Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 4 - July / Aug. of 2011
Vol. 44 nº 4 - July / Aug. of 2011
|
WHICH IS YOUR DIAGNOSIS?
|
|
WHICH IS YOUR DIAGNOSIS? |
|
|
Autho(rs): Pedro José de Santana Júnior1; Jorgeana Milhomem Bandeira2; Ana Caroline Vieira Aurione3; Renato Duarte Carneiro4; Rubens Carneiro dos Santos Júnior5; Kim-Ir-Sen Santos Teixeira6 |
|
|
A female, 67-year-old patients presented at the Hospital das Clínicas ambulatory - Universidade Federal de Goiás (HC-UFG) complaining of pain and paresthesia in the right lower limb, with progressive intensity over the last five months. The patient remained limited to the bed, in decubitus position with the affected limb in semi-flexed position. She denied the occurrence of trauma. At clinical examination, a palpable mass of about 15 cm in diameter, with undefined margins was found in the right flank. The patient reported previous history of uterine cervix carcinoma diagnosed in 2007. Abdominal radiography and computed tomography (CT) were performed at the Department of Radiology of HC-UFG.
Images description Figure 1. Abdominal radiography demonstrates fading of the psoas muscle outline associated with opacity in the right hemiabdomen. Note the expansile effect characterized by displacement of bowel loops to the left and undefined ascending colon.  Figure 1. Abdominal radiography. Figure 2. Abdominal computed tomography. Contrast-enhanced axial (A,B) and coronal (C,D) sections demonstrate an expansile, multiseptated, heterogeneous cystic lesion with peripheral iodinated contrast uptake, located in the right iliopsoas compartment. Also, densification of adjacent fat planes (on A,B,C,D) and displacement of the ipsilateral kidney (on C,D) are observed. 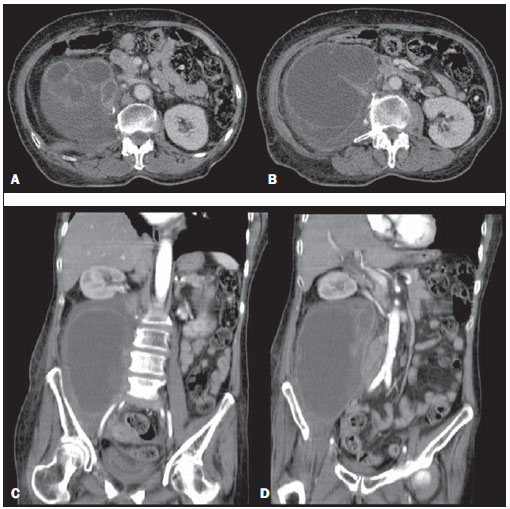 Figure 2. Abdominal computed tomography, contrast-enhanced axial sections (A,B) and coronal sections (C,D). Diagnosis: Metastasis from squamous cell carcinoma of uterine cervix to the right iliopsoas compartment. COMMENTS The iliopsoas compartment may be involved by different pathological processes including infection, tumor and hemorrhage. The patients may present several nonspecific signs and symptoms, causing delay in the diagnosis. The imaging assessment of such compartment, particularly by means of CT has been a relevant landmark in the diagnosis of such lesions. However, it is important to note that radiological findings may be common to several etiologies, which most of times. The involvement of the iliopsoas compartment is usually secondary to a direct extension of adjacent tumors of retroperitoneal, abdominal, pelvic, neuronal, osseous and lymphonodal origin(1,2). Primary tumors of the iliopsoas muscle (liposarcoma, fibrosarcoma, leiomyosarcoma and hemangiopericytoma) are rarely found. The retroperitoneal fascial planes do not offer a barrier to tumor dissemination, with direct and random invasion in contrast to the inflammatory/infectious involvement(3). At CT and magnetic resonance imaging, lesions with either homogeneous or heterogeneous appearance are observed as a function of the presence of necrosis, hemorrhage and alterations in the cellular structure(3). Presence of hypoattenuating area, irregular margins, adenopathy, bone destruction and discontinuity of fascial planes represent the most significant findings in the distinction among tumors, abscesses and hematomas(2). In the series described by Muttarak & Peh(1), among the 14 reported cases of tumor, there was secondary involvement in ten, with metastasis from uterine cervix carcinoma being the most common origin, similarly to the present report. The infectious involvement of the iliopsoas compartment may be primary or secondary. Primary abscesses are rare and generally idiopathic. Staphylococcus aureus and gram-negative microorganisms are the organisms most frequently involved. Immunocompromised patients, especially those undergoing corticotherapy, chemotherapy, as well as HIV-positive patients are particularly predisposed to infection(1,3). The secondary involvement of the iliopsoas compartment is much