Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 4 - July / Aug. of 2011
Vol. 44 nº 4 - July / Aug. of 2011
|
CASE REPORT
|
|
Color Doppler of Meckel’s diverticulum: report of two cases |
|
|
Autho(rs): Mariana Damian Mizerkowski1; José Vicente Noronha Spolidoro2; Matias Epifanio3; João Cyrus Bastos4; Matteo Baldisserotto5 |
|
|
Keywords: Meckel’s diverticulum; Color Doppler; Ultrasonography. |
|
|
Abstract: INTRODUCTION
Meckel's diverticulum (MD) is found in 2-3% of the population and is the most common congenital abnormality of the gastrointestinal tract, and hemorrhage is the most frequent complication(1). At B-mode ultrasonography (US), MD appears as a cyst-like, tubular-shaped or tear-drop-shaped structure, with the so called gut signature(2,3). Scintigraphy, US and computed tomography (CT) may be utilized for detecting complications(2-7). Color Doppler US may demonstrate parietal hyperemia in an inflamed MD(3,4). The authors describe two cases of complicated MD detected at US, whose findings were different from the cases described in the literature: hemorrhagic MD without parietal hyperemia at color Doppler, and the other, a perforated MD detected at color Doppler US with no sign of inflammation. CASES REPORT Case 1 A two-year-old boy admitted to the emergency department for painless hematochezia for two days. Laboratory tests demonstrated hemoglobin = 7.6 mg/dl; platelets = 432,000/mm3, without leukocytosis. Clinical examination did not demonstrate any significant alteration. At B-mode US, a cystic image with gut signature was identified in the lower right abdominal quadrant (Figure 1A). During the examination, the cyst emptied itself after contractions. Parietal thickening of the distal ileum and enlarged mesenteric lymph nodes were observed. Color Doppler US did not demonstrate any sign of hyperemia of the cystic wall (Figure 1B). The presence of one MD was confirmed by Tc-99m scintigraphy (Figure 1C). 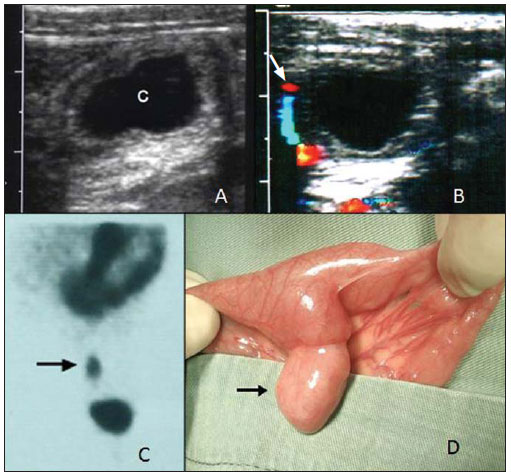 Figure 1. A: B-mode US: cystic structure (C) in the right lower abdominal quadrant. B: Color Doppler US did not detect the presence of vessels on the walls of the cystic structure. The vascular structure (arrow) is the adjacent mesenteric artery. C: Radiopharmaceutical uptake by the MD at scintigraphy. D: Surgical specimen showing MD on the antimesenteric border of the ileum (arrow). At the fourth day of hospitalization, a MD was localized in the terminal ileum and was resected (Figure 1D). Anatomopathological study of the surgical specimen revealed gastric and enteric mucosa in the MD without inflammation or ulcerations. Three days postoperatively, the patient was uneventfully discharged. Case 2 A 15-year-old boy presenting blood in stools for one month. Four days after the symptoms onset, the patient underwent rectosigmoidoscopy which revealed the presence of stale blood in the rectosigmoid junction. Serum hemoglobin level was 11 mg/dl. History of appendectomy three years before. At color Doppler US, a fixed cystic image with gut signature was observed in the right lower abdominal quadrant, with no sign of parietal hyperemia or inflammation (Figure 2A). The Tc-99m scintigraphy was inconclusive. Laparotomy performed in the next day demonstrated a perforated MD at 30 cm from the terminal ileum, attached to the adjacent bowel (Figure 2B). Anatomopathological study of the surgical specimen demonstrated a layer of gastric mucosa with inflammation. 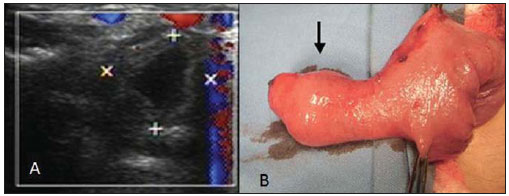 Figure 2. A: Color Doppler US demonstrates a cystic structure in the right lower abdominal quadrant with no sign of mural inflammation. B: Surgical specimen shows MD on the antimesenteric border of the ileum (arrow). DISCUSSION Meckel's diverticulum is a true diverticulum and its layers are formed by all the layers of the ileal wall(6). Ectopic gastric mucosa and pancreatic tissue may be found within the diverticula (1,6). Typically, MD is located in the terminal ileum at 40-100 cm from the ileocecal valve and, for this reason, should be considered in the differential diagnosis of right iliacal fossa conditions, such as appendicitis(3-7). It may be asymptomatic and incidentally found at laparotomy. The most common symptom is painless hematochezia(1) and complications include perforation, intussusception and volvulus. In cases where the MD is inflamed, it may be detected by US, CT or scintigraphy(2-7). Ultrasonography has become a relevant tool in the diagnosis, particularly in emergency cases, considering the symptoms, additionally to the fact that it is a method free from ionizing radiation. In both cases, the B-mode US demonstrated the MD with a typical appearance of a cystic mass with the so called gut signature: inner hyperechoic layer (submucosal), and outer hypoechoic layer (muscular)(2-4). Such an appearance may mimic intestinal duplication