Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 2 - Mar. / Apr. of 2011
Vol. 44 nº 2 - Mar. / Apr. of 2011
|
ORIGINAL ARTICLE
|
|
Utilization of radiation protection gear for absorbed dose reduction: an integrative literature review |
|
|
Autho(rs): Flávio Augusto Penna Soares1; Aline Garcia Pereira2; Rita de Cássia Flôr3 |
|
|
Keywords: Radiation protection; Dose in computed tomography; Dose reduction; Radiation protection gear. |
|
|
Abstract: INTRODUCTION
The use of ionizing radiation for diagnostic and therapeutic purposes has been increasing as a result of developments in equipment and easier access to radiographic exams. In Brazil, such utilization has been increasing at yearly rates of approximately 10%, with imaging diagnosis studies having increased 45.27%(1) between December/2000 and 2006 according to data reported by Datasus (the IT Department of the Brazilian Public Health System). In the same period, in the State of Santa Catarina, such increase reached 57.16%(2). As regards imaging diagnosis equipment available in Brazilian health centers, there was a 5.48% increase between 2002 and 2005, according to Instituto Brasileiro de Geografia e Estatística (IBGE) (Brazilian Institute of Geography and Statistics)(3,4). The use of radiation in medical diagnosis is highly beneficial, allowing the detection of tumors and fractures (at conventional radiography, computed tomography and mammography), and for the treatment of diseases (radiotherapy) such as cancer. Radiation also is present nuclear medicine, for the investigation of the physiology of organs and systems of the human body. However, the interaction between radiation and human tissues may cause biological effects. Such effects were noted immediately after the discovery of the X-rays, when skin disorders appeared on the skin of people exposed to X-rays, a fact which prompted scientists to investigate the possible causes of such disorders. The manifestation of such biological effects occurs in two different manners: the deterministic effect, caused by high doses of radiations in a short time span, and the stochastic effect caused by low radiation doses received over a long time span. Such effects lead to diseases already diagnosed such as radiogenic cataracts, radiodermatitis and sterility, among others. Therefore, professionals working in radiology centers should at all times resort to radiological protection principles and carefully avoid exposure to radiation, and also protect the patients from unnecessary exposure to radiation. The term “dose” utilized in the present article can be understood as absorbed dose, which is defined as the amount of energy deposited on matter by the photons or ionizing particles per unit of mass, and so has the unit Joule per kilogram (J/kg), also referred to as gray (Gy). On the other hand, the equivalent dose is the ratio between the mean absorbed dose in the organ or tissue and the radiation weighting factor, with such factor taking into consideration the tissue/organ radiosensitivity. In the international system, its unit for the equivalent dose is also J/kg, however in order to differentiate it from the absorbed dose, it received the special name of sievert (Sv). Another term of interest in the radiation measurement process is “radiation exposure unit”, which is defined as the amount of electrical charge produced in an amount of mass by the passage of radiation, and its unit in the international system is the roentgen (R). The simple, effective and low-cost way to protect occupationally exposed individuals as well as the patients submitted to ionizing radiation, is the use of radiation protection gear (RPG). It is important to clarify the use of the RPG acronym. It is used in substitution of “individual protection equipment” as, according to the Associação Brasileira de Normas Técnicas (ABNT) (Brazilian Association of Technical Standards)( 5) and the regulating Standard No. 6(6), the term “gear” is utilized to designate protection of the whole body and also of the chest, as in the case of lead aprons. The other types of equipment used for radiation exposure protection are not mentioned in this regulating standard, with the sole exception of lead gloves. Even so, in order to be considered individual protection equipment according to the law, lead aprons