INTRODUCTION
Paranasal sinuses are a group of air-filled spaces developed as an expansion of the nasal cavities, eroding the adjacent bone structures. According to the literature, some os such regions present a high risk for injuries and consequential intraoperative complications, with the ethmoid and frontal sinuses being most frequently affected(1,2). Anatomical variations, in association with their inherent conditions, are added to such risks so the knowledge on these structures is critical for endoscopic surgeons as well as for radiologists involved in the preoperative evaluation, in order to avoid therapeutic failure and iatrogenic complications(2—5).
The acquisition of an excellent definition of the sinusal anatomy for a preoperative endoscopic evaluation can be done by means of computed tomography that is the gold standard in the study of such structures, for providing accurate information on soft tissues, bone structures and air, thus characterizing a highly sensitive imaging method(5,6).
The present pictorial essay is aimed at demonstrating the main anatomical variations that may be detected in paranasal sinuses by means of 40-row multislice computed tomography.
NASAL SEPTUM
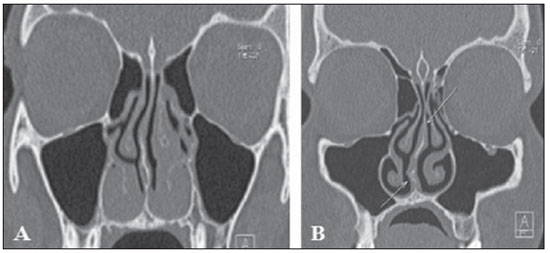
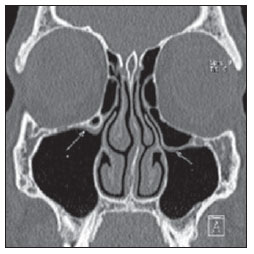
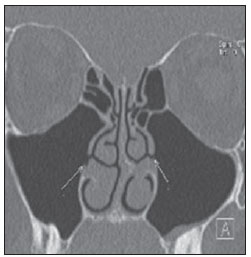
Alterations of the nasal septum (delimited by the vomer, perpendicular plate for the ethmoid bone and septal cartilage) result in morphological variations such as septal deviation, chondrovomeral junction deformity and nasal bone spur. Septal deviation is a sift of the midline associated with deformities or asymmetry of the adjacent turbinates (Figure 1A) or of the nasal wall structure, with variable presentations in the population(6,7).
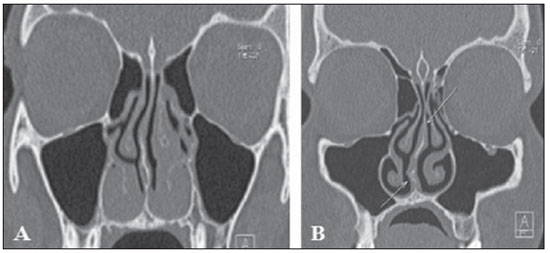
Figure 1.
Nasal septum deviation. A: Nasal septum deviation to the right. Also, note hypertrophy of the inferior turbinates and of the left middle turbinate. B: Double nasal septum deviation, with the upper portion deviated to the left, and the lower portion to the right with spur at right.
Nasal septal spur (Figure 1B) is a generally asymptomatic bone deformity that may cause restriction of the nasal air flow, and that may be associated with septal deviation. Depending on the degree of obstruction and symptoms severity, surgical correction may be required(7).
VARIATIONS OF THE MIDDLE TURBINATES
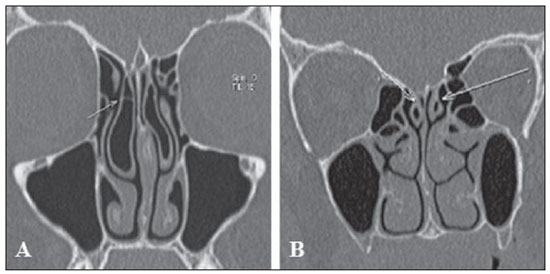
Concha bullosa (Figure 2A) is a variation originated from pneumatization of the bone plate by extension of ethmoid sinus cells. Such variation may be either uni- or bilateral (Figure 2B). Varied degrees of pneumatization of the concha may be observed, possibly causing middle meatus or infundibulum obstruction, besides being related to deviation of the nasal septum to the contralateral side(8). Other variation that is frequently associated with septal deviation and spur is unilateral hypoplasia (Figure 3A). In cases of bilateral hypoplasia, it is associated with low fovea ethmoidalis(7). Paradoxical turbinates occur as the convexity of the middle turbinate is directed towards the medial wall of the maxillary sinus. Depending on the degree of curvature of the paradoxical turbinate (Figure 3B), compression of the infundibulum and sinusal obstruction may be observed(8).
