INTRODUCTION
Intracapsular temporomandibular joint (TMJ) disorders refer to changes in the TMJ articular capsule. In the past, the diagnosis of such a condition was limited to physical examination and plain radiological examination by means of radiography of the joint with the patient at rest and after opening the mouth, with lateral and panoramic views of the mandible.
The arrival of magnetic resonance imaging (MRI), with excellent resolution for the diagnosis of TMJ alterations, allowed the analysis of soft parts of the joint, as well as its lining cartilage and the articular disc(1). Magnetic resonance imaging is currently the gold standard for evaluation of intracapsular TMJ disorders.
Ultrasonography (US) may represent a useful option in cases of internal TMJ disorders and in the cases of patients with contraindications for MRI, such as those presenting with claustrophobia or with pacemakers.
This study was aimed at evaluating the sensitivity and specificity of high resolution US in the assessment of intracapsular TMJ disorders, attempting to establish parameters and technical standards for analysis.
The temporomandibular joint
Temporomandibular joints are large bicondylar joints comprising the osseous components of the glenoid fossa and the mandibular condyle. It also comprises a flexible articular disc, attached by ligaments and tendons which divide the articular space in two compartments: the superior and inferior compartments(2,3).
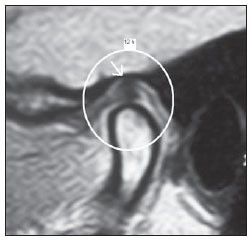
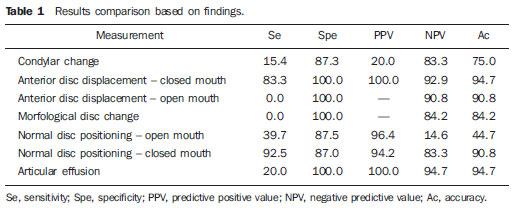
With the patient keeping the mouth closed, the mandibular condyle is located in the central region of the glenoid fossa and the position of the articular disc is considered normal as its posterior portion is located between 12 and 1 o'clock on the articular surface of the mandibular condyle, as shown on Figure 1.
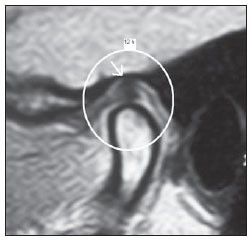
Figure 1. MRI – sagittal T1-weighted image. The mandibular condyle is positioned in the middle of the glenoid cavity and the posterior portion of the articular disc is considered normal as it is located between 12 and 1 o’clock on the articular surface of the mandibular condyle (arrow).
The articular disc presents a biconcave appearance in the middle, appearing like a "bow-tie" at MRI, although normal morphological variations may be observed. The middle of the disc, the intermediate zone, must be positioned at the anterosuperior aspect of the condyle with the patient keeping the mouth closed (Figure 1).
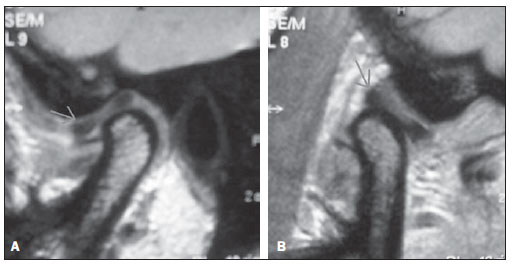
The collateral ligaments fix the disc medially and laterally. The superior and inferior retrodiscal ligaments posteriorly fix the disc, where they fuse with the posterior portion of the articular disc that contains a neurovascular bundle. The disc is anteriorly attached to the tendinous portion of the lateral pterygoid muscle. With the opening of the mouth, the digastric muscle forces the inferior condylar displacement, anteriorly and medially through the articular space, while the retrodiscal ligaments stabilize the disc, which can move up to 25 mm (Figure 2).
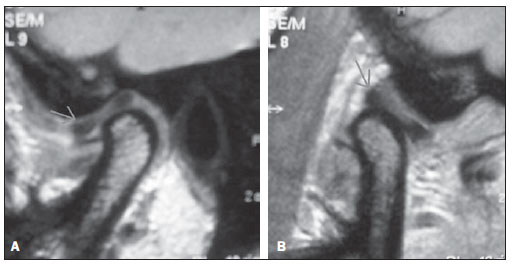
Figure 2. MRI. A: Sagittal section demonstrating habitual topography of the articular disc with the patient at rest. B: Sagittal section showing physiological articular disc displacement after opening the mouth.
The etiologies for intracapsular TMJ disorders may be related to odontogenic disorders, infections or neoplasias, but in the greatest majority of cases they are related to problems originated from the articular discs(4,5).
