INTRODUCTION
Technological developments in the field of imaging methods utilizing ionizing radiations have allowed the performance of minimally invasive surgeries in different areas of medicine, particularly interventional cardiology. The safety, credibility and effectiveness of such invasive techniques have allowed the performance of increasingly complex and sophisticated interventions, with the advantage of being less aggressive to patients yielding clinical benefits comparable to those of conventional surgery(1).
However, such procedures expose both the patient and the medical team to high radiation doses. Several studies have demonstrated high skin entrance doses in patients, causing erythema and, in some cases, skin necrosis(2,3).
The absorbed dose on the patient’s skin surface can be determined by means of appropriate dosimeters, or estimated from dose indicators parameters displayed by the angiographic system during the clinical procedure, such as “cumulative dose” (K
a,r) and air kerma area product (P
KA)(4,5). This cumulative dose, internationally denominated as cumulative reference point air kerma, is calculated from the irradiation parameters selected by the fluoroscopic angiographic C arm during the clinical procedure. The reference for such calculation is a point denominated interventional reference point (IRP), defined by the IEC 601- 2-43 standard, and is located on the central axis, at 15 cm from the isocenter towards the focal point. The IRP is defined as the location that represents the beam entrance into the patient’s skin(5,6). The skin absorbed dose in the most irradiated region and the K
a,r are considered as the appropriate magnitudes for estimating the risk for occurrence of deterministic effects (such as erythema, alopecia and sterility), while P
KA is utilized for estimating the occurrence of stochastic effects (such as cancer)(5,6).
The International Commission on Radiological Protection (ICRP) recommends that, in interventional procedures, the values and location of maximum cumulative skin dose (MSD) be registered on the hospital files or on the patient’s records, whenever such dose exceeds 1,000 mGy in procedures which may need to be repeated, such as in cardiology, in case of restenosis (reoccurrence of obstruction of an artery previously treated by means of angioplasty). The ICRP and several guidelines also recommends clinical follow-up and recording of such data in case of any interventional procedure in which MSD exceeds 3,000 mGy, K
a,r exceeds 5,000 mGy or P
KA exceeds 500 Gy.cm
2(5,7).
Besides the patient who is directly exposed to the primary radiation beam, professionals, particularly physicians, also receive high doses as they are exposed to the scattered radiation, because they need to be in close proximity with the patients during the procedures. The radiation dose values may also be high as a function of the number of procedures performed by the physician. Studies developed by the American Society of Cardiovascular and Interventional Radiology demonstrated that high radiation doses have been observed even in cases where modern apparatuses are utilized by qualified professionals(8,9). According to Filippova, cardiologists are the professionals who receive the highest doses(10).
The present study was aimed at evaluating the radiation dose levels in interventional cardiology procedures such as transluminal coronary angioplasty at a hospital where such procedures are routinely performed. The relevance of the present study is to provide data for physicians, contributing to the optimization of the radiation dose reduction both for patients and for the medical team.
MATERIALS AND METHODS
In the present study, 34 procedures of percutaneous transluminal coronary artery angioplasty, with and without placement of stents, were analyzed. All the procedures were performed in a public hospital in the city of Recife, PE, Brazil, between April of 2007 and September of 2009.
The equipment utilized for such procedures was an Integris Allura 12 monoplanar angiography system (Philips Medical Systems; Best, The Netherlands), equipped with a 3-phase X-ray generator and a microprocessor high frequency converter, nominal voltage 40–150 kV and maximum current of 1 A. The X-ray tube had focal points at 0.5 and 0.8 mm and was equipped with two collimators, one of them of the iris type (automatic) and the other of the rectangular type (manual). The X-ray beam filtration was done with 2.5 mmAl at 100 kV, besides added filtration with aluminum and copper selected by software. The image intensifier had a diameter of 30 cm, with four fields of view (30/22/17/12 cm), selectable by the physician. Neither the leaded drape nor a lead glass window was installed in the equipment. Such devices aid in the reduction of the incidence of scattered radiation on the physician(11).