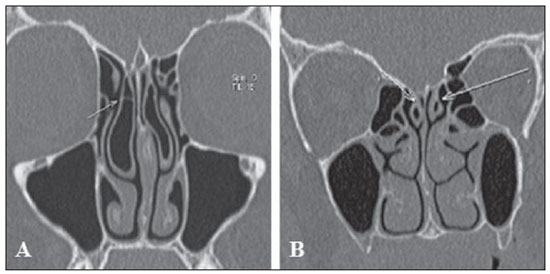
Figure 2.
Anatomical variations of the nasal conchae. A: Bilateral middle concha bullosa, with septation at right. B: Bilateral pneumatization of superior nasal concha.
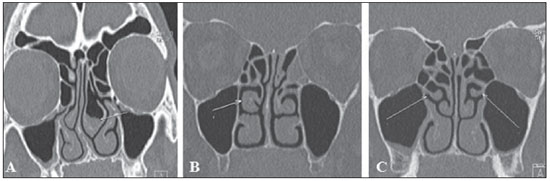
Figure 3.
Anatomical variations of the nasal conchae. A: Middle concha bullosa at left, with inflammatory process inside. Hypoplasia of right middle nasal concha in association with septal deviation. B: Paradoxical middle turbinate at right. C: Bilateral, accessory middle nasal concha.
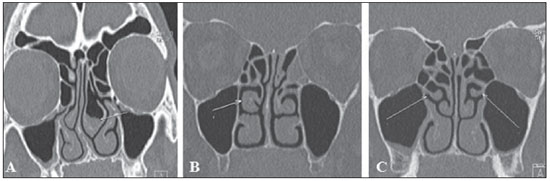
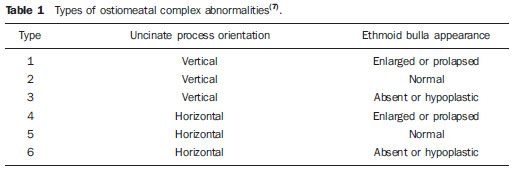
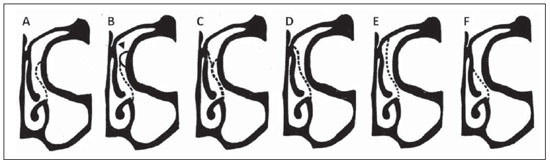
The uncinate process is a superior extension of the lateral nasal wall that is anatomically relevant for draining the frontal recess. Variations such as hypertrophy, deviation and pneumatization (Figure 4) may affect the drainage, generating abnormalities in the ostiomeatal complex (Table 1) and predisposing to obstruction(6,7,9).
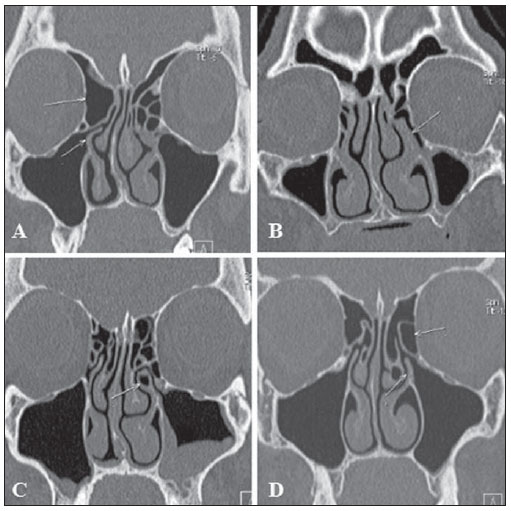
Figure 4.