and gloves must be compliant with rigorous manufacturing criteria, and only after testing and certification by the Ministério do Trabalho e Emprego (MTE, 2006)(6) (Ministry of Labor and Employment) they can receive the denomination seal. For such reason, the herein utilized acronym RPG comprises all accessories for radiological protection such as: goggles, gloves, aprons, thyroid protection shield, gonadal protection shields, vests and skirts, among others. The present article is an integrative review that is aimed at identifying in the literature, publications related to the forms of protection of individuals occupationally exposed to ionizing radiations, as well as protection of patients submitted to medical exposures, demonstrating the efficiency of protectors and encouraging their utilization. MATERIALS AND METHODS The present bibliographic research was based on the assumptions of an integrative review. The integrative review is defined as that in which previously published researches are synthesized and generate conclusion on a theme of interest(7). Such method was chosen as it allows a wide and systematic analysis of scientific papers, with characterization and analysis of theoretical foundations and production trends related to the use of RPGs. In this research, the review comprised the following phases: theme identification; definition of inclusion and exclusion criteria; summary of selected themes and evaluation of studies included in the integrative review; categorization of the studies; results interpretation and presentation of knowledge review(8). The bibliographic survey was carried out at the Centro Latino-Americano e do Caribe de Informação em Ciências da Saúde (Bireme), Lilacs, PubMed/Medline, ScienceDirect, and SpringerLink databases. The search in the databases was developed over the period of 2008–2009, considering the following search descriptors in the Portuguese language: redução de dose (dose reduction); aventais de chumbo (lead aprons); radiologia (radiology); raios X (X-rays); proteção radiológica (radiological protection); dose absorvida (absorbed dose); vestimentas de proteção radiológica (radiation protection gear). The latter was found in a monograph, and although it is not an indexed term, it is being utilized for being easily understandable. In the search in the English language, the utilized descriptors were the following: lead apron; dose reduction; protective garment; protective gear; x-ray; computed tomography; apron; fluoroscopy; radiation protection. The selection of publications was carried out by means of careful reading of abstracts and ensuing text reading, in order to evaluate the relationship with the theme to be researched. The computer program IPEM report 78 of Institute of Physics and Engineering in Medicine (IPEM)(9) was also utilized for calculating air kerma rates, with the purpose of scientifically corroborating the results presented in the studies. Thus, the sample comprised 21 articles, most of them in English. Other sources such as thesis, monographs and books contributed with reports on the biological effects associated with radiation, forms of protection, and the practical results of the utilization of RPGs that comprised the document sources in the analysis process. RESULTS Importance of the use of RPGs The interaction of ionizing radiation with the human organism may generate biological effects, which vary with the degree of cells radiosensitivity and absorbed radiation dose. According to Biral(10), the radiosensitivity degree is inversely proportional to the cell differentiation, i.e., cells with little differentiation in their function are more radiosensitive, such as, for example, the epidermis cells, erythroblasts and spermatogonial cells. There are however, cells that challenge that rule: the oocytes and lymphocytes. Depending on the radiosensitivity, the ionizing radiation may directly affect the cells (ionization) or indirectly (action of free radicals), with damages to the DNA strands, alteration of their genetic material, as well alteration of their proteins, enzymes, and modification of permeability of the cells’ membrane and activation of the oncogenes. The human body has mechanisms to repair the damage caused by radiation, however, when they fail, the results are the incapacity of cells