All the procedures were performed with the normal pulsed fluoroscopy mode (30 pulses per second) and pulsed cinegraphy mode (15 images per second), with normal images matrix (512 × 512). In the fluoroscopy mode, the images are viewed in real time and are not recorded, while at the cinegraphy mode the images are recorded in a cinegraphic sequence (filming) to be viewed after the procedure. Fluoroscopy and cinegraphy modes may be pulsed or continuous, according to the X-rays produced by the generator.
The randomly selected patients sample included 31 adults, with no restriction regarding gender, age or weight, and was based on the elective scheduling of the hospital hemodynamics unit. Three of the 31 patients underwent two procedures over the study period, and 21 patients were clinically followed-up after the procedure, with the purpose of checking for skin lesions. Nine of such patients had their backs photographed and were evaluated by the physicians both before and 14 days after the procedure, in compliance with international recommendations(8).
The present study was approved by the Committee for Ethics in Research of the hospital. The patients or their guardians who agreed to participate in the study were appropriately informed on the risks and benefits of the research and signed a term of free and informed consent in compliance with the requirements defined by the Resolution CNS 196/96 that regulates research involving human beings in Brazil(12).
The physicians sample included two professionals specialized in interventional cardiology, from the hospital medical staff. The dosimetric monitoring was performed on the physician who performed the procedure. The physician assistant, when present, was not monitored.
Radiation on patients
The patients’ dosimetry was approached in two manners as follows:
1. Evaluation of “cumulative dose” (Ka,r) and PKA
Amongst the data provided by the angiography equipment during the procedures, the following data were recorded: level (normal/high/low) and mode (continuous/ pulsed) of fluoroscopy and cinegraphy; total number of images acquired in the cinegraphy mode; and fluoroscopy time (min). Also, the angle and rotation of the C-arm (X-ray tube and image intensifier) were recorded for each projection of the radiation fields resulting in the different magnifications of the images intensifier; the distances between the focal point and the intensifier (source to image detector distance – SID) and between the focal point and the patient (source to skin distance – SSD); and irradiation parameters such as voltage (kV), pulse width (ms) and current (mA) applied to the X-ray tube.
Based on the irradiation parameters (kV, mA and ms) which are automatically selected by the equipment according to the utilized projections, the patient characteristics and radiographic contrast, the angiographic equipment calculates the K
a,r Such calculation is performed with reference to a (IRP) point, without considering backscattering, as defined by the IEC 601-2-43 Standard(6). From the value of K
a,r it was possible to calculate the incident air kerma K
a,i (mGy) at the point corresponding to the patient skin surface (at the level of the table surface), taking into consideration the variation of radiation intensity with the inverse square distance. Considering that K
a,r does not account for the contribution of the radiation scattered by the patient, for determining the patient’s skin entrance surface air kerma (K
a,e) the K
a,i was multiplied by a backscattering factor (1.3). Such backscattering factor represents the contribution of radiation that is scattered from the central beam due to the presence of the surgical table, the mattress and the patient himself.
With the distance from the intensifier to the X-ray tube and the diameter of the irradiation field, the irradiated area was calculated for each angle/rotation at the level of the surgical table, by utilizing the appropriate geometrical factors. With such values, P
KA was calculated by multiplying K
a,i by the obtained area. Total P
KA was calculated by summing up the partial P
KA at the different projections utilized in the procedure.
2. Radiochromic film dosimetry
In order to evaluate the radiation distribution and location of the maximum absorbed dose on the backs of nine patients, radiochromic films of the GafChromic XR V2 (International Specialty Products; New Jersey, USA) type were utilized. Such films are available in the 35 × 43 cm format and are developed for uses in dosimetry in patients during fluoroscopy and radiotherapy procedures. The films were positioned over the surgical table at the level of the posterior chest area, with the white face of the film positioned towards the entrance of the X-ray beam, according to the film manufacturer’s usage instructions(13). The film was wrapped in a black plastic envelope to protect it from light as well as from liquid products utilized in the asepsis of the patient.
