INTRODUCTION
Computed tomography-guided transthoracic needle biopsy has been widely utilized as an effective and safe diagnostic procedure in many clinical settings and in different organs(1).
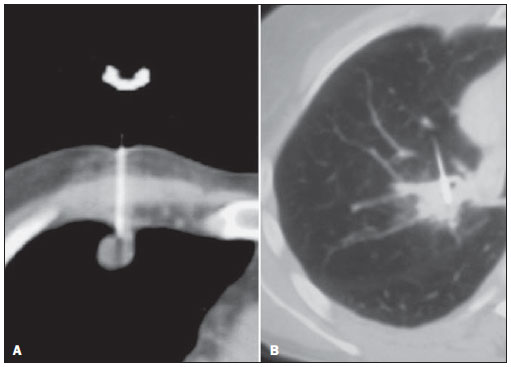
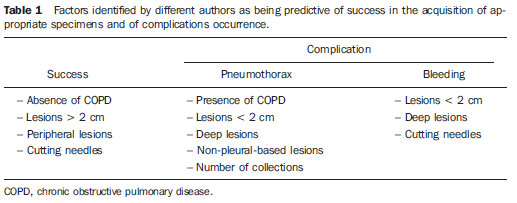
In the lungs, percutaneous biopsy by means of fine needle aspiration biopsy (FNAB) or by cutting needle (CNB) has become one of the main choices for the investigation of nodules and masses. The versatility of such a method allows the access to lesions in different lung locations, being utilized both for peripheral and deep lesions, even in cases where such lesions are rather small(2) (Figure 1).
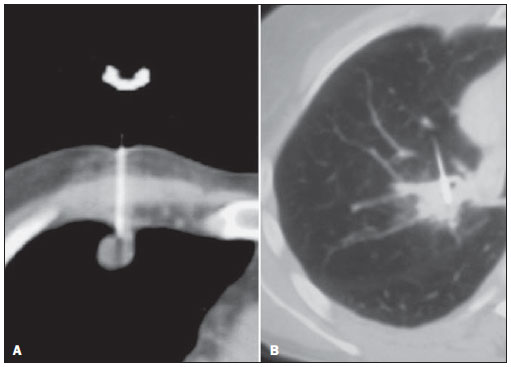
Figure 1. Computed tomography-guided transthoracic needle biopsy of pulmonary nodules. Lesions, needles and their interaction have excellent visualization at computed tomography. A: Peripheral pleuralbased nodular lesion measuring 10 mm. B: Central lesion measuring 20 mm.
In the present article the authors discuss indications, technical aspects of the procedure and expected success and complication rates of percutaneous biopsies of lung nodules and masses.
DISCUSSION
1. Indications
Percutaneous biopsies of lung nodules and masses are performed in various clinical settings, preferably in cases of peripheral lesions not easily accessible at bronchoscopy or in cases of central lesions in patients who have previously undergone non diagnostic bronchoscopy.
Pulmonary nodules
Pulmonary nodules may be either incidentally identified or identified at routine assessments and be considered suspicious for primary lung cancer based on the patients’ clinical history and radiological findings. In such cases, the biopsy may be useful in the approach to the disease in various different ways. In cases of lesions with low malignancy probability, the documentation of benignity by means of percutaneous biopsy can spare the patient more invasive procedures, such as thoracoscopy or thoracotomy. In cases of lesions highly suggestive of malignancy, biopsy is most frequently utilized for diagnostic documentation in patients who either refuse or do not present conditions to tolerate more invasive procedures.
Pulmonary nodules identified in patients with primary malignant neoplasias in other organs may be submitted to percutaneous biopsy whenever it is necessary to document metastatic disease, immunohistochemical study to support the definition of the therapeutic approach definition, or in cases where there is the possibility of the pulmonary nodule being a second primary or secondary neoplasm(3).
Pulmonary masses
In determined clinical contexts, pulmonary masses with certain radiological characteristics are strongly suggestive of primary lung neoplasia, and, as such lesions are often followed by unequivocal signs of locally advanced or metastatic disease, percutaneous biopsy may be performed to determine the histologic type of the neoplasm to allow the adoption of the appropriate non surgical treatment.