reproduction or their definite modification. In some cases, cellular death(11) may occur. Absorbed dose reduction in patients In order to minimize the primary and secondary radiation dose, RPGs are worn by patients. According to the ABNT Standard NBR IEC 61331(5), the RPGs are divided into devices for patients and for occupationally exposed individuals. The RPGs for patients comprise: lead aprons, gonadal aprons, scrotal shields, ovarian shields and lead curtains. The gonads contain germ cells with high cell division rates and high radiosensitivity, therefore there is great preoccupation in protecting such gland from ionizing radiation. Studies have demonstrated that the use of protective equipment during computed tomography exams considerably reduces the exposure to radiation in up to 95%(12). Hohl et al.(13) have demonstrated a reduction of 87% in an abdominal computed tomography study. Raissaki(14) has studied the application of gonadal protectors in pediatric radiology, observing an absorbed dose reduction of approximately 50% in girls’ and 95% in boys’ gonads. One of the studies developed by Parker et al.(15), on dose reduction in multislice computed tomography angiography, revealed that the dose in the breast region, during a study for suspected pulmonary embolism, may be reduced by approximately 60.6% with the utilization of a tungsten-antimony shield. The crystalline and the thyroid gland are other organs of the human system that require radiological protection, because of their great radiosensitivity. Hopper et al.(16), in their study, have demonstrated that the utilization of a bismuth shield during a chest computed tomography reduced by 60% the radiation on the thyroid gland and by 40% on the crystalline. In another study developed by Hopper(17), the utilization of bismuth eye shields reduced the radiation in the crystalline by 48.5%, while the thyroid shield reduced the dose in such gland by 67.3%, with the utilization of such protectors not causing any hindrance to the quality of the images. As regards the crystalline, other studies have demonstrated that the protection of such region reduced the dose by approximately 30-40%(18,19). According to studies developed by Brniæ et al.(20), the use of chest shielding reduces the dose by 57% in this region during a skull study. The use of the same shielding in a pediatric chest study reduces the dose by 29%(21). Such data and those from other studies may be better compared on Table 1. 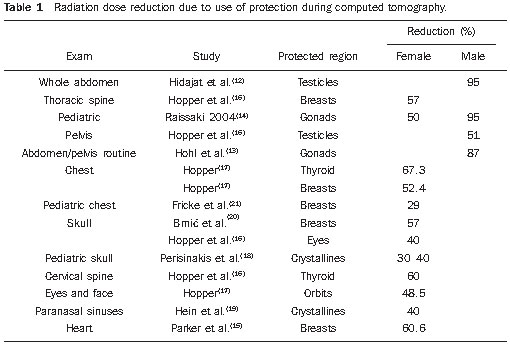 Studies on dose reduction as a function of the utilization of RPGs in conventional radiology are scarce; however, in such studies, one observes the utilization of chest shielding during a radiographic lateral study of the chest reduces the radiation dose by 88% in the uterus and ovaries region( 22). Absorbed dose reduction in occupationally exposed individuals For occupationally exposed individuals, the types of RPGs comprise lead protective aprons with lead thicknesses ranging from 0.25 to 0.50 mm, protection gloves, leaded eyewear and thyroid shield(5). In occupationally exposed individuals, a dose reduction can be observed with the utilization of RPGs during interventional procedures. According to Scremin et al.(23), the number of interventional procedures requiring radiographic images, such as those performed in hemodynamics services, has increased over the past few years due to the fact that such technique does not necessarily require surgery, involving less risk for the patients. Their study is focused on occupational exposure and has demonstrated that the use of a protective lead shielding in the form of a curtain, reduces in up to 90% and 80% the dose received in the chest region respectively by the physician and by the assisting nurse during a cardiac catheterization. During orthopedic surgeries involving interventional radiology, the hands of the physician are amongst the parts most exposed to primary radiation(24). A procedure that is quite frequently performed is percutaneous vertebroplasty, which consists of the insertion of a canula into the injured bone and injection of bone cement to restore it. A radiographic equipment is utilized to guide such canula, with almost continuous emission of radiation. Synowitz & Kiwit(25) observed that the use of protective gloves