The radiation changes the colors of the radiochromic film in such a manner that the most darkened areas correspond to the most irradiated areas. The entrance surface air kerma – K
a,e (mGy) – was estimated from the readings of the optical density on these darkened areas, 24 hours after the procedure, in order to assure the stability of the film’s optical absorbance, as recommended by the manufacturer, and by the application of calibration factors established at the Laboratory of Metrology of Ionizing Radiations, Department of Nuclear Energy of Universidade Federal de Pernambuco (LMRI/DEN/UFPE)(13,14).
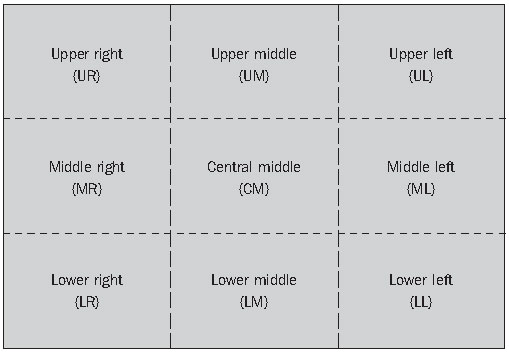
In order to establish a relationship between the location of the most irradiated areas on the films and the regions on the backs of the patients, the film was divided into nine regions as follows: upper right side (UR), middle right side (MR) and lower right side (LR), upper middle (UM), central middle (CM), lower middle (LM), and upper left side (UL), middle left side (ML) and lower left side (LL), as shown on Figure 1.
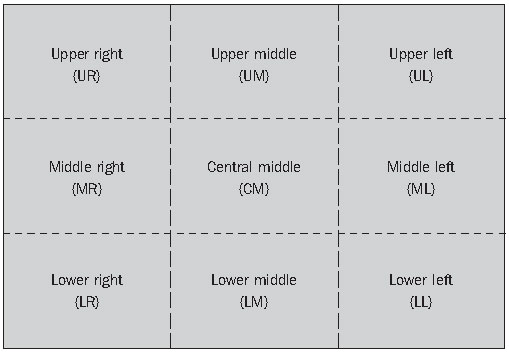
Figure 1. Regions of the radiochromic film.
The maximum skin dose (MSD) on the patient’s skin surface was calculated by multiplying the highest value of K
a,e, determined by the optical density on the surface of the film, by an energy absorption coefficient (1.054) that relates the absorption of radiation on human tissue with the absorption of radiation in the air, as in the case of K
a,e.
Radiation on physicians
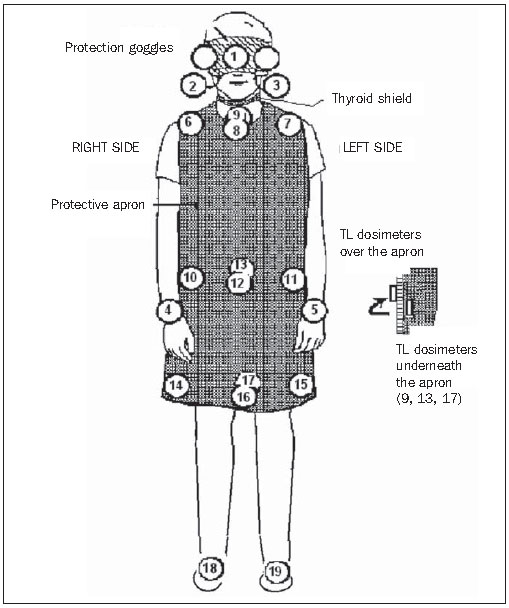
On the physicians, the dosimetry was performed with 38 TL dosimeters (TLD- 100) distributed in pairs as shown on Figure 2.
