Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 44 nº 1 - Jan. /Feb. of 2011
Vol. 44 nº 1 - Jan. /Feb. of 2011
|
ORIGINAL ARTICLE
|
|
Hepatic vein Doppler flowmetry in patients with nonalcoholic steatosis |
|
|
Autho(rs): Valéria Ferreira de Almeida e Borges1; Angélica Lemos Debs Diniz2; Helma Pinchemel Cotrim3; Haroldo Luis Oliva Gomes Rocha4; Frederico Chaves Salomão5 |
|
|
Keywords: Fatty liver; Hepatic steatosis; Ultrasonography; Doppler flowmetry; Hepatic vein; Liver biopsy. |
|
|
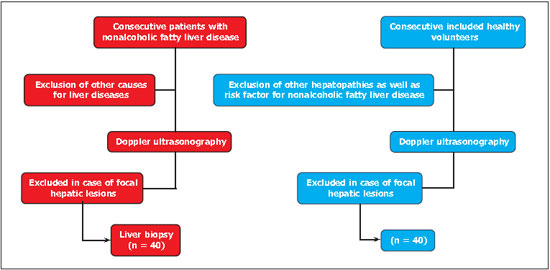
Abstract: INTRODUCTION
Steatosis is chemically defined as hepatic triglyceride content greater than 5% of the hepatic volume or of the liver weight(1) or, histologically, when 5% or more of the hepatocytes contain triglycerides(2). Ultrasonography is the imaging method most frequently indicated in the diagnosis and evaluation of hepatic steatosis, considering its noninvasiveness, wide availability and low cost(3–5). It has been described that the hepatic veins present a decrease in pulsatility in cases of fat infiltration, from the triphasic pulsatile pattern to a biphasic pattern and eventually to a monophasic flow where no oscillation in the flow velocity waveform is identified at pulsatile Doppler(6). The objective of this study was to evaluate flow velocity waveform patterns in the right hepatic vein of patients with different steatosis degrees in nonalcoholic fatty liver disease confirmed by biopsy, and comparing them with each other and with a control group. MATERIALS AND METHODS This is an observational study, in which the data were prospectively collected. It was developed in a single research center at Universidade Federal de Uberlândia (UFU), Uberlândia, MG, Brazil. The volunteers were consecutively included (Figure 1). The study was approved by the UFU Committee for Ethics in Research under number 065/08. Only those patients who signed a term of free and informed consent after verbal explanation were included in the present study. In the period between October/2008 and November/2009, 182 patients with nonalcoholic fatty liver disease were evaluated at the fatty liver unit of Hospital das Clínicas of UFU. Among those patients, 40 were included in the present study after clinical evaluation, laboratory tests, ultrasonography and histopathological evaluation of liver fragments obtained by biopsy, thus constituting the group of steatotic patients. Also, a group with 40 healthy volunteers without risk factors for nonalcoholic fatty liver disease, with minimal or no alcohol ingestion, neither diabetes nor obesity were included as a (nonsteatotic) control group. Such control group was submitted to the same evaluations as the patients with the disease, except for hepatic biopsy, for ethical reasons. All the volunteers in the steatotic group met the specific inclusion and exclusion criteria described below. The volunteers included in the control group met the same exclusion and inclusion criteria, except for the presence of hepatic steatosis at ultrasonography. Additionally, for the control group, any evidence of insulin resistance and risk factor for nonalcoholic fatty liver disease were exclusion criteria. Inclusion criteria were the following: presence of steatosis at US; age between 18 and 70 years, both sexes; written consent after verbal explanation. Exclusion criteria were: alcohol ingestion > 140 g/week for men and > 70 g/week for women(7); use of drugs known to be hepatotoxic, such as tetracycline, amiodarone, tamoxifen and alpha-methyldopa; presence of chronic viral hepatitis B or C; hemochromatosis; Wilson's disease; deficiency of alpha-1-antitrypsin; autoimmune hepatitis; other chronic liver diseases, portal hypertension, cirrhosis, ascites and liver failure; any form of coagulation disorder, no matter how slight it might be; presence of heart disease, acute coronary, cerebral or peripheral ischemia; presence of respiratory failure, kidney disease, ectopic or absent right