Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 3 - May / June of 2011
Vol. 44 nº 3 - May / June of 2011
|
ORIGINAL ARTICLE
|
|
Comparison between transvaginal ultrasonography and sonohysterography in the assessment of patients with abnormal uterine bleeding |
|
|
Autho(rs): Iêda Maria Silveira Diógenes Feitosa1; Helvécio Neves Feitosa2; Francisco Herlânio Costa Carvalho3; Silvia Menescal Pereira1; Francisco das Chagas Medeiros4 |
|
|
Keywords: Transvaginal ultrasonography; Sonohysterography; Hysteroscopy; Abnormal uterine bleeding. |
|
|
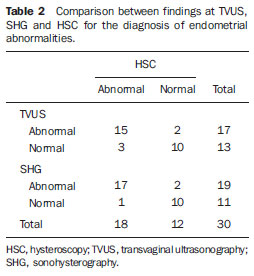
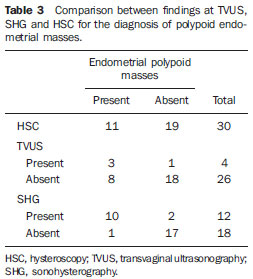
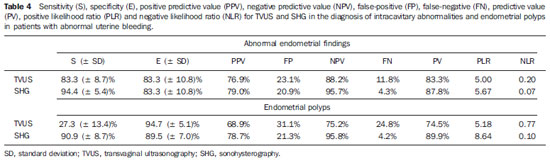
Abstract: INTRODUCTION
Pelvic ultrasonography, and in particular transvaginal ultrasonography (TVUS), is a propedeutic method extensively utilized in gynecology and obstetrics. In pregnancy, it is widely utilized to analyze embryonic and fetal anatomy at the first trimester(1) and to evaluate the biometry and morphology of the uterine cervix in more advanced gestations(2), demonstrating to be an excellent predictor of preterm delivery(3). It leaves no doubts about the benefit of evaluating adnexal masses(4), including deep endometriosis and its intestinal involvement — with effectiveness comparable to magnetic resonance imaging(5). It is the most frequently utilized propedeutic imaging method as a first line of investigation in patients with abnormal uterine bleeding(6). Abnormal uterine bleeding is one of the main complaints at gynecological clinics at any age group, possibly as a consequence of anovulation, disorders related to pregnancy, hormonal changes or lesions of benign or malignant nature. The etiology of such abnormality may range from local anatomic causes to endocrine disorders, or even other organic diseases or iatrogenic factors. The main focus in the diagnostic investigation of such patients is ruling out the possibility of endometrial carcinoma and correctly identify local anatomic causes, such as polyps and uterine myomas, which may require surgical treatment, or functional disorders that require clinical treatment(6). Sonohysterography (SHG) — instillation of sterile saline solution by means of a catheter — was initially described by Nannini et al. in 1981(7). Other authors also utilized fluids as expanders of the uterine cavity, in order to allow echographic contrast with adjacent structures, thus allowing better evaluation of the endometrium(8—11). The use of SHG yields better images as compared with TVUS, providing a more accurate measurement of the endometrial thickness, which allows a more clear evaluation of the heterogeneity or of the thickening etiology, besides allowing the distinction between focal and diffuse abnormalities(12). The present study was aimed at determining the value of SHG and TVUS in the detection of endometrial changes in patients with abnormal uterine bleeding, and comparing the sensitivity and specificity of the methods in the detection of such disorders. MATERIALS AND METHODS This is a comparative, cross-sectional and observational study on diagnostic imaging methods, developed at the Unit of Ultrasonography of Maternidade-Escola Assis Chateaubriand — Universidade Federal do Ceará (UFC), Fortaleza, CE, Brazil. The sample comprised 30 patients with ages ranging from 29 to 71 years, presenting abnormal uterine bleeding (menorrhagia, metrorrhagia or postmenopausal bleeding without using hormonal therapy). Twenty-one (70%) of the patients were premenopausal women, and nine (30%) were postmenopausal women. All the pregnant patients as well as those using contraceptives were excluded. The project was approved by the UFC Committee for Ethics in Research, and the study was developed in the