Occasionally, percutaneous biopsy is requested in order to define the nature of radiological findings that are suspicious for tumor recurrence, or to establish the molecular profile of a previously diagnosed neoplasm, with the purpose of refining the indication of chemotherapy agents or targeted therapies(3).
2. Technical aspects
In most of centers, percutaneous biopsy is performed by radiologists or interventional radiologists. The patients referred for the procedure are generally under clinical care by physicians or surgeons who at some point request the percutaneous biopsy.
Preprocedural assessment
Some aspects are important for the assessment of the patient candidate for percutaneous biopsy as well as of the pulmonary lesion to be approached. Ideally, such an assessment should be performed during a preceding consultation. In such an opportunity it is possible to provide the patient with information on the procedure’s inherent risks and characteristics.
Clinical issues that should be assessed previously to the procedure include: general patient status, consciousness level, pulmonary functional reserve, coagulation activity and the patient ability to follow instructions regarding breathing and breath hold(3,4).
Small pulmonary lesions are hardly accessible in poorly cooperative patients or those who are under sedation. In such cases, tracheal intubation and induced apnea may be necessary to allow percutaneous approach to the lesion.
The most frequent complication of percutaneous lung biopsies is pneumothorax. Generally, such a complication is easily controllable; however patients with chronic obstructive pulmonary disease (COPD), poor pulmonary reserve (FEV
1 < 35%) or with a single lung, may face severe consequences. A careful risk-benefit analysis must be performed in such cases and, as the procedure is performed, all the necessary conditions to allow immediate management of complications should be available.
Appropriate coagulation activity levels are required to minimize bleedings in percutaneous biopsy, and anticoagulant agents should be discontinued. Typically, a four-day anticoagulant therapy interruption period is necessary; however it is important to coordinate such a strategy with the assisting physician who is following up the anticoagulant therapy. A coagulation test must be performed up to one week prior to the procedure in patients with no suspicion of coagulopathy, or within a shorter period in patients submitted to interruption of anticoagulant therapy(3,5). Prothrombin time, activated partial thromboplastin time and platelet count must be assessed before the procedure; platelet count < 100,000/ml and prothrombin or thromboplastin time ratios above the 1.4 standard are considered as relative contraindications. In such situations, a risk-benefit analysis must be performed(4,6,7).
Lesion characteristics such as location, size and distance from the skin may affect success and complication rates or increase procedure times, and must be taken into consideration on the risk-benefit assessment prior to the procedure(6).
Additionally, a careful evaluation of the clinical and radiological context of the indication as well as of the presence of more easily approachable lesions in other sites, besides the possibility of utilizing other less invasive diagnostic methods, should always be carried out.
Procedure
A term of free and informed consent must be obtained before the procedure, and the patients are instructed to fast for four hours prior to the procedure on account of the utilization of anesthetics and eventually intravenous contrast agents.
Whenever possible, the biopsy is performed on an outpatient basis and without sedation(3,4).
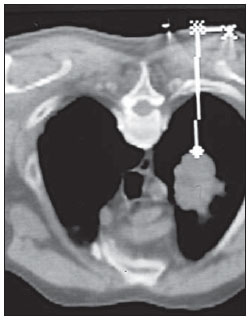
Based on previous studies, the patient is positioned in a decubitus that best allows a more direct access to the lesion. A series of images are then acquired for the planning of an entry point, pathway and calculation of the distance between the entry point and the lesion (Figure 2). Whenever possible, pathways minimizing the passage of the needle through aerated lung parenchyma should be selected in order to reduce the risk for pneumothorax(3). After asepsis and local anesthesia down to the pleura (lidocaine 2%), the needle is introduced as planned. Such a maneuver can be followed up in real time by means of apparatuses equipped with CT-fluoroscopy.
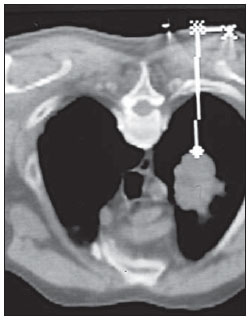
Figure 2. Tomographic section identifying metal marker attached to patient’s skin and pulmonary lesion allowing the planning of entry point and needle pathway by means of cursors.