kidney; focal hepatic lesions; focal renal lesions, which might interfere with the comparison between liver and kidney;pregnancy and lactation; refusal to participate in the study. Clinical evaluation Demographic data and the anthropometric measurements such as weight and height were obtained during outpatient consultations. The body mass index (BMI) was calculated by means of the Quetelet's formula: BMI = weight in kg/(height in m2). Waist circumference was measured in centimeters, by utilizing an inelastic tape, at the midpoint located between the last rib and the iliac crest, at the end of normal expiration. The circumference of the hip was measured at the level of the greatest gluteal protuberance. The waist/hip ratio was obtained by the division of waist circumference by the hip circumference. Laboratory tests The following tests were performed: complete blood count, plasma lipid profile, coagulation, total protein and fractions, aspartate aminotransferase, alanine aminotransferase, alkaline phosphatase, gamma-glutamyltransferase, total bilirubin and fractions, glucose, insulin, markers for hepatitis B and C, autoantibodies, serum copper and ceruloplasmin and iron profile. Evaluation of insulin resistance For the cases that did not met DM2 diagnostic criteria, and did not present glycemic risk for diabetes, the HOMA-IR (homeostasis model assessment for insulin resistance) index was calculated. For such purpose, material for insulin and glycemic tests was collected after fasting and the calculations were made according to the following formula: glycemia (mg/dl) × insulin (UI/ml) ÷ 405(8). Sonographic evaluation All the 80 patients were submitted to Doppler ultrasonography, with 2–5 MHz multifrequency transducer (Voluson 730 Pro V; General Electric, Milwaukee, WI, USA). The patients were examined under fasting conditions, between 8:00 and 10:00 a. m., in dorsal decubitus, with arms extended besides their head. All liver segments were scanned, and the presence of vascular malformations, cysts, focal parenchymal lesions was ruled out. The color Doppler mode was utilized for identification of the hepatic veins, and to evaluate their pulsatility pattern and flow direction. The evaluation of the right hepatic vein was standardized at the level of the 10th or 11th right intercostal space during a short breath-hold period, at a distance of 2.0 cm distal to the hepatic veins confluence, to avoid artifacts in the waveform pattern. The analysis was recorded for at least four cardiac cycles (approximately 6 seconds). The transducer angle was 30°. The waveform patterns were classified into three groups: normal triphasic waveform with a short reversed flow, biphasic waveform without reversed flow but fluttering of more than 10% of the mean phasic amplitude, and monophasic flat waveform with fluttering of < 10% of the mean phasic amplitude (Figure 2). Because of alterations in the vessel diameter, of up to 2 mm per cardiac cycle at systole and diastole, besides different flow directions, velocimetry in the hepatic veins was not calculated. 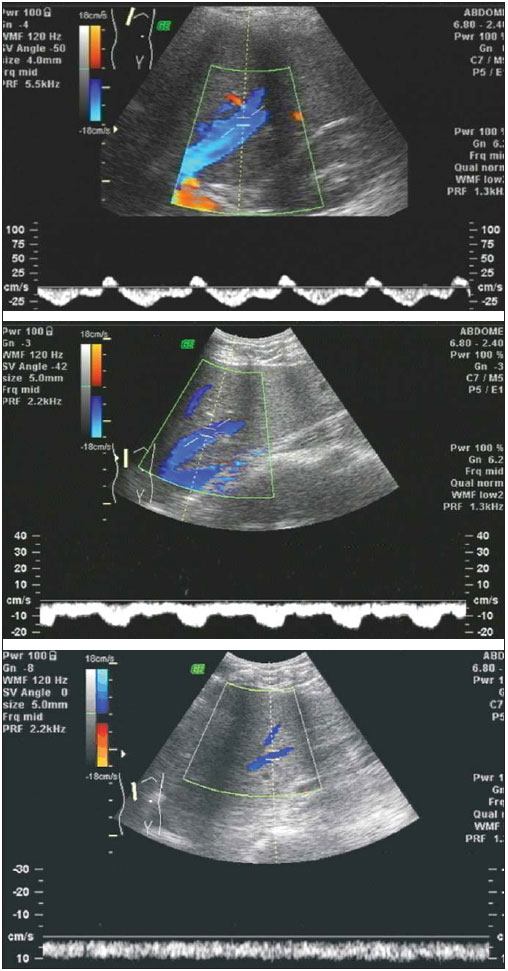 Figure 2. Hepatic vein flow pattern at Doppler. On the upper image, triphasic pattern; on the central image, biphasic pattern; on the lower image, monophasic pattern. Histological evaluation Hepatic biopsy specimens were collected under US guidance by means of Trucut needle, at the right hepatic lobe. The hepatic tissue fragment with approximately 10 mm was fixed in 4% formol-saline and stained with hematoxylin-eosin and Masson's trichrome techniques according to the method adopted at the division of Pathological Anatomy of Hospital das Clínicas of UFU. A single observer, an experienced pathologist, performed a blind evaluation of the material. The biopsy was performed one week after the ultrasonography. The histopathological evaluation was based on the reviewed standardized classification of the Pathology Committee of the NASH Clinical Research