period between July and December of 2003. After signing a term of free and informed consent, all the patients were submitted to anamnesis and underwent gynecological examination as initial steps of propedeutics, as well as to diagnose and treat genital infectious processes. Subsequently, pelvic ultrasonography, TVUS, SHG and hysteroscopy (HSC) were performed, in this order. The following criteria were adopted to express the sonographic results: normal cavity, endometrial thickening (> 14 mm for premenopausal women and > 5 mm for postmenopausal women) and endometrial atrophy (endometrial thickness < 4 mm)(13). Hyperechogenic nodular lesions in the endometrial cavity were considered as polyps, while lesions with mixed echogenicity or hypoechoic lesions altering the contours of the endometrial cavity were considered as submucosal myomas. Findings were considered as suspected for malignancy in cases where the endometrial echo was irregular or with a variable echotexture(10). All the patients underwent SHG following TVUS, even when the TVUS results were normal. A Sonoline Versa Pro model US apparatus (Siemens; Erlangen, Germany) was utilized with a 6.5 MHz transvaginal probe and a 3.5 MHz convex probe for pelvic examination, both of them multifrequency. All the TVUSs and SHGs were performed by a single investigator, with a title of Specialist in Gynecology and Obstetrics, qualified in Ultrasonography in Gynecology and Obstetrics by Federação Brasileira de Ginecologia e Obstetrícia (Brazilian Federation of Gynecology and Obstetrics). During the SHG, with the patient in gynecological positioning, a speculum examination was also performed in order to visualize the uterine cervix and rule out the presence of purulent mucus. After that, the vaginal antisepsis was made with iodinated povidone topical solution. Catheterization of the cervical canal was made with an Nelaton® urethral catheter Nbr.8, already filled with liquid (sterile saline solution at 0.9%) coupled to a 20 ml syringe, to reduce the production of artifacts such as the presence of air in the uterine cavity. The catheter was fixed with a Cherron clamp inserted until the bottom of the uterine cavity is achieved. Whenever necessary a Pozzi forceps was utilized for better immobilization of the uterine cervix and to facilitate the catheter insertion. Subsequently, the speculum was carefully removed and the vaginal transducer was inserted, to analyze the images concomitantly with the solution infusion. The endometrial thickness was separately measured in its anterior and posterior layers, in the sagittal plane, excluding the adjacent hypoechoic zones. The results of the SHG examination were expressed according to the criteria preconized by Bernard et al.(13): normal cavity, endometrial thickening (single layer endometrial thickening > 6 mm for premenopausal women and > 3 mm for postmenopausal women), endometrial atrophy (endometrial thickness < 2 mm). Polyps were diagnosed when a well delimited hypoechogenic focal thickening was found. All the patients underwent HSC, which was considered as the standard method. The hysteroscopic finding was defined as normal (normal or atrophic endometrium) or abnormal (presence of focal or diffuse thickening, polyps, myomas or synechiae). All the HSCs were performed by a single investigator, who did not have access to the results obtained at ultrasonography or sonohysterography. During the performance of HSC, endometrial biopsies were also performed in all the patients; but the histopathological results were conclusive in only 24 of the cases, with the collected material being considered as insufficient for analysis in six cases. The histopathological studies were performed at the Department of Pathology and Legal