more frequent, generally resulting from dissemination of infectious processes originated in kidneys (perinephric abscesses), bones (osteomyelitis and tuberculosis), and in intestinal loops (appendicitis, diverticulitis, Crohn’s disease and perforated colon carcinoma(1). The most common tomographic findings are enlargement of the iliopsoas muscle with hypoattenuating Center, as well as parietal contrast enhancement. Such signs are nonspecific and non-distinguishable from metastases and lymphoma. Secondary findings that may corroborate such diagnosis include densification in adjacent fat planes, bone destruction and intermingled gas bubbles. Iliopsoas compartment hematomas may be either spontaneous or secondary to hemorrhagic diathesis, anticoagulant therapy, trauma, tumor, recent surgery or biopsy, or even resulting from extension of bleeding in adjacent organs and vessels(1,2). As causal factor and patient’s age were correlated, most noticeable association with coagulopathy and trauma was observed in the youngest age range (fourth decade of life), and with aortic aneurysm rupture, anticoagulant therapy for arteriosclerotic disease and thromboembolism in the most advanced age range (seventh decade of life)(3). Acute hemorrhage is seen as a spontaneously hypoattenuating lesion. Fluid-fluid level may be present because of hematocrit effect. It is important to highlight that chronic hematomas are hardly differentiated from abscesses and tumors. Percutaneous aspiration is useful in such differentiation. Based on the present case, it is possible to observe the critical role of CT in the determination of the involvement of the iliopsoas compartment by the lesion. At one end, one observes the difficulty in determining which radiological findings are suggestive of disease in such location. In a high number of cases, such findings are insufficient to determine the disease etiology. On the other hand, the diagnostic accuracy significantly increases as radiological findings are associated with clinical data. In the present case, the patient was submitted to laparotomy with biopsy of the retroperitoneal mass radiologically identified, with a result compatible with a poorly differentiated infiltrating squamous cell carcinoma and extensive areas of necrosis. Hence the significance of the present report, where the previous history of invasive squamous cell carcinoma of uterine cervix, in association with imaging findings may favor the diagnosis of metastatic lesion in the iliopsoas muscle. REFERENCES 1. Muttarak M, Peh WCG. CT of unusual iliopsoas compartment lesions. Radiographics. 2000;20:S53-66. 2. Leão ARS, Amaral RPG, Abud TG, et al. Patologias do compartimento iliopsoas: avaliação radiológica. Radiol Bras. 2007;40:267-72. 3. Lenchik L, Dovgan DJ, Kier R. CT of the iliopsoas compartment: value in differentiating tumor, abscess, and hematoma. AJR Am J Roentgenol. 1994;162:83-6. 1. MD, Radiologist, Trainee at the Unit of Magnetic Resonance Imaging of Santa Casa de Misericórdia de São Paulo, São Paulo, SP, Brazil. 2. MD, Radiologist, Trainee at Unit of Magnetic Resonance Imaging of CRER – Centro de Reabilitação e Readaptação Henrique Santillo, Goiânia, GO, Brazil. 3. Graduate Student of Medicine, Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil. 4. Titular Member of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MD, Radiologist at Multimagem Diagnósticos, Goiânia, GO, Brazil. 5. Master in Radiology, Professor, Department of Radiology, Hospital das Clínicas da Universidade Federal de Goiás (UFG), Head for the Unit of Magnetic Resonance Imaging at Instituto de Neurologia de Goiânia, Goiânia, GO, Brazil. 6. PhD of Radiology, Associate Professor, Department of Radiology at Hospital das Clínicas da Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil. Mailing Address: Dr. Pedro José de Santana Júnior Rua T-36, nº 3485, ap. 104, Edifício Solar dos Tocantins, Setor Bueno Goiânia, GO, Brazil, 74223-050 E-mail: psantanajr@hotmail.com Study developed at Hospital das Clínicas da Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554