Network(2), which designated and validated the histologic characteristics and a score system for nonalcoholic fatty liver disease activity, for the purposes of clinical studies. The histopathological variables were described and subdivided into hepatocellular changes, fibrosis and inflammatory infiltrate. The hepatocellular changes that were systematically searched were the following: steatosis, hepatocellular ballooning and Mallory bodies. Steatosis was classified as mild (up to 33% of hepatocytes infiltrated by fat droplets), moderate (from 33% to 66%) and severe (more than 66% of fatty infiltration in the hepatocytes). The inflammatory infiltrate intensity was classified into mild, moderate and accentuated. Fibrosis was described according to location in the hepatic acinus, appearance and intensity. Statistical analysis The statistical analysis was performed with the aid of the software Statistical Package for the Social Sciences (SPSS for Windows, version 16.0) (SPSS Inc.; Chicago, IL, USA). The Lilliefors normality test was utilized in the analysis of the data distribution. The continuous variables were expressed as mean ± standard deviation, median and quartiles, as appropriate, and compared by means of the analysis of variance between means (ANOVA) and Tukey's range test for post-hoc analysis. The categorical variables were expressed by absolute (n) and relative frequencies, and were analyzed by means of the Fisher's and Mann-Whitney's tests. The correlation analyses were performed by utilizing the Spearman coefficient. All significance tests were bilateral, adopting a significance level of 0.05 (α = 5%), with descriptive levels (p) lower than this value being considered as statistically significant. RESULTS Clinical characterization of patients and controls The clinical characteristics of steatotic patients as compared with controls are shown on Table 1. 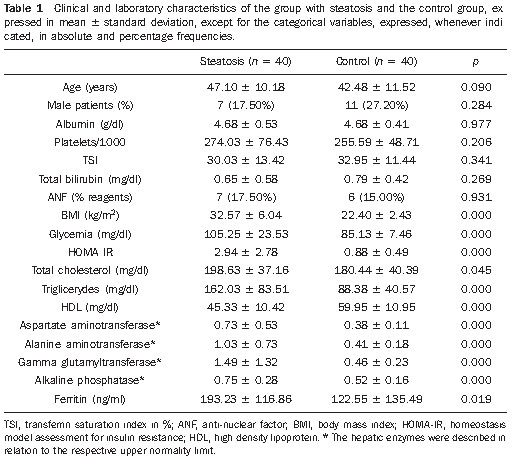 The groups were paired with respect to age and sex. The ages of volunteers in the control group ranged from 27 to 70 years, with a mean age of 42.48 ± 11.52 years. The mean age of the steatotic patients was 47.10 ± 10.18 years. By utilizing the variance analysis (ANOVA for one variable) no significant difference was found between mean ages (p = 0.061). The control group comprised 11 men and 29 women, while the steatotic group comprised seven men and 33 women. By utilizing the Fisher's test, no statistically significant difference was observed between these ratios (p = 0.284). No statistically significant difference was found between the groups with respect to the albumin serum level, bilirubin, platelet count and transferrin saturation index. The patients with nonalcoholic fatty liver disease presented altered obesity, dyslipidemia, insulin resistance, hepatic enzymes indices and ferritin levels as compared with the control group. Histological evaluation The histological evaluation was only performed in the group of diseased patients, confirming the presence of steatosis in all of them. Among those patients, 16 presented mild steatosis, i.e., with up to 33% of affected hepatocytes; 19 presented moderate steatosis (33% to 66% of affected hepatocytes); and five presented severe steatosis, with more than 66% of the hepatocytes infiltrated by fat droplets. At biopsy, none of the patients presented advanced fibrosis producing nodulations (cirrhosis). Thirty of the patients presented some degree of fibrosis, and in nine of them (22.5%) bridging fibrosis was described. Sonographic evaluation Differences were observed in the hepatic vein flow velocity waveform pattern at Doppler between the steatotic and the control groups. In the control group, the predominant waveform pattern was triphasic, while in the group with the disease the pattern was either biphasic or monophasic. At Doppler, 22 of 40 steatotic patients (55%) presented abnormal hepatic vein pattern, with 16 (40%) with monophasic pattern and six (15%) with biphasic