Medicine of the School of Medicine of UFC. The results were considered as normal in cases where the endometrium was proliferative, secretory, atrophic, or presented irregular maturation; or abnormal, in the presence of polyps, simple or complex hyperplasia, with or without atypia, myoma or endometrial carcinoma. The calculation of the sample size was made by utilizing, within the considered period, the total number of available observation units (women) equal to 200, at a significance level of 5%, and considering an estimation error margin of 16%, n corresponding to 30. The statistical analysis was performed with the aid of the software SPSS 10.0 (SPSS Co.; Chicago, IL, USA) and comprised descriptive analysis, calculation of sensitivity estimates, specificity and respective standard deviations, positive predictive values (PPV), negative predictive values (NPV), false-positive (FP) and false-negative rates (FN), predictive values (accuracy), positive likelihood ratio (PLR) and negative likelihood ratio (NLR) for endometrial changes. The McNemar’s test was utilized for comparison of sensitivities and specificities of diagnostic methods. The adopted significance level was 0.05 (5%). RESULTS Initially, the present study included 40 patients with abnormal uterine bleeding. However, ten women were excluded, for the following reasons: four presented cervical stenosis that impaired the SHG performance, five, for not having undergone HSC (standard method) and one for refusal in participating in the study. Complications were not observed; only two patients reported a mild discomfort. At HSC, 12 patients (40%) presented normal endometrial cavity, and 18 patients were diagnosed with intracavitary abnormalities (60%). Polyps were the most frequent lesions, and were found in 10 patients (33.3%), followed by diffuse endometrial thickening in three patients (10%), focal endometrial thickening in one (3.3%), submucosal myoma in two (6.7%), diffuse endometrial thickening with synechia in one (3.3%) and submucosal myoma with polyp in another case (3.3%) (Figures 1 to 4; Table 1). Histopathological study found simple endometrial hyperplasia without atypias in one patient and endometrial clear cell carcinoma in another. In the first case, both TVUS and SHG were normal while HSC revealed endometrial polyp. In the second case, TVUS and SHG revealed endometrial thickening, and HSC revealed endometrial thickening with atypical vascularization.  Figure 1. TVUS demonstrating endometrial thickening with variable echotexture. 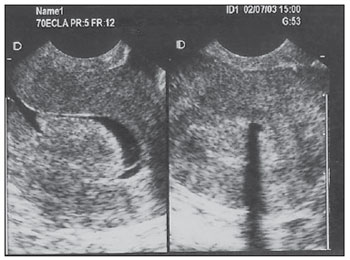 Figure 2. SHG clearly demonstrating the presence of hyperechogenic image at left (polyp). At right, acoustic shadowing is observed, produced by the presence of gas in the cavity (artifact). Same patient as on Figure 1. 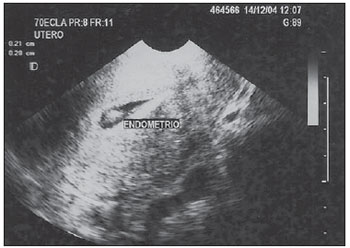 Figure 3. SHG demonstrating single hyperechogenic image suggestive of endometrial polyp – sagittal plane. 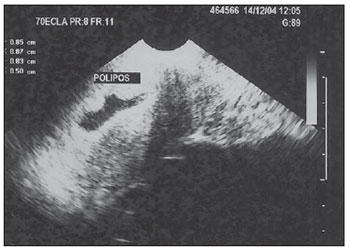 Figure 4. SHG demonstrating multifocal hyperechogenic images suggestive of endometrial polyps. Same patient as on Figure 3, after changing the transducer position – parasagittal plane. 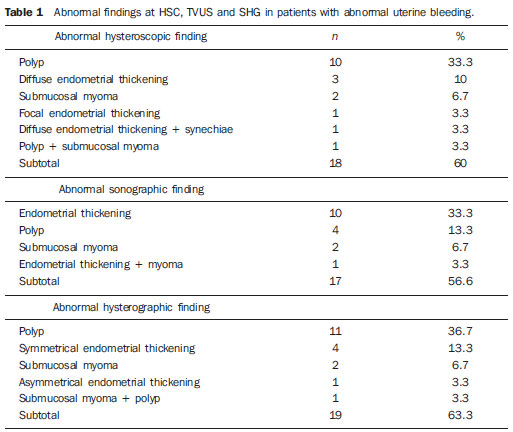 Analysis of the TVUS and SHG results was performed for the diagnosis of all the abnormalities (Table 2) and specifically for the finding of endometrial polyp (Table 3). Hysteroscopy (HSC) was utilized as the standard method, and the properties of each method were evaluated. The estimated prevalence of endometrial abnormalities (40%) and polyps (30%) were considered (Table 4). SHG allowed the detection of 17 of the 18 women with intracavitary abnormalities (sensitivity of 94.4%) and was in agreement with HSC in 10 of the normal exams (specificity of 83.3%). There were two false-positive results and one false-negative result. For the specific polyp diagnosis, the method was consistent in the detection of 10 among the 11 cases (sensitivity of 90.9%) and was compatible with absence of polyps in 17 of the 19 cases without such finding (specificity of 89.5%). In two opportunities, the method provided a false-positive result, with one case being false-negative. Transvaginal ultrasonography allowed the detection of intracavitary abnormalities in 15 of the 18 women (sensitivity of 83.3%), the results of the method being compatible with normality in 10 cases in which no endometrial abnormality was observed (specificity of 83.3%). The diagnosis was false-positive in two opportunities and false-negative in three others. For the specific diagnosis of polyp, the method allowed the detection of three among the 11 cases (sensitivity of 27.3%) and was compatible with absence of polyps in 18 of the 19 cases without such a finding (specificity of 94.7%). The method result was false-positive in one case and false-negative in eight cases. The McNemar’s test revealed statistical similarity regarding sensitivity (83.3% × 94.4%; p = 0.500) and specificity (83.3% × 83.3%; p = 1.000) for the methods (TVUS and SHG) in the diagnosis of intracavitary lesions. Specifically for the diagnosis of polyps, the specificity was statistically similar (94.7% × 89.5%; p = 1.000) and the sensitivity was greater for SHG (90.9% × 27.3%; p = 0.016) as compared with TVUS (Table 5). 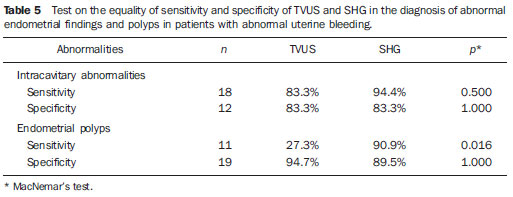 DISCUSSION Sonohysterography improves the detection of endometrial disorders, such as polyps, myomas, hyperplasia, cancer and synechiae. Additionally, it helps avoiding invasive diagnostic procedures and improving the preoperative evaluation of women requiring therapeutic intervention. It is easily and quickly performed, at a reasonable cost and is well tolerated by patients, besides being free from relevant complications(10). In the present study aimed at comparing SHG and TVUS in the diagnosis of endometrial abnormalities, in most of cases HSC was utilized as the standard method, rather than the anatomopathological study of the complete surgical specimen, as the indication for hysterectomy was restricted to a few cases. Thus, considering that its high sensitivity and specificity in the detection of intracavitary abnormalities has already been demonstrated(14), HSC was utilized for this purpose. The authors decided to include patients with abnormal uterine bleeding, independently from sonographic findings, so that subtle endometrial abnormalities underdiagnosed at TVUS were not excluded, which might limit the results interpretation, and to allow the comparison between the different methods. Another Brazilian study has included only patients with abnormalities found at TVUS(15). A single investigator performed TVUS and SHG, so interobserver variability was eliminated. One single investigator performed all the HSCs with guided-biopsy, blind to the previous studies results to avoid possible influence on the diagnoses. Hysteroscopy allowed the diagnosis of 18 intracavitary abnormalities (60% of the patients with abnormal uterine bleeding). Polyps were the most prevalent lesions (33.3%). Similar data have been described by other authors. Clevenger-Hoeft et al.(16) have found 32.5% (26 cases) in patients with abnormal uterine bleeding, and 10% (10 cases) in asymptomatic patients. Schwärzler et al.(17), in preoperative evaluation of the uterine cavity in 98 patients with abnormal uterine bleeding, in spite of clinical treatment, have found endometrial abnormalities in 52 of them (53%). Dueholm et al.