Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 5 - Sep. / Oct. of 2011
Vol. 44 nº 5 - Sep. / Oct. of 2011
|
CASE REPORT
|
|
Chilaiditi’s syndrome: a case report |
|
|
Autho(rs): Rachid Guimarães Nagem1; Henrique Leite Freitas2 |
|
|
Keywords: Chilaiditi’s syndrome; Chilaiditi’s sign; Acute abdomen; Pneumoperitoneum; Hepatodiaphragmatic space. |
|
|
Abstract: INTRODUCTION
Chilaiditi’s syndrome refers to either temporary or permanent interposition of the colon or small bowel in the hepatodiaphragmatic space, causing symptoms. The isolated and asymptomatic presentation of such a condition is known as Chilaiditi’s sign. Such sign was first described in 1865 by Cantini who observed it at clinical examination, but only in 1910, with the publication of a study reporting three cases, by Demetrius Chilaiditi, it was consolidated as a radiological diagnosis(1). The incidence of such finding at radiography is between 0.025% and 0.28% including all the age ranges, with a slight increase in individuals aged above 60 years, being most frequently found in men than in women at a 4:1 ratio(2,3). The association of Chilaiditi’s sign with symptoms such as abdominal pain, nauseas, retrosternal pain, respiratory symptoms, vomiting, abdominal distension, intestinal obstruction or subocclusion characterizes Chilaiditi’s syndrome. CASE REPORT A female, 56-year-old patient was admitted to the unit of immediate assistance presenting abdominal pain in the previous eight hours. The patient reported intense pain in the epigastrium and in the right shoulder. Because of the pain intensity, she could not keep herself in dorsal decubitus for clinical examination. The admission examination revealed normal breath sounds, tachypnea (respiratory rate = 32 rpm), tachycardia (heart rate = 116 bpm), broad and symmetrical pulse waveforms, blood pressure 130 × 90 mmHg. Tense, painful abdomen, no sign of peritoneal irritation and preserved hydroaerial noise were observed. Tests were immediately requested, with the following results: amylase, 94; negative PCR; Na, 146; Cl, 107; K, 4.3; leukogram: 7,100 (0% rod neutrophils); normal sinusal rhythm at ECG, without ST segment elevation or depression. Plain chest radiography in orthostasis (Figure 1) demonstrated hyper transparency in the right hepatodiaphragmatic region, suggesting the presence of pneumoperitoneum.  Figure 1. Chest radiography in orthostasis demonstrating the presence of air within the right hepatodiaphragmatic space. The patient was referred to the Hospital Regional de Betim with diagnosis of acute abdomen secondary to a perforated viscus, and underwent a new abdominal radiography that suggested the presence of colon interposition between the liver and the diaphragm (Figure 2). Abdominal ultrasonography was subsequently performed (Figure 3), but neither free fluid nor other abnormalities were observed. At that first moment, exploratory laparotomy was ruled out. The patient was kept with no analgesia, under fasting and intravenous fluids, and abruptly presented complete pain relief, at approximately 24 hours from the pain onset. A further chest radiography (Figure 4) did not demonstrate the previous image of right subphrenic hyper transparency. The patient was discharged with recommendations for follow-up on an outpatient basis. 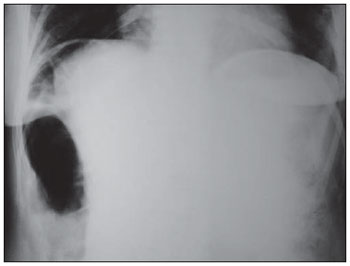 Figure 2. Abdominal radiography confirms the presence of air in the right subphrenic space, probably corresponding to a hollow viscus (colon). 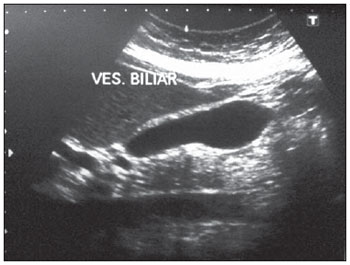 Figure 3. Abdominal ultrasonography ruled out the presence of free fluid or any other abnormality. 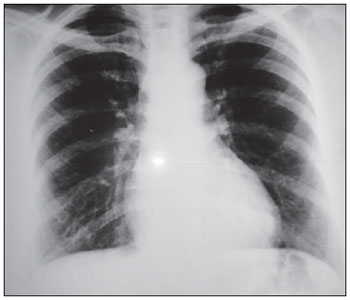 Figure 4. A further chest radiography demonstrates the disappearance of the image of air within the hepatodiaphragmatic space. DISCUSSION Hepatodiaphragmatic interposition of hollow viscera, colon or bowel, described in 1910 by Chilaiditi(4), is a rare entity that is generally incidentally found at imaging studies, with an incidence of up to 0.3% at plain chest radiography and 2.4% at chest/abdominal computed tomography(5). In cases where such a sign is found in association with symptoms such as pain, nauseas, dyspepsia and vomiting, it is called Chilaiditi’s syndrome(6). Its cause still remains unknown, but it is probably multifactorial. Several conditions may facilitate the Chilaiditi’s syndrome onset as they change the