pattern. At Mann-Whitney test, the difference in the frequency of the abnormal hepatic vein flow velocity waveform pattern between the two groups was statistically significant (p < 0.0001). A reversed and statistically significant correlation between the fatty infiltration degree and the hepatic vein flow velocity waveform pattern was observed (r = –0.57 ± 0.08; p < 0.01). The difference in the frequency of the abnormal hepatic vein flow velocity waveform pattern among the subgroups of steatotic patients was not statistically significant (p = 0.33). Table 2 demonstrates the distribution of flow velocity waveform patterns according to the degree of steatosis detected at histology. 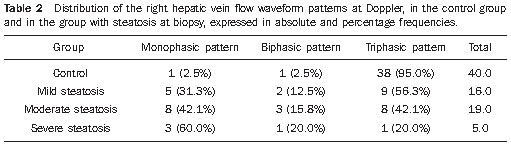 DISCUSSION Nonalcoholic fatty liver disease is a common cause of chronic hepatopathy in insulin-resistant individuals(9). The disease presentations range from steatosis, with possible progression to steatohepatitis, fibrosis, cirrhosis and hepatocellular carcinoma(10). At ultrasonography, the most frequent presentation is the finding with an appearance suggestive of steatosis(11). In the present study, a control group of individuals with no risk factor risk for nonalcoholic fatty liver disease was utilized for comparison. Such group was confirmed to be comprised of healthy individuals, without any sign characterizing insulin resistance, which clearly differentiated it from the group of patients with the disease. The mean HOMA-IR index for the healthy volunteers was quite low (0.88) and the cutoff point between the control group and the group with the disease (> 1.35) was lower than the ones reported in other Brazilian studies(10,11). In the present sample, the mean values for hepatic enzymes in relation to the upper normal limit demonstrated to be compatible with very subtle increases, with normal aminotranferases levels in most of the cases, as already described in the literature. On the other hand, at histology, all the patients submitted to biopsy met some criteria for nonalcoholic steatohepatitis, confirming, as previously known, that hepatic enzymes are falsely normal in the majority of such patients(12,13). In the setting of portal hypertension, the clinical value of Doppler in the hepatic and portal veins hemodynamics is well established. On the other hand, the contribution of steatosis, inflammation and fibrosis in the setting of nonalcoholic fatty liver disease, to change the hepatic and portal veins flow velocity waveform is the focus of more recent interest. In the present study, Doppler ultrasonography and hepatic biopsy were prospectively performed in a same week, in a group of volunteers with diffuse and homogeneous steatosis caused by nonalcoholic fatty liver disease, with the objective of reducing eventual biases. Other conditions that might interfere with Doppler, such as pregnancy, cardiac failure, valvulopathies and chronic pulmonary disease, were ruled out. Dietrich et al.(14), in a study published in 1998, demonstrated that the relationship between the left hepatic lobe and the heart, often leads to artifacts in the Doppler signal, particularly because of heart motion. For this reason, the evaluation of the left hepatic vein, particularly, is not always reliable. In 35 of 135 patients the evaluation of the middle hepatic vein was only possible during deep inspiration, with respiration artifacts initially producing a monophasic flow velocity waveform, then changing to biphasic and triphasic during the examination. The most reproducible evaluation of the flow velocity waveform was obtained on the right hepatic vein through the intercostal pathway, at a 30º angle, as performed in the present study. Other studies approaching hepatic vein flow velocity waveform also have not found its capacity to differentiate groups with the disease (Table 3), finding frequencies similar to those observed in the present study regarding the pathological hepatic vein pattern in patients with the disease and in the controls(6,14,15). 