Disc displacement is defined as an abnormal relationship of the articular disc with the mandibular condyle, glenoid cavity and articular eminence. Displacement may occur either with or without reduction, and such classification will depend upon whether or not the normal relationship between the articular disc and the condyle will be restored after the opening of the mouth. Disc displacement with reduction occurs as the disc is displaced with the patient at rest, and is recaptured to its physiological position after the opening of the mouth. Disc displacement without reduction occurs as the disc remains out of its habitual position after the opening of the mouth. The disc reduction is considered incomplete as the recapture after opening the mouth is partial, or complete as the recapture is fully achieved(6).
Studies indicate that the prevalence of disc displacement in asymptomatic individuals ranges between 12% and 34%(7). Clinically, TMJ disorders related to the articular disc can range from clicking and/or opening limitation, observed in the early stages, to crepitus, lock jaw and progression to osteoarthrosis, in advanced cases.
MATERIALS AND METHODS
Ultrasonography and MRI were performed in 38 patients presenting with intracapsular TMJ disorder.
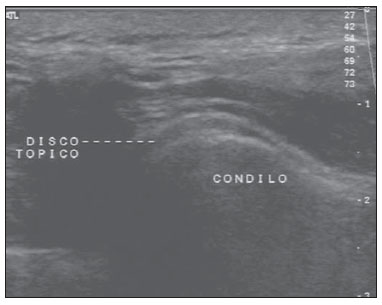
A control group including 10 healthy voluntary individuals (20 joints), with no history of temporomandibular disorder was selected. All the volunteers have given their previous written consent. All of them underwent ultrasonography for characterization of the correct articular discs positioning that was later confirmed by MRI. In the control group, the physiological positioning of the articular disc and its characteristics were demonstrated at US. The articular disc presents intermediate and homogeneous echogenicity, which allows the visualization of the posterior 2/3 of the disc with the patient keeping the mouth closed (Figure 3).
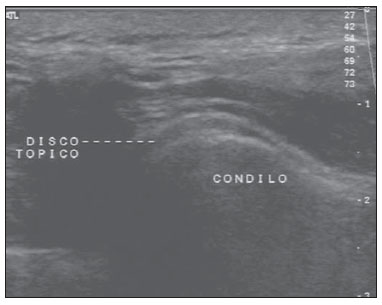
Figure 3. The articular disc presents intermediate and homogeneous echogenicity at US, allowing the visualization of the posterior 2/3 of the disc with the patient at rest.
Overall, 76 joints were studied in 38 patients, nine of them being men and 29, women, with ages ranging between 16 and 65 years and mean age of 33.13 years. All the patients submitted to the study were referred to the service with symptoms related to TMJ, such as pain, clicking when opening the mouth and/or TMJ locking.
The scans were performed with a HDI 5000 ATL apparatus (ATL, Philips Medical Systems; Bothell, WA, USA), equipped with a 12.5 MHz transducer, after verbal detailed explanation on the procedure and after obtaining written consent from the patients and approval by the Human Research Ethics Committee of Universidade de São Paulo. All patients underwent MRI scans in a 1.0 or 1.5 T Philips apparatus, equipped with a TMJ coil, with sagittal and coronal T1- and T2-weighted sequences, without the utilization of paramagnetic contrast medium, since, according to the literature, such a procedure is considered as the gold standard for the evaluation of TMJ disorders(1).
The US scans were performed with oblique axial sections, with the patients in dorsal decubitus (Figure 4), evaluating the following parameters: visualization or not of the articular disc with the mouth closed and after opening it, presence of joint effusion, morphological changes of the articular disc, such as ruptures and degenerative processes, and in the mandibular condyle, such as the presence of osteophytes or abnormalities on the articular surface.

Figure 4. US transducer positioning for the study of TMJ articular disc.
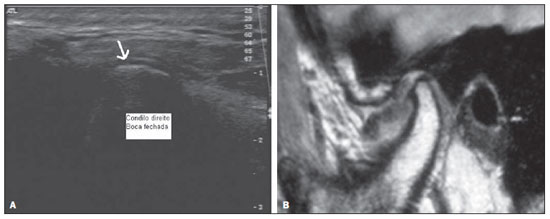
The articular disc position was considered normal when its posterior portion was located between 12 and 1 o'clock on the articular surface of the mandibular condyle (Figure 4). In the present study, anterior displacement was considered whenever the posterior portion of the disc was located before the 12 o'clock position, the case was considered as being anterior displacement. Cases where the articular disc was not visualized at US with the patient keeping the mouth closed were considered as being a disc displacement (Figure 5).