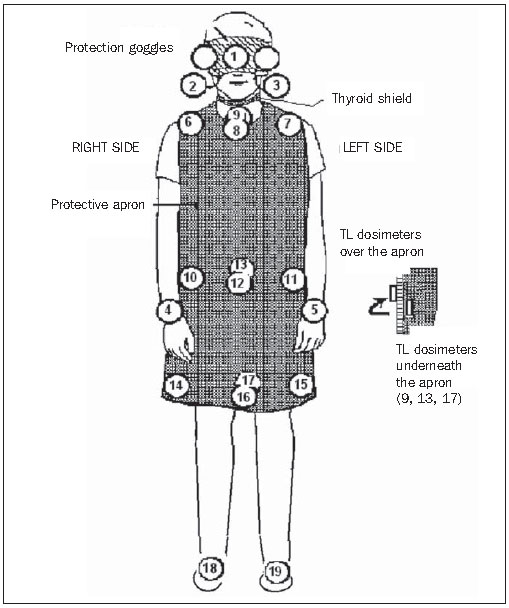
Figure 2. Location of the TL dosimeters over the apron and on the body of the physicians: face – forehead (1) right eye region (2) and left eye region (3); upper limbs –hands, at the wrist level, inside the procedure glove [right hand (4) and left hand (5)]; thyroid region – on the external surface of the thyroid shield (8) and inside the thyroid shield (9); torso – at the level of the shoulders, over the apron, right side (6) and left side (7); thorax - lower abdomen – at waist level: on the apron, right side (10), left side (11), at the middle, over the apron (12) at the middle, underneath the apron (13); at the knee level, over the apron, right side (14) and left side (15), at the middle, over the external surface (16) and inside the apron (17); lower limbs – feet, anterior region, right foot (18) and left foot (19).
The effective dose E (mSv) was estimated from the measurements obtained with the TL dosimeters placed at the level of the neck, over the thyroid protector, and another at the level of the waist, under the protective apron (TL 8 and 13, respectively, shown on Figure 2), and utilizing the Niklason algorithm(15), as follows:
E = 0.02 (HO – HU) + HU
where:
HO corresponds to the value of H
P(0.07) (mSv) for the TL (8) dosimeter measurement and
HU is the value of H
P(10) (mSv) obtained by the TL (13) dosimeter.
The readings from the TL dosimeters (8 and 13) were corrected by means of the coefficients defined at ICRP 74(16) for the conversion of such measurements into the corresponding personal dose equivalents H
P(0.07) and H
P(10), respectively.
RESULTS
Radiation on patients
The 31 evaluated adult patients (39% women and 61% men) were between 36 and 78 years old (60 ± 11 years), weighted between 49 and 116 kg (73 ± 14 kg) and were between 1.50 e 1.80 m tall (1.63 ± 0.10 m). The values in parenthesis represent the mean standard deviation (M ± 1s).
The results of the dosimetric evaluation by the described methods were the following:
1. Evaluation of “cumulative dose” (Ka,r) and PKA
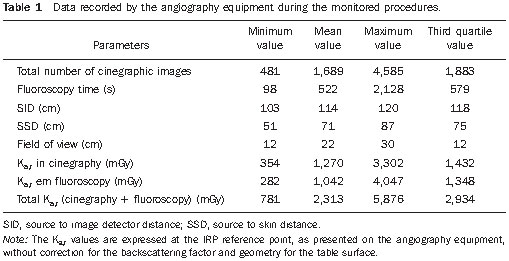
Minimum, mean, maximum and third quartile values of the parameters recorded by the equipment during the procedures are shown on Table 1.
On Table 1, one observes that the K
a,r values, both at fluoroscopy and cinegraphy, are practically the same, in spite of the differences between patients and procedures.
