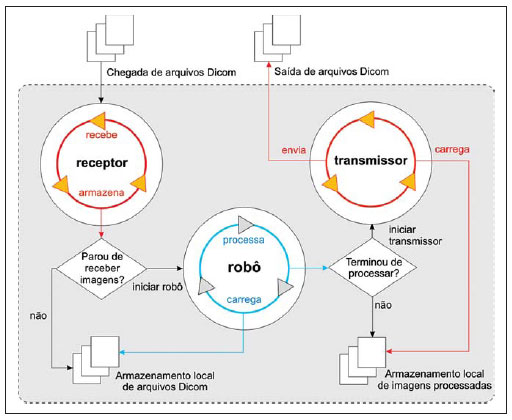
Figure 2.
Client-CAD functioning scheme. Functioning principle of the Client-CAD module created with basis on the CAD-PACS integration model. It illustrates the functioning of the receptor, robot and transmitter processes responsible for the processing and transmission of the CAD results to the PACS.
Based on the architecture of the client operation, the first process denominated receptor represents an independent computer code which implements a DICOM service provider for images storage (storage service class provider – CStore SCP). It starts running whenever the client requests a copy of a given imaging study stored at PACS. For each received image, the client invokes the robot process that, on its turn, initiates the CAD system image processing routine.
As the CAD routine is completed, the robot locally stores the image resulting from the processing and initiates the third and last process, the transmitter. In this stage, the i-CAD is utilized to change the serial number of the processed image. Completing the integration cycle, the transmitter sends DICOM messages for images storage request (storage service class user – CStore SCU) and sends the resulting image to the PACS server.
RESULTS
The experiment results are directly related to the development of the Client-CAD software and to the success of the integration between the computer aided diagnosis system (CAD) for diffuse lung lesions and the medical images management system. The Client-CAD workflow comprises four vital tasks which contributed to the integration success, as follows:
– query & retrieval: the client periodically queries the PACS server searching for new imaging studies by sending DICOM C-Find messages. The query is always performed by utilizing the data model for images query and retrieval at the study level (study root query retrieve information model FIND);
– CAD processing: Once received and stored, the images are processed one at a time by the CAD routine initiated by the client. For each image, the processing result consists of a JPEG image which comprises relevant data that may be of assistance in the decision making by the radiologist;
– encapsulation: each resulting JPEG image is encapsulated by the client in a compatible DICOM format. Mandatory data in the dictionary, such as patients' identification and name, for example, are copied from the original DICOM file. The difference between the original file and the encapsulated version lies on the way the file is built. The encapsulated DICOM file is encoded from a JPEG image and follows the information model of the DICOM secondary capture image storage SOP class;
– transmission: the resulting image transmission is performed by sending the DICOM C-Store SCU message implemented on the client. Thus, when the PACS server receives the encapsulated DICOM file, the file manager stores its contents in the same patient folder of the original file, but within a new image series according to the new serial number generated by the i- CAD code.
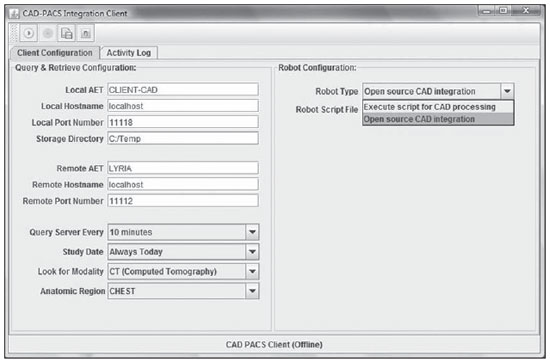
Figure 3 presents the interface of the client Client-CAD code. It is possible to visualize several of the utilized parameters. The fields on the left upper corner are utilized for the configuration of the DICOM communication between the client and the PACS server. Immediately below are the fields that identify the PACS to be queried. And below that, the last field establishes the scheduling configurations for the client's queries and images retrieval.