during the procedure resulted in a 75% dose reduction in the hands of the surgeon. Most of the studies are focused on the crystalline, the thyroid and the gonads, which are highly radiosensitive. However, few studies approach the radiation dose to the lower extremities of the members of the medical team. An Irish study indicates that, with the utilization of protective lead curtains mounted on the sides of the patient table, it is possible to reduce by 64% the radiation dose to the lower extremities(26). With the software IPEM Report 78 of IPEM(9) for the simulation of the spectrum emitted by tungsten targets, it is possible to evaluate the RPGs effectiveness and the influence of different material thicknesses on the radiological protection level. Simulations were performed with 55, 75, 95 and 115 kV, as they comprehend the range of voltages normally utilized in conventional radiography. The air kerma dose was calculated by unit of µGy/mAs at 75 cm from the bulb, including the inherent attenuation of 2.5 mm thick aluminum in the equipment. Based on the results obtained by the software, one have observed that the 0.25 mm thick lead protection reduces the dose by at least 86.82% (115 kV), reaching up to 99.06% (55 kV) at lower energies. With the use of 0.5 mm-thick lead shielding, the dose reduction ranges between 95.79% (115 kV) and 99.94% (55 kV). Table 2 and Figure 1 show the data comparison. 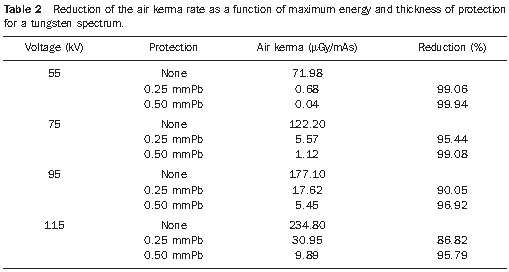 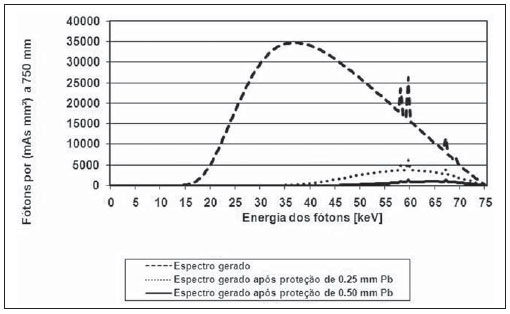 Figure 1. Energy spectrum of a tungsten target tube with inherent 2.5 mmAl filtration at 75 kV. Additionally to the reduction of air kerma, the use of RPGs considerably eliminates low-energy photons, as shown in Figure 1. This implies even greater absorbed dose reduction levels, as the low energies are contained by elements with high atomic number, such as lead. DISCUSSION The analyzed set of pieces of research clearly demonstrates contribution of studies on the developments in radiological protection, considering that, after the discovery of X-radiation by Roentgen in 1895, while radiographies were performed, skin disorders started to manifest in workers. Crocker(27) was the pioneer in study on diseases attributed to radiation exposure. In 1897, this physicist related the occurrence of dermatitis and skin ulcers with the prolonged use of the Crookes’ bulb near the body. Knowing that the lesions were similar to severe sun burns, for which the suggested protection was to cover the body with something black, he proposed that occupationally exposed individuals utilized red gloves or covered their hands and faces with red paint. At that time, it was a common belief that such pigments were effective barriers against ionizing radiation. In 1902, Rollins proposed three ways to decrease workers’ and patients’ exposure to radiation, as follows: utilizing absorbing eyewear, encapsulating the X-ray tubes in lead and limiting the field of irradiation to the region of clinical interest by means of protective materials. However, such recommendations were not followed for a long time. Starting in 1913, the British and Germans produced radiological protection reference guidelines, recommending the utilization of protective equipment by workers. In the period between 1922 and 1928, North Americans and the British published recommendations for workers, indicating dose tolerance levels and determining barriers for worker protection. In 1928, during the Second International Congress of Radiology in Stockholm, the International Commission on Radiological Protection (ICRP) was created, with the purpose of defining guidelines on radiological protection to be adopted by most of the countries in the world(28). According to Archer(29), after the Congress in Stockholm, the National Bureau of Standards (NBS) of the United States of America established the Advisory Committee on X-Ray and Radium Protection (ACRP), a committee that published its first report in 1931, with the title of X-Ray Protection. In 1964, the ACRP was reorganized and transformed into the widely known National Council on Radiation Protection and Measurements (NCRP). In 1961 the ACRP and NBS joined in the publication of a report titled Medical XRay Protection up to Three Million Volts, that later came to be known as NCRP No. 26, introducing