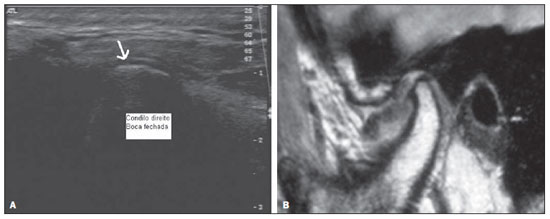
Figure 5. Patient presenting complete anterior disc displacement. A: Ultrasonography demonstrating the non-visualization of the disc on the condylar surface (arrow). B: MRI demonstrating anterior articular disc displacement, which was not characterized at ultrasonography.
All the patients underwent US scans whose results were later compared with the MRI findings. In the statistical analysis, several performance measurements for US (test) were calculated and compared with the MRI results (gold standard) as follows: sensitivity, specificity, positive predictive value, negative predictive values and accuracy. All the US scans were performed by an experienced radiologist and titular member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem.
RESULTS
Magnetic resonance imaging with the patients keeping their mouths closed demonstrated 24 TMJ with anterior disc displacement. In these same articulations, US demonstrated anterior displacement in 7, while in 13 the discs could not be visualized, and in 4, disc displacement was not observed.
In 48 joints, the articular disc could not be visualized at US with the patients keeping their mouths closed. Of those joints, 41 presented normal positioning at MRI and 7 presented anterior displacement.
Morphological alterations in the mandibular condyle were visualized by MRI in 13 joints; on the other hand, US identified such alterations in 2 joints of this latter group. Articular effusion was visualized by MRI in 5 joints, and by US in only 1 joint.
Magnetic resonance imaging demonstrated alterations in the articular discs, such as changes in signal intensity or loss of habitual morphology in 12 joints, which were not visualized at US.
Table 1 shows the results from each one of the statistical measurements evaluated in the present study for each of the findings.
DISCUSSION
At MRI, 24 joints with anterior displacement of the articular disc were identified with patients keeping their mouths closed. In such joints, US demonstrated articular displacement in 7 cases, while in 13 cases the discs could not be visualized on the articular surface, and in 4 disc displacement was not observed at US. The authors considered that the non-visualization of the disc on the condylar surface with the patients at rest is related to the articular disc displacement. Thus, US allowed the diagnosis of 20 (83.3%) among the 24 disc displacements observed in the present study. Such findings are similar to those in the studies developed by Emshoff et al.(8,9), that demonstrated sensitivity and specificity around 90—95% for these parameters. Studies developed by Jank et al.(10) have also demonstrated high sensitivity (90%) and specificity (84%) for the evaluation of the articular disc with the patient at rest. Studies developed by Emshoff et al.(11) have demonstrated accuracy > 90% in the evaluation of disc displacement by US. Similar results were obtained by Hayashi et al.(12), whose studies demonstrated sensitivity and specificity of 83% and 96%, respectively.
The US findings related to condylar changes demonstrated that the method does not present yet significant sensitivity in the diagnosis of disorders related to the morphology and changes of the condylar cortical bone, a fact that was also observed by Emshoff et al.(13). Studies developed by Brandlmaier et al.(14) have demonstrated sensitivity of 87% and specificity of 20% in the diagnosis of TMJ osteoarthritis, indicating that US may be useful in the diagnosis of the presence, but insufficient to diagnose absence of osteoarthritis.
The presence of articular effusion is an uncommon sign in asymptomatic patients(15). More extensive articular effusion may be observed in patients with articular dysfunction(16). The present study has not included a significant number of patients to enable the establishment of parameters in relation to the sonographic diagnosis of presence of articular effusion, although recent studies report that US presents good sensitivity for such evaluation. Tognini et al.(17) have developed studies demonstrating values sensitivity and specificity of about 75% for US in the detection of intra-articular fluid.
The method has not demonstrated significant sensitivity for the visualization of articular disc with the patient keeping the mouth open. In 48/76 joints (63%) the disc could not be visualized at US after the opening of the mouth. The disc could not be visualized either in 6 joints with open mouth in patients of the control group. Such finding is probably related to the medial displacement of the articular disc after opening the mouth, as the mandibular condyle and the glenoid cavity do not allow appropriate ultrasound propagation, impairing the visualization of the articular disc.
Also, the method did not present significant sensitivity for the evaluation of morphological changes in the disc, as those identified in 12 joints at MRI and in none at US.
The present study demonstrates that, although still with limitations, the evaluation by US can become a useful option in the initial study of TMJ disorders in patients with contraindications for MRI, besides being more financially accessible, a fact with significant relevance in Brazil. In the future, further studies utilizing transducers with higher resolution may eventually allow a more complete and accurate analysis of the joint.
CONCLUSIONS
Ultrasonography presented high sensitivity and specificity in the identification of TMJ articular disc displacement as compared with MRI that is the gold standard, and when the US scans were performed with the mouth closed. The results suggest that US can eventually be considered as an alternative method to detect the correct positioning or disc displacement in patients who cannot be submitted to MRI.