For smaller or hardly accessible lesions, the coaxial approach technique may be utilized. Such a technique consists of the insertion of a cannula with a central rigid rod (mandrel) into the lesion. The mandrel is then removed, and the biopsy needle is then inserted through the cannula to collect the specimen. Thus multiple collections may be performed through the cannula(3). Once the needle is positioned, new tomographic images are acquired in order to confirm its position in relation to the lesion. Then, the specimen is collected.
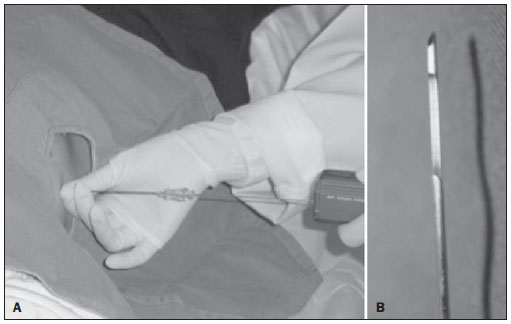
In cases of FNAB, Chiba type needles 22-25-gauge are utilized and the collection is performed by means of the aspiration technique, with back-and-forth movements and negative pressure. The collected material may be prepared in smears and fixed in alcohol or deposited in a fluid medium (Figure 3).

Figure 3. A: Fine needle aspiration puncture technique utilizing negative pressure and back-and-forth movements B: Chiba type fine needle utilized in fine needle aspiration puncture.
In the cases of CNB, 18-20-gauge cutting needles with an automatic biopsy system are utilized. Generally, the obtained fragments are preserved in a formaldehyde 10% solution (Figure 4).
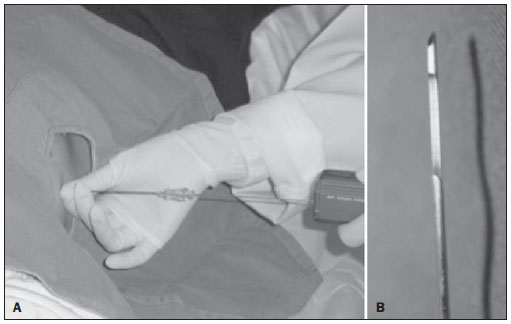
Figure 4. A: Cutting needle (tru-cut) biopsy coupled with automatic spring-activated triggering system. B: Detail of the cutting needle extremity with a lateral cutting section for specimen collection.
The number of collections may vary for both types of needles. The following factors may influence such number: difficulties in the procedure, occurrence of complications, specimen’s quality, and required type of pathological analysis. Typically, two or three specimens are collected.
The immediate analysis of the specimens by a cytopathologist is recommended by some authors in cases of FNAB. Such a recommendation is aimed at increasing the biopsy success rate and at reducing the number of collected specimens, as this technique allows the confirmation of the specimen appropriateness from the first puncture. On the other hand, besides requiring the availability of such a professional, the immediate analysis determines an increase in the total procedure time. With some experience, a higher number of collections can produce comparable results, without an increase in complication indices(8).
Post-procedural care
After the procedure, further images are acquired in order to evaluate the presence of possible complications such as pneumothorax or hemorrhage. Patients with no signs of complications are monitored for one hour and are released after confirmation of hemodynamic and respiratory stability and chest radiography confirming the absence of pneumothorax. Late complications rarely occur and patients must be instructed to seek medical assistance in the event of dyspnea or hypotension(3,4,7).
3. Results
Success indices
The literature presents a significant variation in reported accuracy indices in percutaneous biopsy of lung lesions. Many studies report accuracy above 90%.
Success indices in the collection of appropriate specimens for analysis and in the achievement of specific diagnosis by means of percutaneous biopsy may vary due to several factors such as patient’s characteristics, experience of the service, type of needle and lesion characteristics(2).
