Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 5 - Sep. / Oct. of 2011
Vol. 44 nº 5 - Sep. / Oct. of 2011
|
CASE REPORT
|
|
Granular cell tumor with orbital involvement in a child |
|
|
Autho(rs): Fabiano Reis1; Josie Naomi Iyeyasu2; Albina Messias Altemani3; Keila Monteiro de Carvalho4 |
|
|
Keywords: Orbit; Granular cell tumor. |
|
|
Abstract: INTRODUCTION
Granular cell tumor is a rare, generally benign tumor which can affect any part of the body, with the orbit being a rather infrequent site, and affecting primarily women after the third decade of life. Its diagnosis is based upon imaging studies (computed tomography and magnetic resonance imaging) and upon the anatomopathologic analysis of the lesion. The treatment is surgical with a good prognosis in most cases. On the following paragraphs, the authors describe a case of granular cell tumor in a seven-year old boy. CASE REPORT A seven-year old boy with one-year history of proptosis of his left eye. Computed tomography demonstrated homogeneous fusiform enlargement of the left medial rectus muscle (Figure 1). 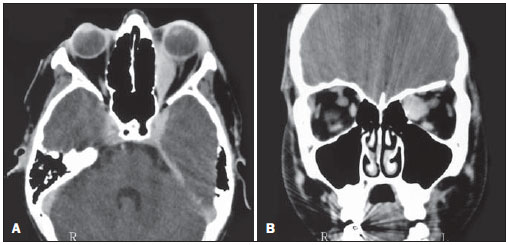 Figure 1. Computed tomography. A: Axial section showing proptosis and fusiform enlargement of the left medial rectus muscle with tendinous involvement. B: Coronal view demonstrating enlarged left medial rectus muscle. At ophthalmological examination, the patient presented 20/20 visual acuity in both eyes and proptosis of the left eye. Versions and ductions showed left medial rectus muscle movement restriction (–4). At slit lamp biomicroscopy, it was possible to observe the presence of a subconjunctival mass on the left medial rectus muscle. Fundoscopy demonstrated increased venous tortuosity in the left eye. Neurological examination did not demonstrate any other abnormalities. Transconjunctival biopsy of the lesion demonstrated the presence of a granular cell tumor in the left medial rectus muscle (Figure 2). 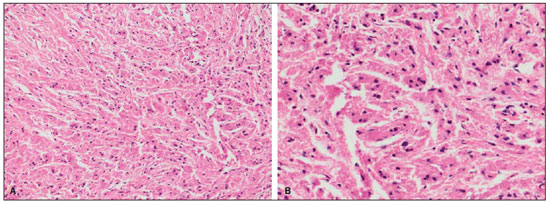 Figure 2. Granular cell tumor. Anatomopathologic study demonstrating cells with abundant rose granular cytoplasm and small eccentric nuclei (hematoxylineosin stain, 200x and 400x magnification). Immunohistochemical analysis was positive for myoglobin and S-100 protein, and negative for NSE. The patient was submitted to frontal craniotomy for total tumor resection with good outcome. DISCUSSION Granular cell tumor, also known as myoblastoma, was first described by Abrikossoff in 1926(1). It is a rare tumor that can affect any part of the body, with highest prevalence between the third and sixth decades of life and highest frequency among women(2). The most frequently affected sites are the following: tongue, subcutaneous tissues(1), larynx, gastrointestinal tract, breasts, pituitary stalk and the anogenital region(2). Ocular involvement is rarely observed and as it happens, the sites most frequently involved are orbit, skin of the periorbital area, lacrimal sac, eyelids, extraocular muscles, ciliary body, conjunctiva and caruncle(1). The most common symptoms include exophthalmos, diplopia and decreased visual acuity (in cases where the optic nerve is affected)(1). In the past, before the confirmation of the neoplastic nature of this condition, it was believed that such lesions resulted from a post-traumatic degenerative and/or regenerative process, infection or any other tissue aggression. The histogenesis of granular cell tumor is not yet fully understood(1), in spite of several studies suggesting its neural crest origin(2), more specifically from the Schwann cells(3). The granular cell tumor is generally benign. The malignant presentation is extremely rare (1% to 3% of cases)(1), and the tumor may be multicentric in some cases (10% to 15% of cases)(2). Malignant transformation is suspected in cases where the patient is at older ages at the moment of the diagnosis