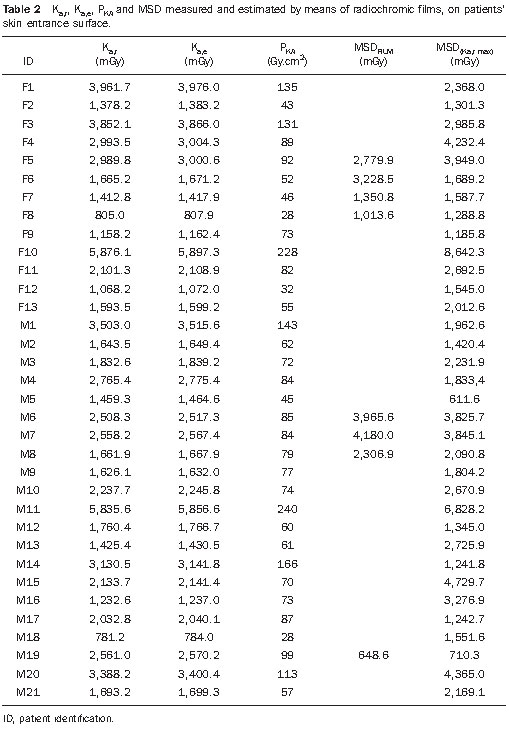
On Table 2, the values for K
a,r, K
a,e, P
KA are expressed at the level of skin entrance surface. As regards P
KA values, one observes that none of the patients exceed 500 Gy.cm
2 in a single procedure.
2. Radiochromic film dosimetry
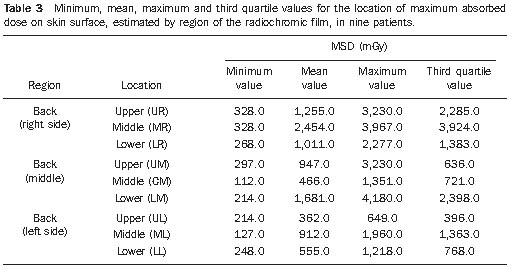
The results for absorbed dose distribution by utilizing the radiochromic film in nine patients are summarized on Table 3.
The results for localization of the maximum absorbed dose indicated higher doses at the middle right side (MR) and lower middle side (LM) of the film, corresponding to the right lower middle and lower middle regions of the patients’ backs. Such locations are consistent with clinical studies, as 65% of the patients presented lesions in the left coronary vessels, which causes the most irradiated areas to be located between the middle and the right side of the backs.
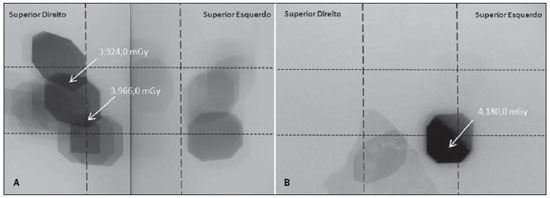
The images with the dose distribution on the backs of the two patients with the highest doses are shown on Figure 3. At the first image (Figure 3A) one observes that in spite of the utilization of different angles, the MSD is located in a region with fields overlapping; at the second image (Figure 3B), the MSD is a result of the projection most utilized in the procedure.
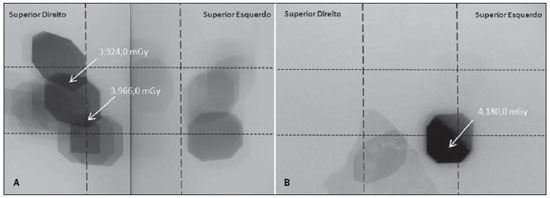
Figure 3. Image demonstrating the dose distribution (K
a,e) on the film’s surface of two patients who presented the highest doses.
The maximum absorbed dose on skin surface, determined with radiochromic film (MSD
FILM), was higher than 2,000 mGy in 63% of the patients. In spite of the possibility of the occurrence of erythema after exposure levels > 2,000 mGy, such reaction was not observed on the skin of any of the patients. The results obtained for both the localization of maximum dose, as well as for determining the maximum dose value have demonstrated the superiority and practicity in utilizing the radiochromic film.