Among the main factors considered as being predictive of a higher success index in obtaining a diagnosis by means of percutaneous biopsy, one can mention the absence of COPD, large dimensions of the lesion (> 2 cm), peripheral lesion location and utilization of cutting needles (CNB)(1,2,9).
Needle selection
One of the most studied factors in the analysis of percutaneous biopsy accuracy is the influence of the utilized needle type. In general, cutting needles utilized in CNBs present higher accuracy indices. However, the differences in accuracy should be evaluated in greater detail.
Most studies report high specificity and reliability on results positive for malignancy for both types of needles, with rare cases of false-positive results(1,10,11).
False-negative results are most frequent, and for such an occurrence, reported results for different types of needles are clearly different.
Fine Chiba type aspiration needles utilized in the collection of specimens for cytological analysis (FNAB) present a higher false-negative index as compared with cutting needles, and depending on the malignancy prevalence in the studied population, such an index may reach up to 50%(1,10–12).
In cases of benign lesions, more reliable results are obtained by means of cutting needles (tru-cut), since they allow obtaining the specimens for histological analysis with false-negative results generally below 10%(1,10,11,13).
Therefore, positive results in cases of lesions highly suspicious for malignancy are reliable with both types of needles; however, a negative result obtained with fine needles (FNAB) must be carefully analyzed, and a new collection should be considered.
For a reliable definition of absence of malignancy, as in the case of low-suspicion solitary nodular lesions, or for the definition of a specific diagnosis of benignity, the utilization of cutting needles should be prioritized(13).
In general, satisfactory success indices in obtaining appropriate specimens for analysis are those above 85%. Sensitivity indices for malignancy are also generally above 85%. And false-positive results are extremely rare and lower than 1%.
In the previous experience reported by the authors, the success indices achieved in obtaining appropriate specimens by FNAB remained in the range between 84% and 88% along the years, and with cutting needles, between 95% and 97%(1,2,10,11,14). Specific histological results were also more frequently obtained with cutting needles(1,2,10,11,14). Some factors associated with higher success indices in the present casuistry include lesions with dimensions > 40 mm, located in the upper lobes and suspicious for malignancy.
Currently, based on the presented results and accumulated experience, the authors perform all the procedures with 18-20-gauge cutting needles. Fine needles are reserved for situations in which the patient present coagulopathy. And, under ideal conditions, the authors perform three specimen collections.
Complications
In the literature, the variation of complication rates reported for percutaneous biopsy of pulmonary lesions is also considerable(4).
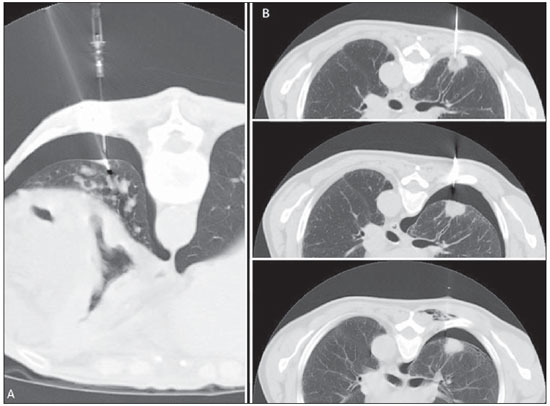
Minor complications such as mild focal hemorrhage, pain and vasovagal reaction rarely occur, but are easily resolved. Pneumothorax is the most frequent moderate complication, most of times not requiring chest drainage. Several strategies may be adopted in the management of pneumothorax identified during or after the procedure, varying with the patient’s clinical status, symptoms, dimensions of the pneumothorax and available homecare conditions(4,7,15) (Figure 5).