Anatomical variations of the uncinate process. A: Right, horizontal uncinate process associated with voluminous ethmoid bulla (type 4). B: Hypertrophy of left uncinate process and insertion into the vertical lamella of left middle nasal concha. C: Pneumatization of left uncinate process. D: Vertical left uncinate process associated with voluminous ethmoid bulla (type 1).
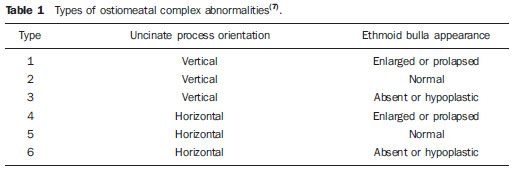
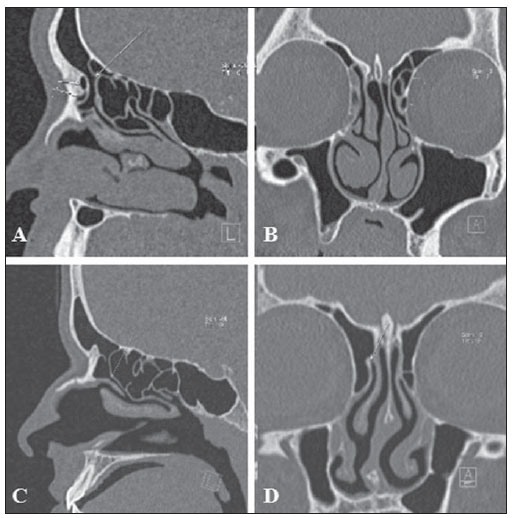
Traditionally, the uncinate process is identified from its lower segment through the architecture of the ostiomeatal unit. Variations in the superior insertion of the uncinate process are classified according to the criteria developed by Landsberg & Friedman(10) (Figure 5).
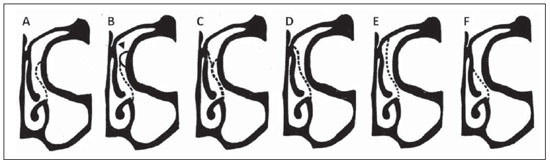
Figure 5.
Landsberg & Friedman classification of superior uncinate process insertion. A: Type 1 (insertion into the lamina papyracea). B: Type 2 (insertion into the posterior wall of agger nasi cell). C: Type 3 (insertion into the lamina papyracea and junction of the middle turbinate with the cribriform plate). D: Type 4 (insertion in to junction of the middle turbinate with the cribriform plate). E: Type 5 (insertion into the skull base). F: Type 6 (insertion into the middle turbinate).
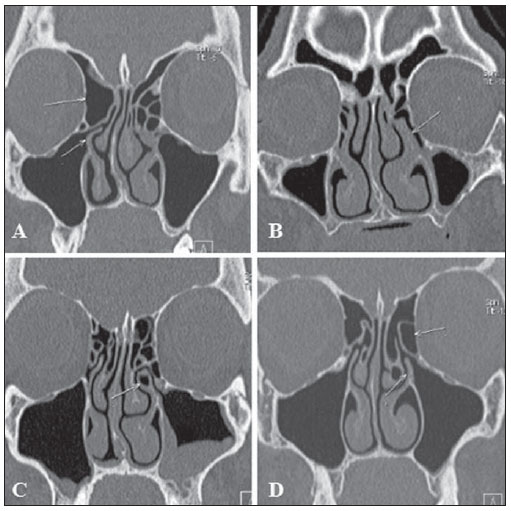
The sphenoid sinuses arise from presphenoid bone centers, with variable pneumatization extent (Figure 6A). In most of cases, pneumatization presents recesses related to the greater sphenoid wing, although lateral extensions may also be observed in the smaller sphenoid wing, inferolateral and septal recesses(7) (Figure 6B).