and where there is a several-year-long history of a nodular lesion with recently accelerated growth(3). The most common sites of metastasis are regional lymph nodes, bones, peripheral nerves, the peritoneal cavity and lungs(4). Lesion biopsy is essential for the differentiation between the benign and malignant presentations of the disease. At microscopy, the tumor is seen as a group of large, elongated, polygonal cells, or as irregular cells with small nuclei(5), whose cytoplasm contains PAS-positive granules. Mitosis is uncommon(5). Immunoperoxidase study is positive for S-100 protein and desmin. Electron microscopy shows numerous degenerative intracellular myelin bodies(6). At the moment of the diagnosis, the radiological study may be negative, particularly in cases of small tumors with signal intensity similar to of that of adjacent tissues(4). In cases where the radiological study is positive, computed tomography demonstrates a well defined mass with soft tissue density, as in the present case. At magnetic resonance imaging, some studies describe granular cell tumor as an isointense homogeneous lesion on T1-weighted images and iso/hypointense lesion on T2-weighted images, as compared with adjacent tissues, while others describe it as a hypointense lesion on T1-weighted images(4). There is a consensus that the lesion is enhanced after intravenous injection of paramagnetic contrast agent(2,4), which is a typical finding of such type of tumor(4). The treatment consists of complete surgical excision with tumor-free margins(3), with adjuvant postoperative radiotherapy and chemotherapy in cases of malignancy(3). Tumor recurrence is rare(5). The authors have considered the present case as a rare occurrence, since the tumor affected a seven-year old boy and, according to previous studies, such disease is most prevalent among women, after the third decade of life. REFERENCES 1. Ahdoot M, Rodgers IR. Granular cell tumor of the orbit: magnetic resonance imaging characteristics. Ophthal Plast Reconstr Surg. 2005;21:395–7. 2. Poyraz CE, Kiratli H, Söylemezolu F. Granular cell tumor of the inferior rectus muscle. Korean J Ophthalmol. 2009;23:43–5. 3. Golio DI, Prabhu S, Hauck EF, et al. Surgical resection of locally advanced granular cell tumor of the orbit. J Craniofac Surg. 2006;17:594–8. 4. Boulos R, Marsot-Dupuch K, De Saint-Maur P, et al. Granular cell tumor of the palate: a case report. AJNR Am J Neuroradiol. 2002;23:850–4. 5. Moseley I. Granular cell tumour of the orbit: radiological findings. Neuroradiology. 1991;33:399–402. 6. Rodríguez-Ares T, Varela-Durán J, Sánchez-Salorio M, et al. Granular cell tumor of the eye (myoblastoma): ultrastructural and immunohistochemical studies. Eur J Ophthalmol. 1993;3:47–52. 1. Docent and Professor at Department of Radiology, Faculdade de Ciências Médicas – Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. 2. MD, Ophthalmologist, Fellow Master degree in Ophthalmology, Department of Ophthalmo-otorhinolaryngology, Faculdade de Ciências Médicas – Universidade Estadual de Campinas (FCMUnicamp), Campinas, SP, Brazil. 3. Docent and Professor at Department of Anatomic Pathology, Faculdade de Ciências Médicas – Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. 4. Docent and Professor at Department of Ophthalmo-otorhinolaryngology, Faculdade de Ciências Médicas – Universidade Estadual de Campinas (FCM-Unicamp), Campinas, SP, Brazil. Mailing Address: Dr. Fabiano Reis Hospital de Clínicas da Universidade Estadual de Campinas (HC-Unicamp) Rua Vital Brasil, 251, Cidade Universitária Zeferino Vaz. P.O.Box 6142 Campinas, SP, 13083-888, Brazil E-mail: fabianoreis2@ gmail.com Received April 13, 2011 Accepted after revision May 30, 2011. Study developed at Hospital de Clínicas da Universidade Estadual de Campinas (HC-Unicamp), Campinas, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554