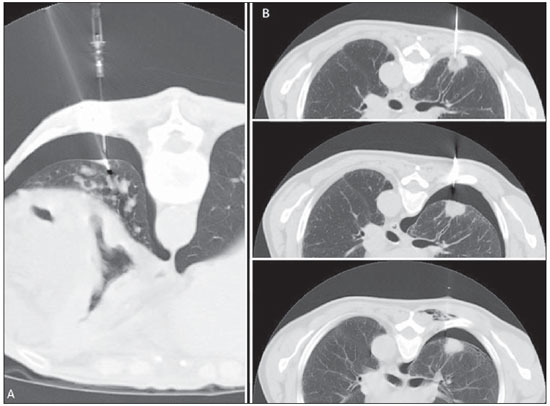
Figure 5. Pneumothorax management techniques. A: Computed tomography section simultaneously depicting pneumothorax, a relief drain and the biopsy needle. The management of the symptoms of the pneumothorax developed during the procedure allows the continuity of the biopsy. B: Images series acquired during the procedure, demonstrating pneumothorax and after its aspiration by means of a fine needle, which many times avoids drainage.
Reported rates of pneumothorax occurrence range from 0% to 61%, and from 3% to 15% for necessity of chest drainage(4).
Factors such as presence of COPD, non-pleural-based lesions, greater depth and small lesion dimensions have been associated with increased risk for development of pneumothorax(4,14,16).
Historically, CNB has been associated with a higher risk for pneumothorax. Much of the data on this subject is based on the utilization of large gauge needles without automatic biopsy systems. Most recent studies have demonstrated rates of occurrence of pneumothorax similar to those reported for fine needle aspiration (FNAB).
Generally, with some experience, pneumothorax and drainage indices should be close to 20% and 5% respectively. Lower indices may be expected in cases of pleural-based lesions > 2 cm and absence of COPD.
Some post-procedural actions, such as positioning the patient over the needle entry point, autologous blood injection into the needle pathway and aspiration of pneumothorax, are adopted by some authors to reduce the pneumothorax index, however the benefit of such actions is still uncertain(17).
Severe hemorrhagic complications are rare, and even rarer cases of death have been reported. The mortality rate is difficult to be established, but in a multicentric study it was estimated to be 0.15%(18).
Table 1 lists the factors identified as predictive of success in the collection of appropriate specimens and the factors most frequently identified as related to relevant complications.
Physicians involved in the performance of percutaneous biopsies must be properly trained to deal with complications, and resuscitation and chest drainage materials must be easily accessible.
In the authors’ practice, pneumothorax indices ranging between 11% and 16% were identified, with necessity of drainage occurring in 2% to 5% of cases where fine needles were utilized. In cases where cutting needles were utilized, such indices were even lower(1,10,14). In spite of the fact that such data were obtained from different casuistries, the complication indices for both types of needles are similar, as already reported by other authors(4,6,12,15). In a retrospective analysis, the authors have identified only the absence of a lesion pleural contact as a predictive factor for the occurrence of pneumothorax.
In the authors’ practice, as the presence of pneumothorax is identified during the procedure, they go ahead with the specimen collection whenever possible and aspiration or a relief drain is utilized in order to stabilize the patient and conclude the collection (Figure 5).
The post-procedural care is adapted on a case-by-case basis. Patients with no sign of complications or with asymptomatic mild pneumothorax are generally monitored for one hour, and are subsequently released. Patients with more severe or symptomatic pneumothorax may remain under observation or be submitted to aspiration or placement of a chest drain.
4. Conclusion
Percutaneous biopsies constitute an indispensable procedure in the practice of thoracic oncology. By means of such a procedure, diagnostic problems can be quickly solved at radiology and pathology departments, most of times avoiding more invasive procedures. Developments in imaging techniques and biopsy needles, and enhancement of operators’ experience have led such procedure to become more versatile, safe and accurate thus expanding its indications.
REFERENCES
1. Chojniak R, Isberner RK, Viana LM, et al. Computed tomography guided needle biopsy: experience from 1,300 procedures. Sao Paulo Med J. 2006;124:10–4.
2. Guimarães MD, Chojniak R, Gross JL, et al. Predictive success factors for CT-guided fine needle aspiration biopsy of pulmonary lesions. Clinics (Sao Paulo). 2009;64:1139–44.
3. Wu CC, Mather MM, Shepard JA. CT-guided percutaneous needle biopsy of the chest: preprocedural evaluation and technique. AJR Am J Roentgenol. 2011;196:W511–4.