(18) have observed 35% of polyps or myomas in a series of 470 premenopausal patients with abnormal uterine bleeding. In the present study there was only one case of endometrial hyperplasia, which presented “normal” results at TVUS and SHG. Similar finding was observed by Ceccato Jr. et al.(19). Endometrial (clear cell) carcinoma was correctly identified by the “endometrial thickening” observed at TVUS, and “asymmetrical endometrial thickening” at SHG. Sonohysterography was quite effective in the diagnosis of uterine abnormalities. Sensitivity of 94.4% and specificity of 83.3% were observed, similarly to the results reported by other studies(13,17,20). In the same comparison between these methods, other authors have demonstrated a greater sensitivity for SHG in the diagnosis of intracavitary abnormalities(12,17). Additionally, a high NPV was demonstrated, implying a low number of undiagnosed lesions. Schwärzler et al.(17), in a study with 104 patients, have showed that SHG increased the polyps’ detection rate from 56% to 84%, however they have observed that the detection of preneoplastic and neoplastic lesions in the endometrium was not improved by SHG. Perhaps, this may be due to the fact that SHG has greater accuracy in the identification of focal lesions than in the diagnosis of diffuse lesions particularly more associated to malignant lesions. In the present casuistry, a very small number of such lesions were observed, so a specific analysis was not feasible. As regards the evaluation of polyps, SHG presented greater sensitivity (90.9% × 27.3%; p < 0.016) and the same specificity (89.5% × 94.7%; p = 1.000) as compared with TVUS. Sonohysterography allowed a reduction of the number of false-negative results for polyps from eight to one, increasing the number of false-positive results from one to two. Schwärzler et al.(17) have observed that SHG decreased the incidence of false-negative results from 11 to four without increasing the number of false-positive results. Jacques et al.(21) have reported accuracy of 91.3% and Kamel et al.(22) 93.3% in the diagnosis of polyps with SHG in patients with abnormal uterine bleeding. Gunes et al.(23), evaluating 83 patients with suspected endometrial cavity abnormalities, have found 16 polyps. In their study, SHG presented sensitivity of 80%, specificity of 87%, PPV of 25%, NPV of 93%, PLR of 6.1 and NLR of 0.23. In the present study casuistry, such values were respectively 90.9%, 89.5%, 78.7%, 95.8%, 8.64 and 0.10. In other words, the values observed in the present study for SHG and those reported by Gunes et al.(23) are approximately the same, except for the higher sensitivity and the much higher PPV in the present study’s population. Albuquerque et al.(24) have reported a greater capacity of SHG to identify polyps as compared with TVUS. The present study aimed at the evaluation of pre- and postmenopausal patients, based on the understanding that such a group is one of the most frequently found at gynecological clinics. Several casuistries have evaluated such patients separately. Karageyim Karsidag et al.(25), evaluating 36 postmenopausal women with recurrent uterine bleeding following dilation and curettage, have analyzed the capacity of several methods to diagnose focal intracavitary lesions. Curettage has not allowed the diagnosis of 70% of the focal lesions. In the comparison between SHG and TVUS, the authors have observed greater sensitivity (93% × 63%) and lower specificity (56% × 78%) for SHG and therefore concluded that, in experienced hands, SHG can be an initial method for the evaluation of the uterine cavity in these patients. In a prospective study, Erdem et al.