many of the common radiological protection principles and methods that are still utilized today. In this same report, the concepts of work load and usage factor were established, in order to more concisely describe accidental exposure and the use of barriers to avoid them. The NCRP Report No. 49 (1976) was the first guideline utilized by American competent experts as a reference to specify radiation protectors in medical X-ray imaging installations. In the nineties, the need to modify such report became noticeable, as it did not approach new technologies such as computed tomography and mammography. The dose limit values, work load and occupation factors, among others, were modified, and two new reports were issued, the reports No.116 and No.147(30). In Brazil, the international regulations were effectively adopted by means of the Ministry of Health Ordinance 453(31), in July of 1998, highlighting the utilization of radiation provided it is beneficial for the health at individual and/or society levels. Another important contribution demonstrated by studies on radiation protection was the knowledge on the biological effects of ionizing radiations. Such studies reveal the cells radiosensitivity and effects on the human body. The ionizing radiation is an electromagnetic wave that interacts with matter transferring energy to the electrons of its atoms. With the energy gain, such atoms start leaving their orbits, changing their electronic or even atoms layers, dissipating the energy in the form of additional radiation, or ionizing other atoms. Such production of free radicals may induce radiobiological effects such as induced chromosomal breaks. Such biological damage depends on the deposited energy (absorbed radiation dose) on the tissue or organ and on the radiosensitivity of such tissue or organ. The biological effect on the human body manifests in two manners. One of them is the deterministic effect, caused by the high radiation dose that leads the cell to a partial or total loss of its biological function, i.e., cellular death. The irradiated individual may present with temporary or permanent sterility, radiodermatitis, nausea, fatigue, cataracts, among other effects. The other form of manifestation is the stochastic one, where small doses of radiation over a long period of time cause genetic mutations. In cases where such mutation occurs in germ cells, the damage causes a hereditary change. In cases where the mutation occurs in somatic cells, there will be a high probability of an individual to develop cancer, particularly in most sensitive regions such as breasts, gonads, bone marrow and lymphatic tissues. The utilization of RPGs is of utmost importance to minimize such an effect(11). Another significant contribution demonstrated in the present review refers to the implementation of measures for radiological protection. The studies mention the Standards of Comissão Nacional de Energia Nuclear (CNEN)(32) (National Committee on Nuclear Energy) that, based on three fundamental principles of radiation protection, established measures against possible effects that may be caused by ionizing radiation, as follows: justification – the medical exposure to radiation will only be acceptable if it results in benefits for the society or to the individual; dose limitation – the exposure to radiation must be restricted to the region of interest, never exceeding the allowed dose limits; optimization – the dose to the patient shall be the lowest possible, without affecting the images quality. This latter principle is related to the ALARA (As Low As Reasonably Achievable) philosophy, that implies in always decreasing the dose of radiation exposure both for the patient and the occupationally exposed individual. According to Gelsleichter(33), all these principles support the main radiological protection mechanisms: distance from the radiation source, time of exposure the source and shielding. The first two mechanisms consist of measures that minimize the exposure, and the third one consists in fixed barriers or accessories that block the trajectory of the X-ray beams, absorbing them. Two types of barriers are utilized in radiological protection: room shielding for collective protection, and RPGs for individual protection. The RPGs are placed between the source of radiation