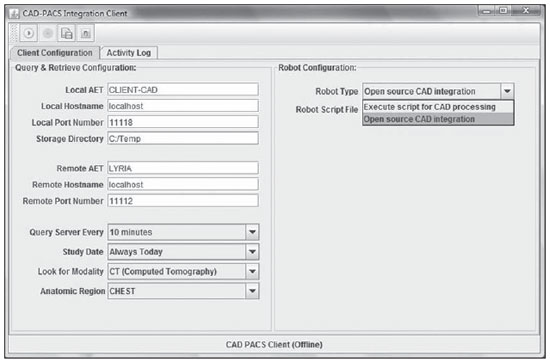
Figure 3.
Client-CAD interface. Client-CAD code. Interface for the configuration of the communication with the PACS server.
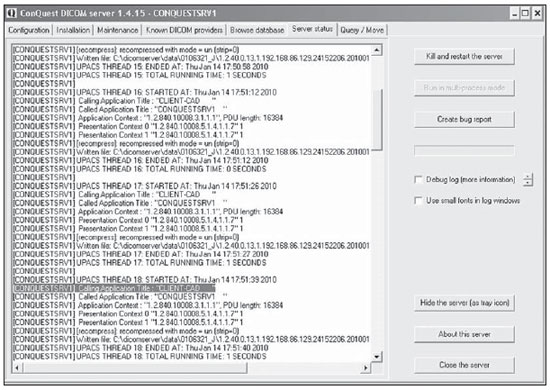
In order to illustrate the CAD-PACS communication, Figure 4 presents the interaction between the client and the PACS Conquest Server. In the highlighted area one visualizes an entity called "CLIENTCAD" requesting the storage of an image resulting from the CAD processing. Once the resulting images are correctly stored in the PACS server, it is possible to visualize the new series created by the CAD-PACS integration on the display station. Figures 5 and 6 show the K-PACS viewer presenting examples of original image series side beside the corresponding CAD system processed images.
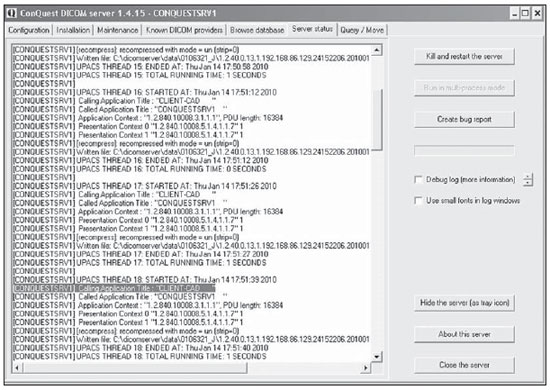
Figure 4.
DICOM Server interface. Conquest Server interface for the visualization of events and status. On the highlighted area, the interaction between the server and the Client-CAD can be seen.
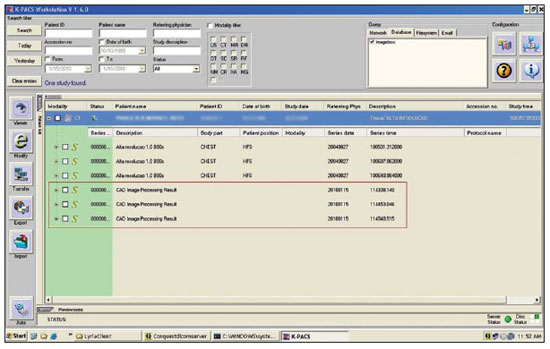
Figure 5.
Updated list of study series. K-PACS viewer query interface. On the highlighted area, three new processed images series after the CAD-PACS integration process completion.
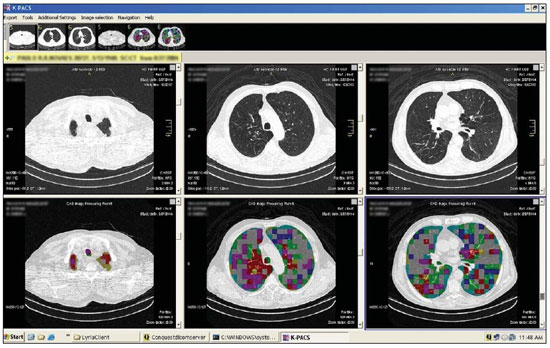
Figure 6.
Example of a display screen. K-PACS viewer module after CAD-PACS integration. The patient’s original images series are shown on the top. On the bottom, the corresponding CAD processed images.