The method has not presented satisfactory results in the characterization of articular discs with patients keeping their mouths open as well as for detection of morphological changes in articular discs and mandibular condyles.
REFERENCES
1. Sano T. Recent developments in understanding temporomandibular joint disorders. Part 1: Bone marrow abnormalities of the mandibular condyle. Dentomaxillofac Radiol. 2000;29:7—10.
2. Ramos ACR, Sarmento VA, Campos PSF, et al. Articulação temporomandibular — aspectos normais e deslocamentos de disco: imagem por ressonância magnética. Radiol Bras. 2004;37:449—54
3. Fritz J, Thomas C, Tzaribachev N, et al. MRI-guided injection procedures of the temporomandibular joints in children and adults: technique, accuracy, and safety. AJR Am J Roentgenol. 2009;193:1148—54.
4. Katzberg RW. Temporomandibular joint imaging. Radiology. 1989;170:297—307.
5. Sommer OJ, Aigner F, Rudisch A, et al. Cross-sectional and functional imaging of the temporomandibular joint: radiology, pathology, and basic biomechanics of the jaw. Radiographics. 2003;23:e14.
6. Milano V, Desiate A, Bellino R, et al. Magnetic resonance imaging of temporomandibular disorders: classification, prevalence and interpretation of disc displacement and deformation. Dentomaxillofac Radiol. 2000;29:352—61.
7. Schmitter M, Kress B, Ludwig C, et al. Temporomandibular joint disk position assessed at coronal MR imaging in asymptomatic volunteers. Radiology. 2005;236:559—64.
8. Emshoff R, Jank S, Rudisch A, et al. Are high-resolution ultrasonographic signs of disc displacement valid? J Oral Maxillofac Surg. 2002;60:623—8; discussion 628—9.
9. Emshoff R, Jank S, Rudisch A, et al. Error patterns and observer variations in the high-resolution ultrasonography imaging evaluation of the disk position of the temporomandibular joint. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 2002;93:369—75.
10. Jank S, Rudisch A, Bodner G, et al. High-resolution ultrasonography of the TMJ: helpful diagnostic approach for patients with TMJ disorders? J Craniomaxillofac Surg. 2001;29:366—71.
11. Emshoff R, Jank S, Bertram S, et al. Disk displacement of the temporomandibular joint: sonography versus MR imaging. AJR Am J Roentgenol. 2002;178:1557—62.
12. Hayashi T, Ito J, Koyama J, et al. The accuracy of sonography for evaluation of internal derangement of the temporomandibular joint in asymptomatic elementary school children: comparison with MR and CT. AJNR Am J Neuroradiol. 2001;22:728—34.
13. Emshoff R, Brandlmaier I, Bodner G, et al. Condylar erosion and disc displacement: detection with high-resolution ultrasonography. J Oral Maxillofac Surg. 2003;61:877—81.
14. Brandlmaier I, Rudisch A, Bodner G, et al. Temporomandibular joint internal derangement: detection with 12.5 MHz ultrasonography. J Oral Rehabil. 2003;30:796—801.
15. Tomas X, Pomes J, Berenguer J, et al. MR imaging of temporomandibular joint dysfunction: a pictorial review. Radiographics. 2006;26:765—81.
16. LarheimTA, Katzberg RW, Westesson PL, et al. MR evidence of temporomandibular joint fluid and condyle marrow alterations: occurrence in asymptomatic volunteers and symptomatic patients. Int J Oral Maxillofac Surg. 2001;30:113—7.
17. Tognini F, Manfredini D, Melchiorre D, et al. Ultrasonographic vs magnetic resonance imaging findings of temporomandibular joint effusion. Minerva Stomatol. 2003;52:365—72.
1. PhD, Associate Professor, Division of Radiology, Course of Medicine, Universidade Federal da Paraíba (UFPB), João Pessoa, PB, Brazil.
2. PhD, MD, Physician Assistant at Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil.
3. PhD, MD, Physician Assistant at Ecoclínica Diagnósticos, João Pessoa, PB, Brazil.
Mailing Address:
Dr. Carlos Fernando de Mello Junior
Rua Valdemar Chianca, 365, ap. 1001, Bessa
João Pessoa, PB, Brazil, 58037-255
E-mail: carlosfmello@hotmail.com
Received March 26, 2011.
Accepted after revision October 18, 2011.
* Study developed at Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (FMUSP), São Paulo, SP, Brazil.
 Vol. 44 nº 6 - Nov. / Dec. of 2011
Vol. 44 nº 6 - Nov. / Dec. of 2011