and the patient, so as to attenuate the radiation that reaches the body. The same applies for occupationally exposed individuals wearing them. Such gear are manufactured from materials with high atomic level (normally lead or its compounds) to block the passage of X-rays photons, besides other washable material that protects the radiation absorbing material. As regards the dose reduction principles, the images acquisition time in a radiological study cannot be reduced as a function of the established radiological technique, as it would imply in loss of image quality; and the increase in the distance from the radiation source is not always possible, as the distance between the source and the command table poses a limitation. Thus, the use of RPGs at in centers of radiology and imaging diagnosis is actually the only effective way to reduce exposure to ionizing radiation of occupationally exposed individuals, as well as medical exposure of patients. Ordinance 453(31), in its item 5.5 establishes that for each X-ray unit there must be a RPG, and such RPG must assure protection to the chest of patients, including the thyroid and gonads, with at least 0.25 mm of lead-equivalent material (mmPb). Additionally, at item 5.10a, the Ordinance determines that in case an individual needs to assist a debilitated patient, such individual must wear a lead apron with a minimum of 0.25 mmPb. As regards professionals, the item 4.26a (ii) item determines that, during radiological procedures, professionals must protect themselves against scattered radiation by wearing RPGs or protective barriers with no less than 0.25 mmPb attenuation. As regards fluoroscopy, item 4.17d determines that the examination room must be equipped with a inferior/lateral lead curtain or skirt to protect the worker against the radiation scattered by the patient, with a thickness = 0.5 mmPb, at 100kVp; and item 4.40 establishes that lead gloves with at least 0.25mmPb must be worn. It is a known fact that radiology professionals resist the use of RPGs, as they are not comfortable because of their heavy weight, which may cause back pain if worn for long periods of time(34). However, it is necessary that occupationally exposed individuals wear RPGs during interventional procedures, as well as in procedures in which the individual is directly exposed to the primary or secondary beam. Additionally, the professional must be aware that whenever possible the patient must wear the RPG during computed tomography scans, conventional radiographic studies, or during interventional procedures in order to protect areas that are exposed to radiation, be such radiation primary or secondary, and that the use of RPG will not affect the image quality. Considering the troubles associated with wearing the RPGs, new materials have been developed to make such gear lighter so as to reduce the professionals fatigue and back pain(35) and the discomfort in wearing them, thus contributing to a reduction in the resistance to the use of RPGs. Studies demonstrate that the use of lead aprons is effective, as they attenuate a large amount of ionizing radiation. Theoretically, it is possible to prove that the lead shielding (0.25 mmPb) at 75 kV is capable of reducing the dose to the patient or to occupationally exposed individuals in up to 95%(9). In practice, the material is not always homogeneous, therefore the attenuation ends up being lower than the theoretical attenuation, but even so this material is important and still efficient. According to Hopper(16), a thyroid shield is capable of attenuating up to 67.3% of the X-radiation. Taking into account that the RPG is not always in perfect conditions, it is necessary to perform some tests, as defined on item 4.45b(x) of Ordinance 453(31), with the purpose of evaluating the quality of the material utilized at the center. Because of the radiobiological effects, such as radiogenic cataracts, sterility, cellular death and genetic mutations that may occur with the utilization of ionizing radiation, any gains related to attenuation of radiation is significant, and for such reason the utilization of RPGs is indispensable. CONCLUSIONS In the present study, the efficiency of the utilization of RPGs by the patient and by occupationally exposed individuals was analyzed, observing that the