The analysis of results obtained for the patients monitored with the radiochromic film allowed observing that K
a,r maximum, i.e., the K
a,r in the projection most utilized during the procedure and the maximum absorbed dose measured with the film, presented a significant correlation (r
2 = 0.808). Based on such relation (K
a,r maximum and MSD
FILM), it was possible to estimate the maximum absorbed dose for the other patients in the study (MSDK
a,r max). The individual results for maximum absorbed dose measured with the radiochromic films (MSD
FILM) and estimated from de relation with K
a,r maximum (MSDK
a,r max) are shown on Table 2.
The maximum absorbed dose on patients’ skin surface was higher than 1,000 mGy in 94% (32 out of 34) of the evaluated procedures, and higher than 3,000 mGy in 29% (10 out of 34).
The patients that presented maximum absorbed dose higher than 3,000 mGy or cumulative air kerma higher than 5,000 mGy were contacted and did not report the occurrence of lesions.
Radiation on physicians
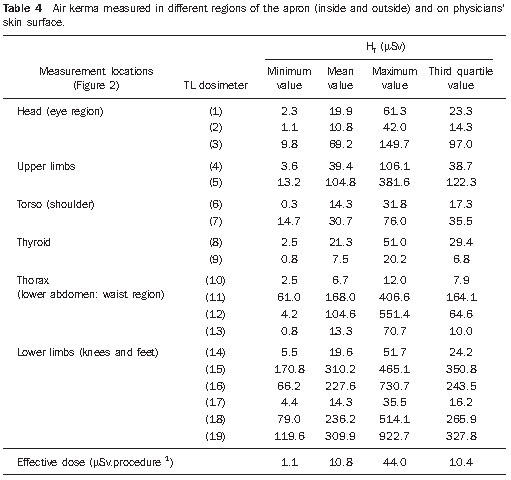
The mean effective dose per procedure on the physicians was 10.8 ìSv. The minimum, mean, maximum and third quartile values of the dose equivalents obtained by the TL dosimeters on the bodies of the physicians are shown on Table 4.
The mean values for the dose equivalents on the extremities, which were the highest ones, were the following: 923 ìSv on the left foot, 514 ìSv on the right foot, 382 ìSv on the left hand and 150 ìSv on the left eye. The reason for the highest doses being located on the left side of the physicians’ bodies and on the lower limbs is because the X-ray tube is located at the left side of the physician and underneath the surgical table, and also because of the absence of a lower lead curtain in the equipment.
DISCUSSION
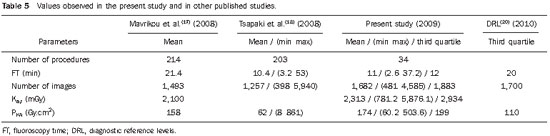
As regards dose parameters, the comparison of the results from the present study with those published in the literature (see Table 5) shows that the recorded values are comparable with those reported by Mavrikou et al.(17) and Tsapaki et al.(18) and with the diagnostic reference levels (DRL) suggested by the IAEA(19) (TF = 22 min, P
KA = 125 Gy.cm
2) and by the European DIMOND III project(20).
Based on the results obtained in the present study, where 94% of the patients presented maximum absorbed dose > 1,000 mGy and, considering that restenosis occurs in 40% of patients submitted to percutaneous coronary interventions within the first six months following the procedure( 21,22), it is recommended that the hemodynamics department of the hospital records the doses and perform the clinical follow-up of all patients submitted to angioplasty procedures (transluminal coronary angioplasty), to evaluate both the occurrence of immediate as well as late effects (cancer).
As regards dosimetry on physicians, the doses on the legs were very high and could be reduced by means of an accessory such as a lower lead curtain placed on the lower part of the table, according to recommendations on Ordinance 453 of the Brazilian Ministry of Health(23). The mean dose per procedure on the left eye of the physicians was 69 μSv. Such value could be significantly reduced in case the upper protective shield of the equipment or protection goggles were utilized. In general, physicians do not wear such goggles during the procedures either because they are not comfortable or because they are not available at the unit. However, several studies have demonstrated the occurrence of injuries to the crystalline lens of interventional physicians as a consequence of the scattered radiation received during such procedures( 24).