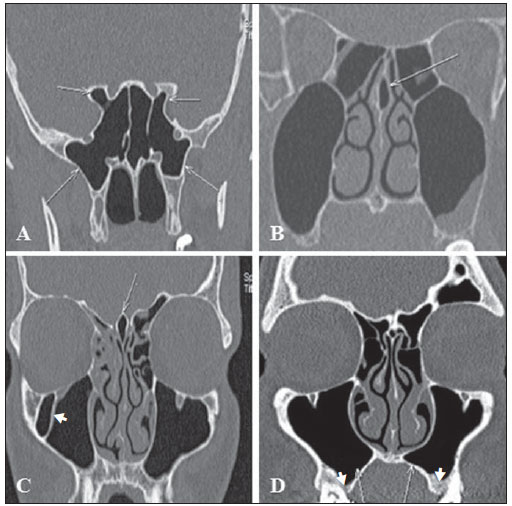
Figure 6. Extension of pneumatization of paranasal sinuses. A: Extension of pneumatization of sphenoid sinus towards the lateral recess of the sphenoid bone (bilateral) and towards the anterior clinoid processes. B: Nasal septum pneumatization characterizing septal recess. C: Pneumatization of crista galli (arrow). Note the presence of septation in the right maxillary sinus (arrowhead). D: Extension of pneumatization of the maxillary sinus towards the palatine recess (arrows) and alveolar recess (arrowheads).
Frontal sinus extension (Figure 6C) is a rare condition characterized by increased sinusal aeration beyond the normal margin of the frontal bone that originates from anterior extension of the anterior ethmoid air cells. Extensions related to the lamina of the frontal bone, crista galli, besides inferior, symmetric extension of the frontal sinus towards the anterior ethmoid air cells may also be found predominantly in male individuals in the age range between 20 and 40 years. Cases in children have not been reported(11).
As regards the maxillary sinus, four recesses have been described, as follows: the palatine recess that extends inferomedially to the hard palate towards the midline; the alveolar recess, closely related to the molar and premolar teeth roots (Figure 6D); the infraorbital recess, projecting anteriorly along the roof of the maxillary sinus; and the zygomatic recess that extends over the malar bone at variable distances(7).
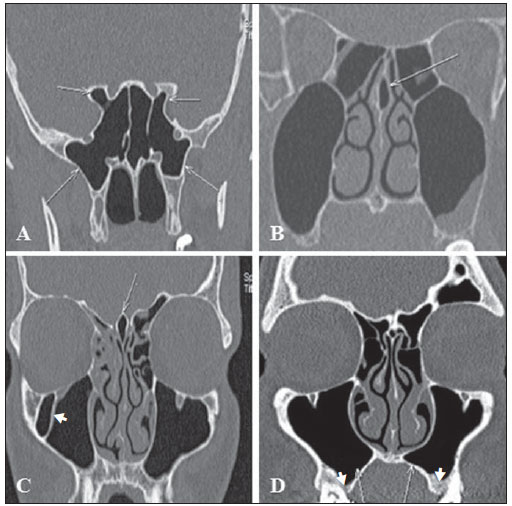
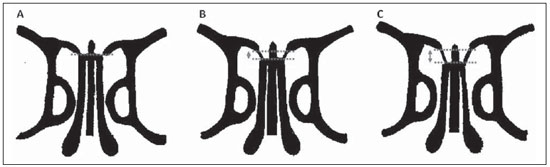
VARIATIONS OF THE CRIBRIFORM PLATE
The cribriform plate may present at variable levels and, in such cases it is classified according to the criteria developed by Keros (Figure 7), that is based on the height of the olfactory fossa in relation to the roof of the ethmoid sinus as compared with the length of the lateral lamella of cribriform plate. The higher the Keros grade, the greater the chance of injury of the cribriform plate and olfactory fossa, with consequential risk for iatrogenic cerebrospinal fluid fistula and olfactory impairment(12).
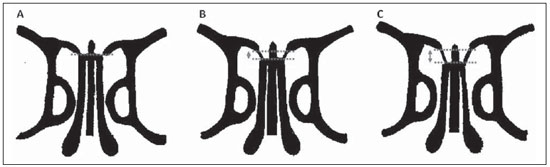
Figure 7.