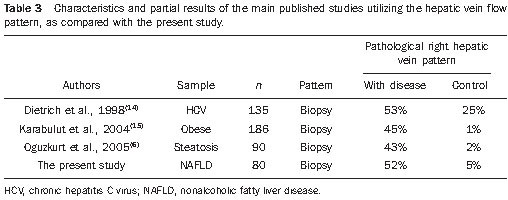 CONCLUSION The triphasic hepatic vein flow velocity waveform pattern was more frequent in the controls as compared with the diseased patients. However, no statistically significant difference was observed between the right hepatic vein flow velocity waveform patterns in the three steatotic sub-groups. REFERENCES 1. Hoyumpa AM Jr, Greene HL, Dunn GD, et al. Fatty liver: biochemical and clinical considerations. Am J Dig Dis. 1975;20:1142–70. 2. Kleiner DE, Brunt EM, Van Natta M, et al. Design and validation of a histological scoring system for nonalcoholic fatty liver disease. Hepatology. 2005;41:1313–21. 3. Saadeh S, Younossi ZM, Remer EM, et al. The utility of radiological imaging in nonalcoholic fatty liver disease. Gastroenterology. 2002;123:745–50. 4. Hamaguchi M, Kojima T, Itoh Y, et al. The severity of ultrasonographic findings in nonalcoholic fatty liver disease reflects the metabolic syndrome and visceral fat accumulation. Am J Gastroenterol. 2007;102:2708–15. 5. Charatcharoenwitthaya P, Lindor KD. Role of radiologic modalities in the management of non-alcoholic steatohepatitis. Clin Liver Dis. 2007;11:37–54, viii. 6. Oguzkurt L, Yildirim T, Torun D, et al. Hepatic vein Doppler waveform in patients with diffuse fatty infiltration of the liver. Eur J Radiol. 2005;54:253–7. 7. Farrell GC, George J, Hall PM, et al. Fatty liver disease: NASH and related disorders. Oxford, UK: Blackwell Publishing; 2005. 8. Turner RC, Holman RR, Matthews D, et al. Insulin deficiency and insulin resistance interaction in diabetes: estimation of their relative contribution by feedback analysis from basal plasma insulin and glucose concentrations. Metabolism. 1979;28:1086–96. 9. Cusi K. Role of insulin resistance and lipotoxicity in non-alcoholic steatohepatitis. Clin Liver Dis. 2009;13:545–63. 10. Guidorizzi de Siqueira AC, Cotrim HP, Rocha R, et al. Non-alcoholic fatty liver disease and insulin resistance: importance of risk factors and histological spectrum. Eur J Gastroenterol Hepatol. 2005;17:837–41. 11. Geloneze B, Vasques AC, Stabe CF, et al. HOMA1-IR and HOMA2-IR indexes in identifying insulin resistance and metabolic syndrome: Brazilian Metabolic Syndrome Study (BRAMS). Arq Bras Endocrinol Metabol. 2009;53:281–7. 12. Browning JD, Szczepaniak LS, Dobbins R, et al. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004;40:1387–95. 13. Suzuki A, Lymp J, Sauver JS, et al. Values and limitations of serum aminotransferases in clinical trials of nonalcoholic steatohepatitis. Liver Int. 2006;26:1209–16. 14. Dietrich CF, Lee JH, Gottschalk R, et al. Hepatic and portal vein flow pattern in correlation with intrahepatic fat deposition and liver histology in patients with chronic hepatitis C. AJR Am J Roentgenol. 1998;171:437–43. 15. Karabulut N, Kazil S, Yagci B, et al. Doppler waveform of the hepatic veins in an obese population. Eur Radiol. 2004;14:2268–72. 1. Master, MD, Unit of Gastroenterology at Universidade Federal de Uberlândia (UFU), Uberlândia, MG, Brazil. 2. PhD, Associate Professor, School of Medicine and Program of Post-graduation in Health Sciences, Universidade Federal de Uberlândia (UFU), Uberlândia, MG, Brazil. 3. Post-doctorate, Associate Professor, School of Medicine of Bahia, Coordinator for the Program of Post-graduation in Medicine and Health, Universidade Federal da Bahia (UFBA), Salvador, BA, Brazil. 4. Fellow Master degree, MD, Unit of Gastroenterology, Universidade Federal de Uberlândia (UFU), Uberlândia, MG, Brazil. 5. Professor of Pathology at Faculdade Atenas, Paracatu, MG, Brazil. Mailing Address: Dra. Angélica Lemos Debs Diniz Avenida Getúlio Vargas, 909, Centro Uberlândia, MG, Brazil, 38400-299 E-mail: angelica@cdeclinica.com.br Received October 13, 2010 Accepted after revision December 8, 2010. * Study developed at Universidade Federal de Uberlândia (UFU), Uberlândia, MG, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554