increasing utilization of radiation implies increased necessity of radiological protection, with all results clearly demonstrating that the utilization of RPGs is directly related to dose reduction, both for the occupationally exposed individual and the patient. The use of RPGs has shown to be effective and follows the ALARA principle, i.e., the radiation is utilized at the minimum necessary doses for the patient and the professional in the area. The utilization of RPGs implies a reduction of the absorbed dose, particularly in the patients’ gonads, with a reduction ranging between 87%(13) and 95%(14), and thyroid gland, with a reduction ranging from 60%(16) to 67,30%(17). In occupationally exposed individuals, there was a significant reduction in the exposure of the surgeons’ hands (75%)(25). Also lower extremities were analyzed, with a reduction of 64%(26) of the absorbed dose. Relatively few studies on X-rays were found in the literature, indicating the need for more studies on the RPGs effectiveness, particularly in conventional radiology. Further studies approaching quality indices, compliance tests and technical specifications of RPGs for patient protection must be defined. As regards occupationally exposed individuals, continued education on the subject is recommended at the centers, so that the health professionals become increasingly aware of the relevance of the utilization of such garments for protection of their own health and safety against ionizing radiations at work. REFERENCES 1. Departamento de Informática do SUS – DATASUS. Informações de saúde. [acessado em 14 de outubro de 2008]. Disponível em: http://tabnet.datasus.gov.br/cgi/deftohtm.exe?sia/cnv/pauf.def 2. Departamento de Informática do SUS – DATASUS. Informações de Saúde. [acessado em 14 de outubro de 2008]. Disponível em: http://tabnet.datasus.gov.br/cgi/tabcgi.exe?sia/cnv/pasc.def 3. Instituto Brasileiro de Geografia e Estatística – IBGE. Pesquisa. Pesquisa de assistência médicosanitária. [acessado em 14 de outubro de 2008]. Disponível em: http://www.ibge.gov.br/home/ estatistica/populacao/condicaodevida/ams/ default.shtm 4. Instituto Brasileiro de Geografia e Estatística – IBGE. Pesquisa. Pesquisa de assistência médicosanitária. Tabelas. [acessado em 14 de outubro de 2008]. Disponível em: http://www.ibge.gov.br/ home/estatistica/populacao/condicaodevida/ams/ 2005/defaulttab.shtm 5. Associação Brasileira de Normas Técnicas – ABNT. Dispositivos de proteção contra radiação- X para fins de diagnóstico médico. ABNT NBR IEC 61331. Rio de Janeiro, RJ: Associação Brasileira de Normas Técnicas; 2004 6. Brasil. Ministério do Trabalho. Portaria MTB nº 3.214, de 08 de junho de 1978. Aprova as normas regulamentadoras – NR – do Capítulo V, Título II, da consolidação das leis do trabalho, relativas à segurança e medicina do trabalho. NR-6 – Equipamento de proteção individual-EPI. Portaria SIT/DSST nº 162, de 12 de junho de 2006. Brasília, DF: Diário Oficial da União; 16/05/2006. 7. Rodgers BL, Knafl KA. Concept development in nursing: foundations, techniques and applications. Philadelphia, PA: WB Saunders; 1993. 8. Mendes KDS, Silveira RCCP, Galvão CM. Revisão integrativa: método de pesquisa para a incorporação de evidências na saúde e na enfermagem. Texto & Contexto Enferm. 2008;17:758–64. 9. Sutton D, Cranley K, Gilmore BJ, et al. Catalogue of diagnostic X-ray spectra and other data: electronic version – Report S. No. 78 (CD Rom). York, UK: The Institute of Physics and Engineering in Medicine; 1997. 10. Biral AR. Radiações ionizantes para médicos, físicos e leigos. Florianópolis, SC: Editora Insular; 2002. 11. Dimenstein R, Hornos YMM. Manual de proteção radiológica aplicada ao radiodiagnóstico. São Paulo, SP: Editora Senac; 2001. 12. Hidajat N, Schröder RJ, Vogl T, et al. The efficacy of lead shielding in patient dosage reduction in computed tomography. RöFo. 1996;165:462–5. 13. Hohl C, Mahnken AH, Klotz E, et al. Radiation dose reduction to the male gonads during MDCT: the effectiveness of a lead shield. AJR Am J Roentgenol. 2005;184:128–30. 14. Raissaki MT. Pediatric radiation protection. Eur Radiol Syllabus. 2004;14:74–83. 15. Parker MS, Kelleher NM, Hoots JA, et al. Absorbed radiation dose of the female breast during diagnostic multidetector chest CT and dose reduction with a tungsten-antimony composite breast shield: preliminary results. Clin Radiol. 