(26) have analyzed 122 women with abnormal pre-and postmenopausal uterine bleeding. Sonohysterography demonstrated sensitivity of 97.7% and specificity of 82.4%, while TVUS demonstrated sensitivity of 83% and specificity of 70.6%. In their study, the histological findings were: 34 normal endometrial cavities, 61 polyps, 19 submucosal myomas, four myomas not related with the cavity and four endometrial hyperplasias. Approximately one third (38/122; 31.1%) of the performed HSCs did not present endometrial cavity abnormalities and could have been considered as “unnecessary”. The authors have concluded that SHG is better than TVUS alone in the evaluation of the endometrial cavity. Moschos et al.(27) have prospectively evaluated 88 peri-and postmenopausal women (age > 40 years) with abnormal uterine bleeding and TVUS, identifying an “abnormal endometrium”. The authors have concluded that SHG was superior to biopsy (Pipelle’s probe) in the diagnosis of endometrial diseases (89% × 52%; p < 0.001), describing a level of evidence II. Albuquerque et al.(24) have compared TVUS, SHG and HSC in patients with abnormal uterine bleeding (53 pre-and post-menopausal patients) considering the histopathological finding as the standard method. They have found, respectively, sensitivity of 83%, 94% and 94% (statistically similar) and specificity of 69%, 77% and 91%. A statistically significant difference was observed between TVUS and HSC specificities of (p = 0.008). Elsayes et al.(10), in a review article, have considered SHG typically indicated in cases of abnormal uterine bleeding, both for premenopausal patients to distinguish anovulatory bleeding from anatomical lesions, and postmenopausal patients, to differentiate endometrial atrophy from intracavitary abnormalities that may require biopsy and/or surgical resection. The main objective of the method is not the histopathological result, but rather differentiating normal from abnormal cases, and when abnormal, whether the disease is focal (< 25% of the involved cavity) or diffuse, which allows the next step in the patient’s follow-up: either HSC or dilation and curettage. Such data are also consistent with those reported on an editorial published in 2007 that suggested a role for SHG in the evaluation of patients with abnormal (pre-or postmenopausal) uterine bleeding after normal TVUS(6). The excellent diagnostic accuracy of SHG, in association with the cost of some unnecessary HSCs, may motivate the use of combined TVUS and SHG in the evaluation of patients with abnormal uterine bleeding in the pre- and post-menopause to evaluate benign disorders — the main cause for abnormal uterine bleeding both in the premenopausal period (polyps, myomas) as well as in the postmenopausal period (atrophy) -, as there is no limit for the endometrial thickness, below which benign disorders can be ruled out, avoiding further investigation of the uterine cavity(6,28). Skaznik-Wikiel et al.(28) have found approximately 25% of benign disorders with endometrial thickness < 5 mm. For other authors, the greatest applicability of SHG would be to evaluate the risk for endometrial cancer which, when early diagnosed, presents a practically 100% chance of being cured. The incidence of endometrial cancer in postmenopausal women with abnormal uterine bleeding is of approximately 10%, and the abnormal uterine bleeding is the main form of clinical presentation of such a disease(29). However, SHG will not replace the role of TVUS as the initial tool in the evaluation of postmenopausal abnormal uterine bleeding, considering the extremely high sensitivity of TVUS (greater than the other diagnostic methods such as SHG, HSC and even nonfocal biopsy), besides the wide availability, tolerability, reasonable cost, possibility of diagnosing other non-cavitary problems, etc.