4. Manhire A, Charig M, Clelland C, et al. Guidelines for radiologically guided lung biopsy. Thorax. 2003;58:920–36.
5. Baglin TP, Keeling DM, Watson HG; British Committee for Standards in Haematology. Guidelines on oral anticoagulation (warfarin): third edition – 2005 update. Br J Haematol. 2006;132:277–85.
6. Topal U, Ediz B. Transthoracic needle biopsy: factors effecting risk of pneumothorax. Eur J Radiol. 2003;48:263–7.
7. Aviram G, Schwartz DS, Meirsdorf S, et al. Transthoracic needle biopsy of lung masses: a survey of techniques. Clin Radiol. 2005;60:370–4.
8. Küçük ÇU, Yilmaz A, Yilmaz A, et al. Computed tomography-guided transthoracic fine-needle aspiration in diagnosis of lung cancer: a comparison of single-pass needle and multiple-pass coaxial needle systems and the value of immediate cytological assessment. Respirology. 2004;9:392–6.
9. Laurent F, Latrabe V, Vergier B, et al. CT-guided transthoracic needle biopsy of pulmonary nodules smaller than 20 mm: results with an automated 20-gauge coaxial cutting needle. Clin Radiol. 2000;55:281–7.
10. Yu LS, Deheinzelin D, Younes RN, et al. Computed tomography-guided cutting needle biopsy of pulmonary lesions. Rev Hosp Clin Fac Med Sao Paulo. 2002;57:15–8.
11. Guimaraes MD, de Andrade MQ, da Fonte AC, et al. CT-guided cutting needle biopsy of lung lesions – an effective procedure for adequate material and specific diagnose. Eur J Radiol. 2010 Oct 26. [Epub ahead of print].
12. Anderson JM, Murchison J, Patel D. CT-guided lung biopsy: factors influencing diagnostic yield and complication rate. Clin Radiol. 2003;58:791–7.
13. Gong Y, Sneige N, Guo M, et al. Transthoracic fine-needle aspiration vs concurrent core needle biopsy in diagnosis of intrathoracic lesions: a retrospective comparison of diagnostic accuracy. Am J Clin Pathol. 2006;125:438–44.
14. Guimarães MD, Andrade MQ, Fonte AC, et al. Predictive complication factors for CT-guided fine needle aspiration biopsy of pulmonary lesions. Clinics (Sao Paulo). 2010;65:847–50.
15. Gohari A, Haramati LB. Complications of CT scan-guided lung biopsy: lesion size and depth matter. Chest. 2004;126:666–8.
16. Yeow KM, Su IH, Pan KT, et al. Risk factors of pneumothorax and bleeding: multivariate analysis of 660 CT-guided coaxial cutting needle lung biopsies. Chest. 2004;126:748–54.
17. Collings CL, Westcott JL, Banson NL, et al. Pneumothorax and dependent versus nondependent patient position after needle biopsy of the lung. Radiology. 1999;210:59–64.
18. Tomiyama N, Yasuhara Y, Nakajima Y, et al. CT-guided needle biopsy of lung lesions: a survey of severe complication based on 9783 biopsies in Japan. Eur J Radiol. 2006;59:60–4.
1. PhD, MD, Radiologist, Director, Imaging Department of Hospital A. C. Camargo, São Paulo, SP, Brazil.
2. Masters, MDs, Radiologists, Imaging Department of Hospital A. C. Camargo, São Paulo, SP, Brazil.
3. PhD, MD, Radiologist, Imaging Department of Hospital A. C. Camargo, São Paulo, SP, Brazil.
4. Fellow PhD degree, MD, Radiologist, Hospital A. C. Camargo, São Paulo, SP, Brazil.
Mailing Address:
Dr. Rubens Chojniak
Hospital A. C. Camargo
Rua Professor Antônio Prudente, 211, Liberdade
São Paulo, SP, Brazil, 01509-010
E-mail: chojniak@uol.com.br
Received March 28, 2011.
Accepted after revision May 24, 2011.
Study developed at Hospital A. C. Camargo, São Paulo, SP, Brazil.
 Vol. 44 nº 5 - Sep. / Oct. of 2011
Vol. 44 nº 5 - Sep. / Oct. of 2011