Considering the limit values for the dose equivalents established by both national and international standards (CNEN, ICRP), corresponding to 500 mSv/year for extremities and 150 mSv/year for the crystalline lens, it is estimated that such limits would be exceeded with 20 to 32 weekly transluminal coronary angioplasty procedures.
CONCLUSION
The results of the present study indicate the necessity of adopting strategies to optimize radiological protection both for patients and physicians. The first steps in that direction could be the adoption of measures to control the cumulative dose, clinical follow-up of patients, and utilization of protective accessories by physician (lower lead curtains and protection goggles, among others).
REFERENCES
1. Atik E. Cateterismo cardíaco intervencionista na cardiologia pediátrica. O posicionamento médico quanto às aplicações atuais e perspectivas. Arq Bras Cardiol. 2002;79:443–5.
2. United Nations Scientific Committee on the Effects of Atomic Radiation. Sources and effects of ionizing radiation. UNSCEAR 2000 Report to the General Assembly, with scientific annexes – annexes D and E. [acessado em 3 de março de 2008]. Disponível em: http://www.unscear.org/ docs/reports/annexd.pdf
3. Miller DL, Balter S, Wagner LK, et al. Quality improvement guidelines for recording patient radiation dose in the medical record. J Vasc Interv Radiol. 2004;15:423–9.
4. Miller DL, Balter S, Cole PE, et al. Radiation doses in interventional radiology procedures: the RAD-IR study. Part I: overall measures of dose. J Vasc Interv Radiol. 2003;14:711–27.
5. Stecker MS, Balter S, Towbin RB, et al. Guidelines for patient radiation dose management. J Vasc Interv Radiol. 2009;20(7 Suppl):S263–73.
6. International Electrotechnical Commission. IEC report 60601. Medical electrical equipment – Part 2-43: particular requirements for the safety of xray equipment for interventional procedures. Geneva, Switzerland: International Electrotechnical Commission; 2000.
7. International Commission on Radiological Protection. ICRP Publication 103: The 2007 Recommendations of the International Commission on Radiological Protection. Annals of the ICRP (v. 37/2-4). New York, NY: Elsevier; 2007.
8. International Commission on Radiological Protection. ICRP Publication 85. Avoidance of radiation injuries from medical interventional procedures. Ann ICRP 30(7-67). Oxford/New York: Pergamon Press; 2000.
9. Vano E. Radiation exposure to cardiologists: how it could be reduced. Heart. 2003;89:1123–4.
10. Filippova I. Patient and staff doses in radiology and cardiology in Estonia. Radiat Prot Dosimetry. 2005;117:59–61.
11. Philips Medical System. Integris Allura 12 & 15: technical handbook. Netherland: Philips Electronics N.V.; 2003.
12. Brasil. Ministério da Saúde. Conselho Nacional de Saúde. Diretrizes e normas regulamentadoras de psquisa envolvendo seres humanos. Resolução CNS nº 196, de 10 de outubro de 1996. [acessado em 15 de setembro de 2009]. Disponível em: http://conselho.saude.gov.br/resolucoes/1996/ Reso196.doc
13. International Specialty Products. GAFCHROMIC
® XR-RV2 dosimetry film. Characteristic performance data. [acessado em 10 de março de 2009]. Disponível em: http://online1.ispcorp.com/_layouts/ Gafchromic/
14. Silva MSR, Khoury HJ, Borrás C, et al. Calibração do filme radiocrômico GAFCHROMIC XRRV2 para radiologia. Rev Bras Fís Méd. 2010; 4:45–8.
15. Kim KP, Miller DL, Balter S, et al. Occupational radiation doses to operators performing cardiac catheterization procedures. Health Phys. 2008; 94:211–27.