(28,29). Sonohysterography has been playing its role in the evaluation of benign and malignant diseases in pre- and postmenopausal patients with abnormal uterine bleeding as well as asymptomatic patients with endometrial abnormalities at TVUS. Considering the excellent correlation between SHG and the hysteroscopic evaluation, it becomes an alternative whenever HSC is not available, particularly in developing countries, as it is easily and quickly performed, besides being inexpensive and well tolerated(6,23,29). However, some questions still remain unanswered: is SHG capable of decreasing the incidence of negative HSCs? In which population would it be best applied? Is its clinical benefit only for focal abnormalities? Some studies on cost effectiveness are also necessary before its total inclusion in protocols for evaluating patients with abnormal uterine bleeding and extrapolation to larger populations. CONCLUSIONS Sonohysterography and Transvaginal ultrasonography present good predictive value for endometrial disorders in patients with abnormal uterine bleeding. Sonohysterography presents sensitivity and specificity similar to those of TVUS in the detection of such abnormalities; however it presents greater sensitivity in the detection of polyps. REFERENCES 1. Rios LTM, Oliveira RVB, Martins MG, et al. Anormalidades do primeiro trimestre da gravidez: ensaio iconográfico. Radiol Bras. 2010;43:125—32. 2. Itaborahy RMR, Carmo AV, Medeiros SF, et al. Avaliação do comprimento do colo uterino em gestantes normais entre 20 e 34 semanas de gestação por meio da ultrassonografia endovaginal. Radiol Bras. 2010;43:379—83. 3. Novaes CEF, Koch HA, Montenegro CAB, et al. Diagnóstico do parto pré-termo pela medida ultrassonográfica do comprimento do colo uterino. Radiol Bras. 2009;42:295—8. 4. Andrade Neto F, Palma-Dias R, Costa FS. Ultrassonografia nas massas anexiais: aspectos de imagem. Radiol Bras. 2011;44:59—67. 5. Cardoso MM, Werner Jr H, Berardo PT, et al. Avaliação da concordância entre a ultrassonografia transvaginal e a ressonância magnética da pelve na endometriose profunda, com ênfase para o comprometimento intestinal. Radiol Bras. 2009;42:89—95. 6. Lee SI. An imaging algorithm for evaluation of abnormal uterine bleeding: does sonohysterography play a role? Menopause. 2007;14:823—5. 7. Nannini R, Chelo E, Branconi F, et al. Dynamic echohysteroscopy: a new diagnostic technique in the study of female infertility. Acta Eur Fertil. 1981;12:165—71. 8. Syrop CH, Sahakian V. Transvaginal sonographic detection of endometrial polyps with fluid contrast augmentation. Obstet Gynecol. 1992;79:1041—3. 9. Parsons AK, Lense JJ. Sonohysterography for endometrial abnormalities: preliminary results. J Clin Ultrasound. 1993;21:87—95. 10. Elsayes KM, Pandya A, Platt JF, et al. Technique and diagnostic utility of saline infusion sonohysterography. Int J Gynaecol Obstet. 2009;105:5—9. 11. Berridge DL, Winter TC. Saline infusion sonohysterography: technique, indications, and imaging findings. J Ultrasound Med. 2004;23:97—112. 12. Krampl E, Bourne T, Hurlen-Solbakken H, et al. Transvaginal ultrasonography sonohysterography and operative hysteroscopy for the evaluation of abnormal bleeding. Acta Obstet Gynecol Scand. 2001;80:616—22. 13. Bernard JP, Lécuru F, Darles C, et al. Saline contrast sonohysterography as first-line investigation for women with uterine bleeding. Ultrasound Obstet Gynecol. 1997;10:121—5. 14. Emanuel MH, Verdel MJ, Wamsteker K, et al. A prospective comparison of transvaginal ultrasonography and diagnostic hysteroscopy in the evaluation of patients with abnormal uterine bleeding: clinical implications. Am J Obstet Gynecol. 1995;172(2Pt1):547—52. 15. Diniz ALD, Gonçalves EG. Papel da histerossonografia no estudo da cavidade uterina em pacientes com sangramento uterino anormal. Rev Bras Ginecol Obstet. 