The initial trials demonstrated a good potential for the proposed model for CADPACS integration, but an important limitation respects the types of files utilized during the integration workflow. Currently, DICOM and JPEG are the supported formats. Therefore, the integration model is compatible with CAD applications that provide JPEG images as a processing output. One should highlight that the DICOM encapsulated JPEG image does not provide the same diagnostic quality as the original image, because of the format's inherent losses, and should therefore be utilized as a complementary information in the decision making process based on the visual inspection of the original images series. In case the CAD is not capable of providing the output in the JPEG format, a possible solution would be capturing and encapsulating the image on the computer screen as the result is presented. Such a simple alternative, however, may in a certain way compromise the reading of results and impair the data interpretation by the physician, due to the various visual and text elements present on the computer screen, which comprise the captured image. In general, the CAD systems do not always present results only in the form of an image. It is common to find quantitative data distributed on worksheets, charts, HTML documents and even complete reports in PDF file format. Such data are relevant and, if integrated into the patient's study in the PACS server, may provide a valuable source of information to assist the physician in the decision making process. Such integration can be performed with methods available at DICOM structured reporting (SR), a new extension of the DICOM standard which establishes standards for encoding documents incorporating references for medical images and related data, as well as services for data transmission and exchange.An integration model based on the properties of the DICOM-SR would be more complete and would further allow interactive activities of data retrieval, for example, content based image retrieval (CBIR).
The actual contribution of a diagnosis aid tool depends on the synergy between the professional and the tool. Such a synergic interaction does not generally occur naturally, demanding user training and appropriateness of the computer solution. The experiment herein described presents a model of image processing tools integration that is transparent within the workflow of a digital radiology environment. However the assessment of the effective contribution of the implemented solution as a supporting tool for the decision making process, based on observer tests for the measurement of diagnostic accuracy was not comprised by the scope of the investigation in the present study.
CONCLUSION
With the massive dissemination of digital apparatuses for the acquisition of medical images, together with the adoption of data management solutions (PACS), the existence of imaging diagnosis centers working under the filmless radiology model has become increasingly common. In a filmless environment, the images are stored and distributed according to the DICOM standard functionalities. The image processing with a view on computer aided diagnosis has been a relevant research field over the last years, with commercial solutions being introduced with the approval for clinical use by the Food and Drug Administration (FDA). In this context, the possibility of integrating tools for diagnosis aid in the environment of medical images management can contribute to optimize the activity of the specialist physician, allowing access to computer data in a transparent and integrated manner. The present article describes an integration model developed on the basis of freeware DICOM libraries. In spite of being focused on the aid in the differential diagnosis of diffuse pulmonary lesions at computed tomography, the implemented framework can be easily extended to other automatic computer applications which do not require interaction with the users. Such extension to other applications would essentially depend on the image processing routine appropriateness to the new area, according to their complexity and standard variations.
REFERENCES
1. Wiley G. The prophet motive: how PACS was developed and sold. Imaging Economics – May 2005. [acessado em 8 de agosto de 2011. Disponível em: http://www.imagingeconomics.com/ issues/articles/2005-05_01.asp
2. Siegel EL, Kolodner RM. Filmless radiology: state of the art and future trends. In: Siegel EL, Kolodner RM, editors. Filmless radiology. New York, NY: Springer-Verlag; 1999. p. 3–20.
3. Azevedo-Marques PM, Salomão SC. PACS: sistemas de arquivamento e distribuição de imagens. Rev Bras Fís Méd. 2009;3:131–9.
4. Horii SC. A nontechnical introduction to DICOM. RSNA Informatics. [acessado em 8 de agosto de 2011]. Disponível em: http://www.rsna.
org/technology/dicom/intro/index.cfm 5. Chen J, Bradshaw J, Nagy P. Has the picture archiving and communication system (PACS) become a commodity? Journal of Digital Imaging. 2011;24:6–10.
6. van de Wetering R, Batenburg R. A PACS maturity model: a systematic meta-analytic review on maturation and evolvability of PACS in the hospital enterprise. Int J Med Inform. 2009;78:127– 40.