Keros classification. A: Type 1 (lateral cribriform lamella of 1–3 mm, the cribriform plate and the ethmoid cell roof are practically parallel to each other). B: Type 2 (lateral lamella of 4-7 mm, cribriform plate is much below the nasal cavity as compared with the ethmoid roof). C: Type 3 (lateral lamella of cribriform plate of 8–16 mm, ethmoid cell roof is located much above the plate).
Infraorbital ethmoid cells (Figure 8), or Haller cells, are ethmoid air cells located anteriorly to the ethmoid bulla, along the orbital floor, adjacent to the natural ostium of the maxillary sinus, which may cause mucociliary drainage obstruction, predisposing to the development of sinusitis(5,7).
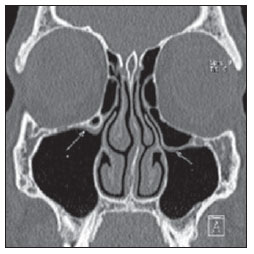
Figure 8.
Haller cell. Bilateral infraorbital ethmoid cells, larger at right.
Agger nasi cells (Figure 9), which are the most anterior ethmoid cells, are located anteriorly to the upper margin of the nasolacrimal duct and anteriorly to the plane of the maxillary sinus infundibulum. Studies demonstrate that their major dimensions are correlated with frontal sinus diseases and lacrimation(6,8,9).
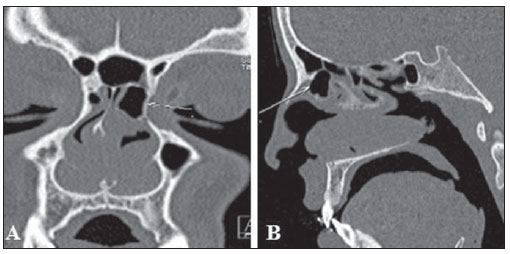
Figure 9.
Agger nasi cell. Voluminous agger nasi cell at left.
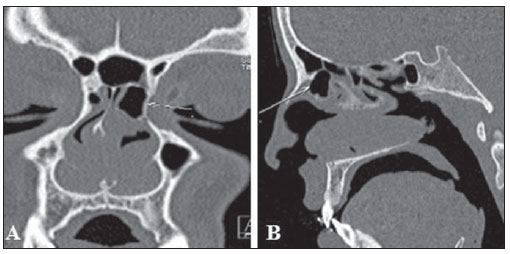
Onodi cells (Figure 10) are ethmoid cells that have migrated to the anterior region of the sphenoid sinus, with anterosuperior location, and intimately related to the optic nerve, causing optic neuropathy in case of certain conditions that affect such cells(13).

Figure 10.
Onodi cell. A,B: Bilateral Onodi cells (arrows). C: Note the sphenoid sinus ostium without connection with the Onodi cell (arrow).
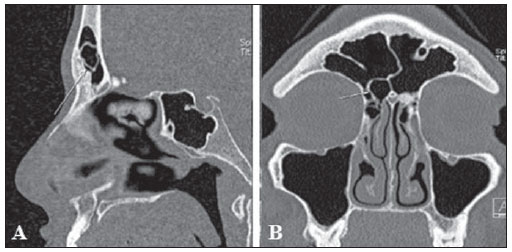
Bulla frontalis (Figure 11) are characterized by anterior ethmoid cells which invade the frontal bone, bulging its floor, but with no connection with this sinus. They are more easily demonstrated at sagittal computed tomography, where they appear as ethmoid air cells located above the ethmoid bulla and as an extension towards the frontal sinus. Depending on their size and pneumatization extent, such cells may affect the frontal sinus drainage, representing a real diagnostic challenge in addition to the difficulty of the surgical management of inflammatory diseases involving such a sinus.
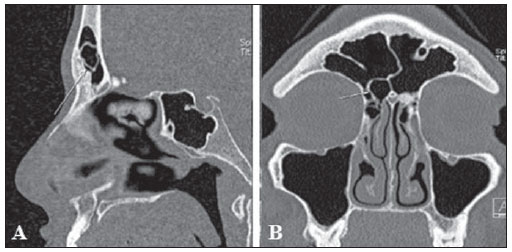
Figure 11.