2000;22:293—9. 16. Clevenger-Hoeft M, Syrop CH, Stovall DW, et al. Sonohysterography in premenopausal women with and without abnormal bleeding. Obstet Gynecol. 1999;94:516—20. 17. Schwärzler P, Concin H, Bösch H, et al. An evaluation of sonohysterography and diagnostic hysteroscopy for the assessment of intrauterine pathology. Ultrasound Obstet Gynecol. 1998;11:337—42. 18. Dueholm M, Forman A, Jensen ML, et al. Transvaginal sonography combined with saline contrast sonohysterography in evaluating the uterine cavity in premenopausal patients with abnormal uterine bleeding. Ultrasound Obstet Gynecol. 2001;18:54—61. 19. Ceccato Jr BPV, Melo VH, Lira Neto JB. A histerossonografia na avaliação da cavidade uterina de pacientes menopausadas. Rev Bras Ginecol Obstet. 2002;24:541—5. 20. Widrich T, Bradley LD, Mitchinson AR, et al. Comparison of saline infusion sonography with office hysteroscopy for the evaluation of the endometrium. Am J Obstet Gynecol. 1996;174:1327—34. 21. Jacques E, Verma U, Whitted RW. Accuracy of saline infusion sonohysterography in diagnosis of uterine intracavitary pathology. Obstet Gynecol. 2001;97(4Suppl1):S18. 22. Kamel HS, Darwish AM, Mohamed SA. Comparison of transvaginal ultrasonography and vaginal sonohysterography in the detection of endometrial polyps. Acta Obstet Gynecol Scand. 2000;79:60—4. 23. Gunes M, Erol O, Kayikcioglu F, et al. Comparison of saline infusion sonography and histological findings in the evaluation of uterine cavity pathologies. Arch Gynecol Obstet. 2008;278:513—6. 24. Albuquerque LGT, Hardy E, Bahamondes L. Histerossonografia: avaliação da cavidade uterina com sangramento anormal. Rev Assoc Med Bras. 2006;52:247—50. 25. Karageyim Karsidag AY, Buyukbayrak EE, Kars B, et al. Transvaginal sonography, sonohysterography, and hysteroscopy for investigation of focal intrauterine lesions in women with recurrent postmenopausal bleeding after dilatation & curettage. Arch Gynecol Obstet. 2010;281:637—43. 26. Erdem M, Bilgin U, Bozkurt N, et al. Comparison of transvaginal ultrasonography and saline infusion sonohysterography in evaluating the endometrial cavity pre- and postmenopausal women with abnormal uterine bleeding. Menopause. 2007;14:846—52. 27. Moschos E, Ashfaq R, McIntire DD, et al. Saline-infusion sonography endometrial sampling compared with endometrial biopsy in diagnosing endometrial pathology. Obstet Gynecol. 2009;113:881—7. 28. Skaznik-Wikiel ME, Jelovsek JE, Andrews B, et al. Accuracy of endometrial thickness in detecting benign endometrial pathology in postmenopausal women. Menopause. 2010;17:104—8. 29. Shi A. The role of transvaginal ultrasound and sonohysterography in the evaluation of postmenopausal bleeding. Menopause. 2010;17:21—2. 1. Masters in Obstetrics and Gynecology, MDs, Gynecologists at the Municipality of Fortaleza and Ceará State Secretariat of Health, Fortaleza, CE, Brazil. 2. PhD, Professor at the School of Medicine – Universidade de Fortaleza (Unifor), Fortaleza, CE, Brazil. 3. PhD, Vice-coordinator for the Program of Mastership in Collective Health, Universidade Federal do Ceará (UFC), Fortaleza, CE, Brazil. 4. PhD, Vice-coordinator for the Department of Maternal-infantile Health, Universidade Federal do Ceará (UFC), Fortaleza, CE, Brazil. Mailing Address: Dr. Francisco Herlânio Costa Carvalho Departamento de Saúde Comunitária – UFC Rua Professor Costa Mendes, 1608, 5º andar, Bairro Rodolfo Teófilo Fortaleza, CE, Brazil, 60430-140 E-mail: herlaniocosta@uol.com.br Received February 9, 2011. Accepted after revision April 27, 2011. Study developed at Maternidade-Escola Assis Chateaubriand – Universidade Federal do Ceará (UFC), Fortaleza, CE, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554