Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 6 - Nov. / Dec. of 2011
Vol. 44 nº 6 - Nov. / Dec. of 2011
|
WHICH IS YOUR DIAGNOSIS?
|
|
WHICH IS YOUR DIAGNOSIS? |
|
|
Autho(rs): Karen Fayad Gemus1; Guilherme de Palma Abrão2; Cláudia Mendes Tagliari1; Wagner M. Mariushi2; Enéas Cota Machado Filho3; Alair Augusto Sarmet Moreira Damas dos Santos4 |
|
|
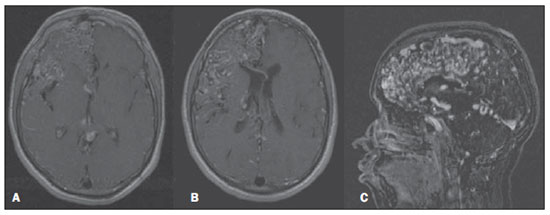
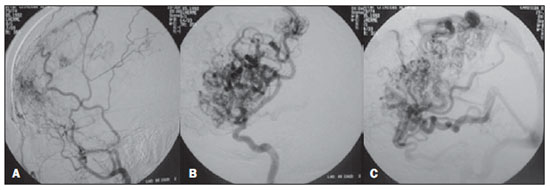
An 18-year-old patient presenting right holocranial headache and convulsive seizures, with progressive hemiparesis at left.
Images description Figure 1. Non-contrast-enhanced (A) and contrast-enhanced (B) skull computed tomography demonstrating a diffuse meshwork of tortuous, dilated vessels in the right cerebral hemisphere. 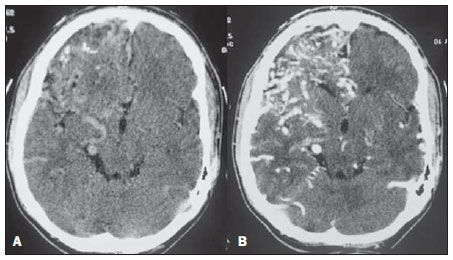 Figure 1. Skull computed tomography. Figure 2. Skull magnetic resonance imaging: contrast-enhanced axial, T1-weighted image demonstrating multiple abnormal vessels intermingled with healthy cerebral parenchyma (A,B), and MRI angiogram of intracranial vessels, venous phase (C), demonstrating anterior, middle and posterior right afferent cerebral arteries, and capillary ectasias with cortical reflux. Figure 3. Digital angiogram of right external carotid artery (lateral) demonstrating transdural shunts (A) and right internal carotid artery (lateral), arterial and venous phases demonstrating capillary ectasias and drainage through cortical and deep veins (B,C). Diagnosis: Proliferative cerebral angiopathy. COMMENTS Notwithstanding its uncertain etiology, proliferative cerebral angiopathy is characterized by endothelial proliferation and angiogenesis, corresponding to 2—4% of cerebral arteriovenous malformations(1). Such condition has a predilection for young, female patients, presenting progressive neurologic deficit, transient ischemic attack, convulsions and disabling headaches as most common symptoms. Hemorrhage episodes are less frequent than in classic arteriovenous malformations(2). The natural history, clinical presentation and the recognition of radiological findings allow the differentiation of proliferative cerebral angiopathy from classic arteriovenous malformations, determining different therapeutic strategies. There is a progressive, vicious circle cascade where the arterial supply associated with venous ectasia creates an environment of local increase in the blood volume and perinidal areas of severe hypoperfusion, triggering an uncontrolled, progressive angiogenic response to this healthy brain with an abnormal blood demand(3). The name proliferative cerebral angiopathy was strictly based on the angiographic evidence of non-focal angiogenic activity, i.e., the presence of transdural supply and afferent arteries stenosis. Other distinct characteristics include absence of dominant feeder vessels to the nidus (generally lobar or hemispheric), draining veins moderately dilated in relation to the size of the arteriovenous shunting zone, and presence of healthy cerebral tissue intermingled with vascular spaces(3), as demonstrated by magnetic resonance imaging (Figure 2). Such findings are determining factors in the diagnostic differentiation between proliferative cerebral angiopathy and classic arteriovenous malformations(3). Differential diagnoses include hereditary hemorrhagic telangiectasia (Rendu-Osler-Weber syndrome), Sturge-Weber syndrome, Wyburn-Mason syndrome and Dirvy-Van Bogaert angiomatosis(4—6). The therapeutic strategy to be adopted should consider the presence of healthy cerebral tissue intermingled with vascular spaces. Arterial embolization of pial afferents in extensive areas determines high risk for permanent neurological deficits(7). The symptoms can be reduced by means of arterial embolization limited to non-eloquent areas and to transdural shunts(2). Since ischemia is the main pathological mechanism of the disease, leading to decelerated angiogenesis, convulsions, headaches and theft syndrome, similar to Moyamoya disease, such signs and symptoms can be reduced by trepanation in the calvarium, which enhances the cortical blood supply by recruitment of additional blood supply(3). As a function of the disease development stage and symptoms, a conservative treatment, with symptoms management and rehabilitation of deficits already present, may be adopted in cases where the risk for occlusion of healthy structures is greater than the arterial embolization benefits. In the present case, such a conservative approach was adopted. REFERENCES 1. Lasjaunias PL, Landrieu P, Rodesch G, et al. Cerebral proliferative angiopathy: clinical and angiographic description of an entity different from cerebral AVMs. Stroke. 2008;39:878—85. 2. Dória-Netto HL, Souza-Filho AM, Dória-Netto RH, et al. Cerebral proliferative angiopathy. Arq Neuropsiquiatr. 2010;68:300—2. 3. Geibprasert S, Pongpech S, Jiarakongmun P, et al. Radiologic assessment of brain arteriovenous malformations: what clinicians need to know. Radiographics. 2010;30:483—501. 4. Schreiber SJ, Doepp F, Bender A, et al. Diffuse cerebral angiomatosis. Neurology. 2003;60:1216—8. 5. Sujansky E, Conradi S. Sturge-Weber syndrome: age of onset of seizures and glaucoma and the prognosis for affected children. J Child Neurol. 1995;10:49—58. 6. Ponce FA, Han PP, Spetzler RF, et al. Associated arteriovenous malformation of the orbit and brain: a case of Wyburn-Mason syndrome without retinal involvement. Case report. J Neurosurg. 2001;95:346—9. 7. Chin LS, Raffel C, Gonzalez-Gomez I, et al. Diffuse arteriovenous malformations: a clinical, radiological, and pathological description. Neurosurgery. 1992;31:863—8; discussion 8—9. 1. Fellows in Radiology and Imaging Diagnosis, Hospital de Clínicas de Niterói (HCN), Niterói, RJ, Brazil. 2. MDs, Physicians Assistants, Unit of Diagnostic and Therapeutic Neuroradiology of the Imaging Center at Hospital de Clínicas de Niterói (HCN), Niterói, RJ, Brazil. 3. MD, Neurosurgeon, Unit of Neurosurgery, Hospital de Clínicas de Niterói (HCN), Niterói, RJ, Brazil. 4. Coordinator for the Imaging Center at Hospital de Clínicas de Niterói (HCN), Associate Professor and Head of the Unit of Radiology at Hospital Universitário Antônio Pedro, Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil. Mailing Address: Dra. Karen Fayad Gemus Rua São Manuel, 20, ap. 503, Botafogo Rio de Janeiro, RJ, Brazil, 22290-010 E-mail: karengemus@yahoo.com.br Study developed at Hospital de Clínicas de Niterói (HCN), Niterói, RJ, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554