Bulla frontalis. Bulla frontalis (arrow).
Other ethmoid cell variations may be found in the frontal recess (Figure 12), influencing its architecture that is determined by the patency of walls and boundaries of adjacent structures(9), such as frontal cells which are classified into four types(14), as follows:
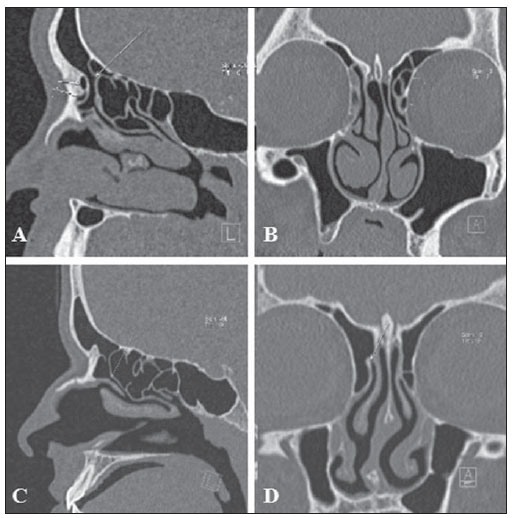
Figure 12.
Anatomical variations in the frontal recess. A,B: Type II frontal cell at left. C,D: Normal frontal recess at right, anteriorly delimitated by agger nasi cell, laterally by the lamina papyracea, and medially by the anterior and superior portions of the middle concha.
a) type 1: detected in 37% of frontal recesses; defined as a single ethmoid cell located anteriorly to the frontal recess and above the agger nasi cell;
b) type 2: detected in 19% of cases; two or more ethmoid cells located anteriorly to the frontal recess, above the agger nasi cell (Figures 12A and 12B);
c) type 3: represents 6—8% of cases; a single, voluminous cell detected above the agger nasi cell, with extension to the frontal sinus;
d) type 4: rarely found, it represents 2—4% of cases, corresponding to an ethmoid cell within the frontal sinus, with no connection with the agger nasi cell.
MAXILLARY SINUSES SEPTA
Maxillary sinus septa (Figure 6C) are thin walls of cortical bone present within the maxillary sinus, with variable number, thickness and length. Such septa may divide the sinus into two or more cavities arising from the inferior and lateral walls of the sinus. Septa originating from teeth may be classified according to their development at the different phases of the dental eruption(15,16).
ACCESSORY MAXILLARY OSTIA
Accessory maxillary ostia (Figure 13) are generally solitary, but occasionally may be multiple. Such variation may be congenital or secondary to sinusal diseases. Possible mechanisms involved in the development of such variation include: main ostium obstruction, maxillary sinusitis or anatomical/pathological factors in the middle meatus, resulting in rupture of membranous areas(17).
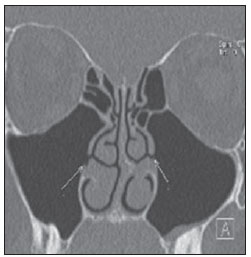
Figure 13.
Accessory ostia of maxillary sinuses. Bilateral accessory ostia of maxillary sinuses.
Computed tomography plays a fundamental role in the diagnosis of sinusal anatomical variations as well as of sinusal diseases, for a better guidance in the decision making about clinical therapeutic and surgical approaches, acting as an essential tool for a better performance of less invasive operative techniques.
REFERENCES
1. Ohnishi T, Tachibana T, Kaneko Y, et al. High-risk areas in endoscopic sinus surgery and prevention of complications. Laryngoscope. 1993;103:181-5.
2. Souza SA, Souza MMA, Idagawa M, et al. Análise por tomografia computadorizada do teto etmoidal: importante área de risco em cirurgia endoscópica nasal. Radiol Bras. 2008;41:143-7.
3. Kantarci M, Karasen RM, Alper F, et al. Remarkable anatomic variations in paranasal sinus region and their clinical importance. Eur J Radiol. 2004;50:296-302.