2008;63:278–88. 16. Hopper KD, King SH, Lobell ME, et al. The breast: in-plane x-ray protection during diagnostic thoracic CT – shielding with bismuth radioprotective garments. Radiology. 1997;205:853–8. 17. Hopper KD. Orbital, thyroid, and breast superficial radiation shielding for patients undergoing diagnostic CT. Semin Ultrasound CT MR. 2002; 23:423–7. 18. Perisinakis K, Raissaki M, Theocharopoulos N, et al. Reduction of eye lens radiation dose by orbital bismuth shielding in pediatric patients undergoing CT of the head: a Monte Carlo study. Med Phys. 2005;32:1024–30. 19. Hein E, Rogalla P, Klingebiel R, et al. Low-dose CT of the paranasal sinuses with eye lens protection: effect on image quality and radiation dose. Eur Radiol. 2002;12:1693–6. 20. Brniƒ Z, Vekiƒ B, Hebrang A, et al. Efficacy of breast shielding during CT of the head. Eur Radiol. 2003;13:2436–40. 21. Fricke BL, Donnelly LF, Frush DP, et al. In-plane bismuth breast shields for pediatric CT: effects on radiation dose and image quality using experimental and clinical data. AJR Am J Roentgenol. 2003;180:407–11. 22. Jackson G, Brennan PC. Radio-protective aprons during radiological examinations of the thorax: an optimum strategy. Radiat Prot Dosimetry. 2006;121:391–4. 23. Scremin SCG, Schelin HR, Tilly Jr JG. Avaliação da exposição ocupacional em procedimentos de hemodinâmica. Radiol Bras. 2006;39:123–6. 24. Hafez MA, Smith RM, Matthews SJ, et al. Radiation exposure to the hands of orthopaedic surgeons: are we underestimating the risk? Arch Orthop Trauma Surg. 2005;125:330–5. 25. Synowitz M, Kiwit J. Surgeon’s radiation exposure during percutaneous vertebroplasty. J Neurosurg Spine. 2006;4:106–9. 26. Shortt CP, Al-Hashimi H, Malone L, et al. Staff radiation doses to the lower extremities in interventional radiology. Cardiovasc Intervent Radiol. 2007;30:1206–9. 27. Crocker HR. A case of dermatitis from Roentgen rays. Br Med J. 1897;1:8–9. 28. Costa PR. Modelo para determinação de espessuras de barreiras protetoras em salas para radiologia diagnóstica [tese]. São Paulo, SP: Instituto de Pesquisas Energéticas e Nucleares; 1999. 29. Archer BR. History of the shielding of diagnostic x-ray facilities. Health Phys. 1995;69:750–8. 30. Archer BR. Recent history of the shielding of medical x-ray imaging facilities. Health Phys. 2005;88:579–86. 31. Brasil. Ministério da Saúde. Secretaria de Vigilância Sanitária. Diretrizes de proteção radiológica em radiodiagnóstico médico e odontológico. Portaria nº 453, de 1º de junho de 1998. Brasília, DF: Diário Oficial da União, 2 de junho de 1998. 32. Brasil. Ministério da Ciência e Tecnologia. Comissão Nacional de Energia Nuclear. Radioproteção. CNEN-NN-3.01 – Diretrizes básicas de proteção radiológica. [acessado em 25 de outubro de 2008]. Disponível em: http://www.cnen.gov.br/seguranca/normas/mostra-norma.asp?op=301 33. Gelsleichter AM. Condições das vestimentas de proteção radiológica em dois hospitais públicos de Florianópolis [trabalho de conclusão de curso]. Florianópolis, SC: Centro Federal de Educação Tecnológica; 2006. 34. Moore B, vanSonnenberg E, Casola G, et al. The relationship between back pain and lead apron use in radiologists. AJR Am J Roentgenol. 1992; 158:191–3. 35. Scuderi GJ, Brusovanik GV, Campbell DR, et al. Evaluation of non-lead based protective radiological material in spinal surgery. Spine J. 2006;6: 577–82. 1. PhD of Physics, Professor at Instituto Federal de Santa Catarina (IFSC), Florianópolis, SC, Brazil. 2. Radiologist Technologist, Consultant for the Sinan Project (Sistema de Informação de Agravos de Notificação), Florianópolis, SC, Brazil. 3. PhD of Nursing Science, Professor at Instituto Federal de Santa Catarina (IFSC), Florianópolis, SC, Brazil. Mailing Address: Aline Garcia Pereira Instituto Federal de Santa Catarina, Campus Florianópolis – DASS Avenida Mauro Ramos, 950, Centro Florianópolis, SC, Brazil, 88020-300 E-mail: aalinegp@gmail.com Received February 4, 2010. Accepted after revision February 17, 2011. Study developed at Instituto Federal de Santa Catarina (IFSC) – Florianópolis Campus, Florianópolis, SC, Brazil. Financial support: Conselho Nacional de Desenvolvimento Científico e Tecnológico (CNPq). |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554