16. International Commission on Radiological Protection. ICRP Publication 74: Conversion coefficients for use in radiological protection against external radiation. Annals of the ICRP (v. 37/2- 4). New York, NY: Pergamon; 1997.
17. Mavrikou I, Kottou S, Tsapaki V, et al. High patient doses in interventional cardiology due to physicians’ negligence: how can they be prevented? Radiat Prot Dosimetry. 2008;129:67–70.
18. Tsapaki V, Patsilinakos S, Voudris V, et al. Level of patient and operator dose in the largest cardiac centre in Greece. Radiat Prot Dosimetry. 2008; 129:71–3.
19. International Atomic Energy Agency. Establishing guidance levels in X ray guided medical interventional procedures: a pilot study. Safety Reports Series nº 59. Vienna: IAEA; 2009.
20. DIMOND website. Patient and staff dosimetry database/Interventional cardiology/Diagnostic reference levels for CA and PTCA. [acessado em 10 de janeiro de 2010]. Disponível em: http:// www.dimond3.org/WEB_DIMOND3/home.htm
21. Martinez EE, Ribeiro EE. Hemodinâmica e cardiologia intervencionista: abordagem clínica. Barueri, SP: Manole; 2008.
22. Unimed. Central de Serviços Auxiliares. Câmara Técnica de Medicina Baseada em Evidências. Avaliação das evidências comparativas entre os
stents coronarianos recobertos por drogas: Sirolimus (
Cypher®) x Paclitaxel (
Taxus®). [acessado em 10 de janeiro de 2010]. Disponível em: http:// www.unimedvtrp.com.br/autoriza/evidencias_ aprovadas/avaliacao_stent_coronariano– recoberto.pdf
23. Brasil. Ministério da Saúde. Secretaria de Vigilância Sanitária. Diretrizes de proteção radiológica em radiodiagnóstico médico e odontológico. Portaria/MS/SVS no 453, de 1º de junho de 1998. Brasília, DF: Diário Oficial da União, 2 de junho de 1998.
24. Lie ØØ, Paulsen GU, WØhni T. Assessment of effective dose and dose to the lens of eye for the interventional cardiologist. Radiat Prot Dosimetry. 2008;132:313–8.
1. Master in Biomedical Engineering, Professor at Instituto Federal de Ciências, Educação e Tecnologia de Pernambuco, Recife, PE, Brazil.
2. PhD of Physics, Titular Professor at Department of Nuclear Energy, Universidade Federal de Pernambuco (UFPE), Recife, PE, Brazil.
3. PhD of Sciences, Visiting Professor at Department of Nuclear Energy, Universidade Federal de Pernambuco (UFPE), Recife, PE, Brazil.
4. MD, Resident, Department of Surgery, Hospital das Clínicas de Pernambuco, Recife, PE, Brazil.
5. MD, Resident, Department of Surgery, Hospital da Aeronáutica de Pernambuco, Recife, PE, Brazil.
6. MDs, Interventional Cardiologists, Department of Hemodynamics, Instituto de Medicina Integral Professor Fernando Figueira (IMIP), Recife, PE, Brazil.
Mailing Address:
Maria do Socorro Rocha da Silva
Grupo GDOIN-DEN, Universidade Federal de Pernambuco
Avenida Professor Luiz Freire, 1000, Cidade Universitária
Recife, PE, Brazil, 50740-540
E-mail: msrochas2003@yahoo.com.br
Received June 1st, 2010.
Accepted after revision March 21, 2011.
Study developed at the Department of Nuclear Energy – Universidade Federal de Pernambuco (UFPE), Dosimetry and Nuclear Instrumentation Group, and Instituto de Medicina Integral Professor Fernando Figueira (IMIP), Recife, PE, Brazil.
 Vol. 44 nº 2 - Mar. / Apr. of 2011
Vol. 44 nº 2 - Mar. / Apr. of 2011