4. Schnipper D, Spiegel JH. Management of intracranial complications of sinus surgery. Otolaryngol Clin North Am. 2004;37:453-72.
5. Kinsui MM, Guilherme A, Yamashita HK. Variações anatômicas e sinusopatias: estudo por tomografia computadorizada. Rev Bras Otorrinolaringol. 2002;68:645-52.
6. Riello APFL, Boasquevisque EM. Variações anatômicas do complexo ostiomeatal: achados tomográficos em 200 pacientes. Radiol Bras. 2008;41:149-54.
7. Earwaker J. Anatomic variants in sinonasal CT. Radiographics. 1993;13:381-415.
8. Araújo Neto SA, Martins PSL, Souza AS, et al. O papel das variantes anatômicas do complexo ostiomeatal na rinossinusite crônica. Radiol Bras. 2006;39:227-32.
9. Huang BY, Lloyd KM, DelGaudio JM, et al. Failed endoscopic sinus surgery: spectrum of CT findings in the frontal recess. Radiographics. 2009;29:177-95.
10. Turgut S, Ercan I, Sayin I, et al. The relationship between frontal sinusitis and localization of the frontal sinus outflow tract: a computer-assisted anatomical and clinical study. Arch Otolaryngol Head Neck Surg. 2005;131:518-22.
11. Hajiioannou J, Owens D, Whittet HB. Evaluation of anatomical variation of the crista galli using computed tomography. Clin Anat. 2010;23:370-3.
12. Keros P. Über die praktische Bedeutung der Niveauunter-schiede der Lamina cribrosa des Ethmoids. Z Laryngol Rhinol Otol. 1962;41:809-13.
13. Klink T, Pahnke J, Hoppe F, et al. Acute visual loss by an Onodi cell. Br J Ophthalmol. 2000;84:801-2.
14. Lee WT, Kuhn FA, Citardi MJ. 3D computed tomographic analysis of frontal recess anatomy in patients without frontal sinusitis. Otolaryngol Head Neck Surg. 2004;131:164-73.
15. González-Santana H, Peñarrocha-Diago M, Guarinos-Carbó J, et al. A study of the septa in the maxillary sinuses and the subantral alveolar processes in 30 patients. J Oral Implantol. 2007;33:340-3.
16. Maestre-Ferrín L, Galán-Gil S, Rubio-Serrano M, et al. Maxillary sinus septa: a systematic review. Med Oral Patol Oral Cir Bucal. 2010;15:e383-6.
17. Kumar H, Choudhry R, Kakar S. Accessory maxillary ostia: topography and clinical application. J Anat Soc India. 2001;50:3-5.
1. PhD, Coordinator for the Sector of Computed Tomography at Clínica de Medicina Nuclear e Radiologia de Maceió (Medradius), Professor of Radiology and Imaging Diagnosis, Universidade Federal de Alagoas (UFAL), Maceió, AL, Brazil.
2. Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MD, Radiologist, Sector of Computed Tomography, Clínica de Medicina Nuclear e Radiologia de Maceió (Medradius), Maceió, AL, Brazil.
3. PhD, MD, Otorhinolaryngologist, Clínica Sinus, Maceió, AL, Brazil.
4. Graduate Students of Medicine, Student Monitor of the Discipline of Radiology and Imaging Diagnosis, Universidade Federal de Alagoas (UFAL), Maceió, AL, Brazil.
5. Graduate Students of Medicine, Universidade Federal de Alagoas (UFAL), Maceió, AL, Brazil.
Mailing Address:
Dra. Christiana Maia Nobre Rocha de Miranda
Rua Hugo Corrêa Paes, 104, Farol
Maceió, AL, Brazil, 57050-730
E-mail: maiachristiana@globo.com
Received February 13, 2011.
Accepted after revision June 3, 2011.
Study developed at Clínica de Medicina Nuclear e Radiologia de Maceió (Medradius), Maceió, AL, Brazil.
 Vol. 44 nº 4 - July / Aug. of 2011
Vol. 44 nº 4 - July / Aug. of 2011