cysts, although the latter ones have a smoother inner layer as they are in the intestinal mucosa(2,3). Other sonographic feature of inflamed MD is the absence of peristalsis which makes it different from the adjacent bowel loops(3). A hemorrhagic MD may contract itself and complicate its detection, like in case 1, where the MD contracted itself during the examination, remaining completely emptied. Generally, in an inflamed diverticulum, color Doppler US can detect parietal hyperemia and presence of a nurturing vessel(3,4). In case 2, B-mode and color Doppler US did not show any mural inflammation sign, despite the presence of perforation and the fact the anatomopathological analysis has demonstrated inflammation. In the investigation of a MD, Tc-99m scintigraphy results may be either negative or inconclusive ince they depend on the presence of ectopic gastric mucosa - which may ulcerate and bleed -, and the bleeding rate(8), which justifies an investigation with other imaging methods such as US. In the patient of the case 1, in spite of the presence of hemorrhage, signs of inflammation or ulceration were not found in the surgical specimen analysis. In case of MD perforation, a hyperechoic outer fibrin layer can be visualized(4). Such image was not demonstrated at the B-mode US in the patient of case 2. Previous reports on the utilization of color Doppler US in the assessment of MD(4) have shown that hyperemia resulting from inflammation may be detected. The nurturing vessel of the diverticulum can also be identified(3,4). In both cases presently described, color Doppler US did not demonstrate any sign of mural inflammation, although in one of the cases, with presence of perforation and adhesions, the lesion has demonstrated inflammation at anatomopathological exam. Ultrasonography is a useful tool in the evaluation of MD, particularly in cases where scintigraphy is negative or inconclusive(3,6). Meckel's diverticula without signs of inflammation can be detected because of their typical presentation of a cystic mass with walls structured like the bowel's (gut signature) with possible peristalsis. Data available in the literature(3,4) indicate that in MD the inflammatory process is identified at color Doppler US by the increase in the vascularization of such structure. In the present cases, the absence of signs of hyperemia was observed even with a perforated and inflamed MD. The authors cannot explain such a fact. Further studies with a higher number of patients could provide more information for determining the color Doppler US accuracy in the identification of MD inflammation. REFERENCES 1. Moore TC. Omphalomesenteric duct malformations. Semin Pediatr Surg. 1996;5:116-23. 2. Daneman A, Lobo E, Alton DJ, et al. The value of sonography, CT and air enema for detection of complicated Meckel diverticulum in children with nonspecific clinical presentation. Pediatr Radiol. 1998;28:928-32. 3. Baldisserotto M, Maffazzoni DR, Dora MD. Sonographic findings of Meckel’s diverticulitis in children. AJR Am J Roentgenol. 2003;180:425-8. 4. Baldisserotto M. Color Doppler sonographic findings of inflamed and perforated Meckel diverticulum. J Ultrasound Med. 2004;23:843-8. 5. Miele V, De Cicco ML, Andreoli C, et al. US and CT findings in complicated Meckel diverticulum. Radiol Med. 2001;101:230-4. 6. Levy AD, Hobbs CM. From the archives of the AFIP. Meckel diverticulum: radiologic features with pathologic correlation. Radiographics. 2004;24:565-87. 7. Sung T, Callahan MJ, Taylor GA. Clinical and imaging mimickers of acute appendicitis in the pediatric population. AJR Am J Roentgenol. 2006;186:67-74. 8. Swaniker F, Soldes O, Hirschl RB. The utility of technetium 99m pertechnetate scintigraphy in the evaluation of patients with Meckel’s diverticulum. J Pediatr Surg. 1999;34:760-4. 1. Master in Medicine (Pediatrics and Child Health), MD, Ultrasonography, Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil. 2. Master in Medicine (Pediatrics and Child Health), Assistant Professor at Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil. 3. PhD in Medicine (Pediatrics and Child Health), Chair of the Committee of Pediatric Gastroenterology, Sociedade de Pediatria do Rio Grande do Sul, Porto Alegre, RS, Brazil. 4. Master in Medicine, Assistant Professor at Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil. 5. PhD of Medicine (Radiology), Associate Professor at Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil. Mailing Address: Dra. Mariana Damian Mizerkowski Rua José Scuissiato, 173, Seminário Curitiba, PR, Brazil, 80740-580 E-mail: maridamiz@hotmail.com Received June 5, 2010. Accepted after revision March 16, 2011. Study developed at Hospital São Lucas da Pontifícia Universidade Católica do Rio Grande do Sul (PUCRS), Porto Alegre, RS, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554