7. Vela JG, Bhaya A, Monteiro AMV, et al. Digitalização de filmes radiográficos com costura de imagens. Radiol Bras. 2011;44:233–7.
8. Parizoti A, Netto TG. Estudo de otimização de imagens em fluoroscopia intervencionista. Radiol Bras. 2009;42:375–8.
9. Ferreira DM, Cohrs FM, Lederman HM, et al. Comparação dos tempos de geração e digitação de laudos radiológicos entre um sistema eletrônico baseado em voz sobre IP (VoIP) e um sistema tradicional baseado em papel. Radiol Bras. 2010;43:7–12.
10. Nobre LF, von Wangenheim A. Software gratuito: uma opção para o radiologista? Radiol Bras. 2010;43(5):ix-x.
11. Barra FR, Barra RR, Barra Sobrinho A. Visualizadores de imagens médicas gratuitos: é possível trabalhar apenas com eles? Radiol Bras. 2010;43:313–8.
12. Azevedo-Marques PM. Diagnóstico auxiliado por computador na radiologia. Radiol Bras. 2001;34:285–93.
13. Doi K. Computer-aided diagnosis in medical imaging: historical review, current status and future potential. Comput Med Imaging Graph. 2007;31:198–211.
14. Azevedo CM, Alvarenga AV, Pereira WCA, et al. Análise computacional da textura de tumores de mama em imagens por ultrassom de pacientes submetidas a cirurgia conservadora. Radiol Bras. 2009;42:363–9.
15. Pádua RDS, Oliveira LF, Azevedo-Marques PM, et al. Auxílio à detecção de anormalidade perfusional miocárdica utilizando atlas de SPECT e registro de imagens: resultados preliminares. Radiol Bras. 2008;41:397–402.
16. Caritá EC, Seraphim E, Honda MO, et al. Implementação e avaliação de um sistema de gerenciamento de imagens médicas com suporte à recuperação baseada em conteúdo. Radiol Bras. 2008;41:331–6.
17. Azevedo-Marques PM, Ponciano-Silva M, Salomão SC, et al. CAD-PACS integration: a framework for pattern recognition of diffuse lung disease in HRCT. Int J Comput Assist Radiol Surg. 2009;4 Suppl 1:S177–83.
18. Le AH, Liu B, Huang HK. Integration of computer- aided diagnosis/detection (CAD) results in a PACS environment using CAD-PACS toolkit and DICOM SR. Int J Comput Assist Radiol Surg. 2009;4:317–29.
19. Zhou Z, Liu BJ, Le AH. CAD-PACS integration tool kit based on DICOM secondary capture, structured report and IHE workflow profiles. Comput Med Imaging Graph. 2007;31:346–52.
20. Bugatti PH, Ponciano-Silva M, Traina AJM, et al. Content-based retrieval of medical images: from context to perception. Computer-Based Medical Systems, 2009. CBMS 2009. 22nd IEEE International Symposium on; 2009 Aug 2–5; Albuquerque, NM. Proc CBMS. 2009; p. 1–8.
1. Master of Bioengineering, Independent Advisor of Health Informatics, Ribeirão Preto, SP, Brazil.
2. Private Docent, Associate Professor, Department of Internal Medicine, Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (FMRPUSP), Ribeirão Preto, SP, Brazil.
Mailing Address:
Dr. Paulo Mazzoncini de Azevedo Marques
Departamento de Clínica Médica, FMRPUSP
Avenida Bandeirantes, 3900, Monte Alegre
Ribeirão Preto, SP, Brazil, 14049-900
E-mail: pmarques@fmrp.usp.br
Received August 10, 2011.
Accepted after revision October 24, 2011.
Financial support: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq).
* Study developed at Centro de Ciências das Imagens e Física Médica do Hospital das Clínicas da Faculdade de Medicina de Ribeirão Preto da Universidade de São Paulo (CCIFM/HC-FMRPUSP), through the Interunits Program of Post-graduation in Bioengineering (EESC/IQSC/FMRP), Universidade de São Paulo, Ribeirão Preto, SP, Brazil.
 Vol. 44 nº 6 - Nov. / Dec. of 2011
Vol. 44 nº 6 - Nov. / Dec. of 2011