anatomical relationship between the liver, colon and diaphragm. Such predisposing factors may be divided into hepatic (liver ptosis caused by relaxation of ligaments, cirrhosis, hepatic atrophy, ascites), intestinal (megacolon, meteorism, abnormal colonic motility), and diaphragmatic (diaphragmatic thinning, phrenic nerve injury, changes in intrathoracic pressure as in cases of emphysema)(7–9). In healthy individuals, Chilaiditi’s syndrome is generally attributed to an increase in the length, diameter and motility of the colon. A Greek study with 1,440 patients submitted to chest/abdominal computed tomography has demonstrated the increase in the intra-abdominal fat as the factor most frequently associated with the Chilaiditi’s sign(5). The great relevance of Chilaiditi’s syndrome resides in its differential diagnosis with conditions that run their course with pneumoperitoneum which generally imply immediate surgical intervention. Other diagnosis to be ruled out is subphrenic abscess. If doubt persists after plain chest radiography, it should be supplemented by lateral views (haustration is better visualized on lateral views) and by left lateral decubitus views with horizontal X-ray beam angulation. On the latter, the free air tends to remain in the subphrenic space. Other imaging methods indicated for the differential diagnosis of Chilaiditi’s syndrome include the opaque enema technique and chest/abdominal computed tomography, this latter being considered as the method with highest diagnostic accuracy(5,8). The treatment for Chilaiditi’s syndrome is generally conservative, including weight loss, management of aerophagia and ascites, and change in decubitus. Rarely, surgical approach may be required, with resection or, most commonly, fixation of the interposed viscus. Cases of volvulus generally require urgent surgical intervention with either colectomy (perforation and gangrene) or colopexy. Because of the lower intensity of postoperative pain, minor complications related to the surgical incision, shorter hospital stay and earlier return to activity, the laparoscopic approach has gained the surgeons’ preference(1,2,9,10). REFERENCES 1. Barroso Jornet JM, Balaguer A, Escribano J, et al. Chilaiditi’s syndrome associated with transverse colon volvulus: first report in a pediatric patient and review of the literature. Eur J Pediatr Surg. 2003;13:425–8. 2. Kamiyoshihara M, Ibe T, Takeyoshi I. Chilaiditi’s sign mimicking a traumatic diaphragmatic hernia. Ann Thorac Surg. 2009;87:959–61. 3. Prieto-Díaz-Chávez E, Marentes EJ, Medina CJ, et al. Síndrome de Chilaiditi como un problema de decisión quirúrgica: reporte de un caso y revisión de la literatura. Cir Gen. 2007;29:294–6. 4. Chilaiditi D. Zur Frage der Hepatoptose und Ptose im allgemeinen im Anschluss an drei falle von temporarae, partiellae Leberverlagerung. Fortschr Geb Rontgenstr Nuklearmed. 1910;16:173–208. 5. Prassopoulos PK, Raissaki MT, Gourtsoyiannis NC. Hepatodiaphragmatic interposition of the colon in the upright and supine position. J Comput Assist Tomogr. 1996;20:151–3. 6. Jackson ADM, Hodson CJ. Interposition of the colon between liver and diaphragm (Chilaiditi’s syndrome) in children. Arch Dis Child. 1957;32:151–8. 7. Duarte MA, Carvalho AST, Penna FJ, et al. Síndrome de Chilaidite na infância (interposição hepato-diafragmática do colo) – relato de cinco casos. Pediatr (S. Paulo). 1983;5:379–82. 8. Farkas R, Moalem J, Hammond J. Chilaiditi’s sign in a blunt trauma patient: a case report and review of the literature. J Trauma. 2008;65:1540–2. 9. Sorrentino D, Bazzocchi M, Badano L, et al. Heart-touching Chilaiditi’s syndrome. World J Gastroenterol. 2005;11:4607–9. 10. Nurdjanah S, Bayupurnama P, Maduseno S, et al. Abdominal malignant fibrous histiocytoma infiltrating stomach with Chilaiditi’s sign manifestation (a rare case report). Kobe J Med Sci. 2007;53:119–24. 1. MD, MCh, Coordinator for the General Surgery Service of Hospital Regional de Betim, Betim MG, Brazil. 2. MD, Resident of General Surgery at Hospital Regional de Betim, Betim MG, Brazil. Mailing Address: Dr. Rachid G. Nagem Rua Gonçalves Dias, 332, ap. 1001, Bairro Funcionários Belo Horizonte, MG, Brazil, 30140-090 E-mail: rgnagem@yahoo.com.br Received February 27, 2011. Accepted after revision April 18, 2011. Study developed at Hospital Regional de Betim, Betim MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554