Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 6 - Nov. / Dec. of 2010
Vol. 43 nº 6 - Nov. / Dec. of 2010
|
ORIGINAL ARTICLE
|
|
Multidetector-row computed tomography angiography for the diagnosis of anomalous pulmonary venous drainage: an initial experiment* |
|
|
Autho(rs): Letícia Yurie Kimura1; Gustavo Spadaccia dos Santos Fernandes1; Karina Tavares de Melo Nobrega1; Luiz Augusto Gadia Gabure1; César Augusto Mastrofrancisco Cattani2; José Pedro da Silva3; Beatriz Helena Sanches Furlanetto4 |
|
|
Keywords: Anomalous drainage; Pulmonary veins, Congenital abnormalities; Multidetector-row computed tomography. |
|
|
Abstract: INTRODUCTION
Anomalous pulmonary venous drainage (APVD) is a rare heart defect of unknown etiology that manifests as a development failure in the pulmonary veins. It represents less than 1% of all congenital heart defects. APVD is defined as the drainage of one or more pulmonary veins from the left atrium, with direct or indirect pulmonary venous return into the right atrium(1–4). APVD is classified as either total APVD, in which all four pulmonary veins drain out of the left atrium, or partial APVD, in which one to three pulmonary veins drain either into a systemic vein or into the right atrium. The anomalous pulmonary venous connection in the systemic venous circuit has been known in its partial form since 1739, and in its total form, since 1798. However, variations in pulmonary venous connection are rarely observed, occurring in 0.4% of autopsy specimens(5). In the general population, total APVD is a rare condition, but it is frequently found in patients at institutions that specialize in congenital heart defects(4–7). According to Darling, Rothney and Craig, total APVD is anatomically classified into four types. In the supracardiac type, drainage is through a vertical vein, generally into the left innominate vein. This is the most frequent type, accounting for 40% to 50% of cases. In the cardiac type, drainage is directly into the right atrium or into the coronary sinus (20%). In the infracardiac type, drainage is through a vertical vein into the portal vein or into the inferior vena cava. This occurs in 10%-20% of cases. The mixed type represents about 10% of cases and is a combination of two or more of the above mentioned types. Association with atrial septal defect is always observed in all types of total APVD, since the absence of this defect with total APVD is incompatible with survival(4,6,7). Until recently, APVD diagnosis was made using echocardiography and conventional angiography. The main disadvantages of echocardiography are operator dependency, dependence on the patient’s acoustic window, and difficulty in evaluating extracardiac structures, particularly pulmonary venous drainage into the left atrium because of posterior positioning. The presence of a real communication between the pulmonary veins and the left atrium is often in doubt. The main disadvantages of conventional angiography is its invasiveness and higher risks for complications. This study aimed to determine if multidetector-row computed tomography angiography (MCTA) is an effective, non-invasive method for the diagnosis of APVD. MATERIALS AND METHODS All cardiac MCTA studies were performed with a 16-row Aquilion (Toshiba Medical Systems; Tokyo, Japan) or a 64-row Light Speed VCT (GE Healthcare; Milwaukee, WI, USA), from July 2003 to November 2007 were retrospectively reviewed, and a database was constructed. Our database showed 2905 cardiac MCTA studies performed from July 2003 to November 2007. These were divided according to their original objective into 393 studies intended to evaluate congenital cardiopathies, and 2512 intended to evaluate coronary arteries. Almost all studies that evaluated congenital cardiopathies were performed under anesthesia, except for those where the patient could cooperate with apnea. Studies performed under anesthesia required prior fasting for 6 hours for patients solely fed by breastfeeding, or 8 hours for patients on other diets. For patients who did not require anesthesia, a 4-hour fast was requested. All studies were retrospectively synchronized to electrocardiograms with two acquisitions, one arterial phase, and one venous phase, with an iodinated contrast (Optiray 320, Mallinckrodt; St. Louis, MO, USA) injection at a dose of 2 ml/kg, followed by a dose of 2 ml/kg of 0.9% saline solution, both in bolus. Beta-blocker drugs were not required in cases of suspected congenital cardiopathy. In children weighing < 10 kg, peripheral venous access was obtained with a Jelco 24 or 22 catheter with the entire contrast medium volume manually injected with a 10 ml syringe, followed by saline solution. The first-phase acquisition was initiated when half the contrast medium volume was injected, followed by the second-phase acquisition with no waiting period, always under apnea supported by the anesthetist. In patients weighting > 10 kg, an injection pump was used, with peripheral injection at 2 ml/s into a Jelco 22 catheter, with the first scan initiated as half the volume of contrast medium was injected, also under apnea. For adult patients who could cooperate with inspiratory apnea, an injection pump with 4 ml/s injection was used to achieve a total dose of 1.2 ml/kg of contrast medium injected through peripheral venous access with a Jelco 20 or 18 catheter, followed by 40 ml of saline solution injected at the same rate, monitoring contrast uptake in the left atrium, with the two scans initiated with a six-second respiratory interval. All MCTA reports on congenital cardiopathies were evaluated, and all cases of APVD were recorded. Reports were prepared by professionals with four-, two- and one-year of experience in MCTA, and all diagnoses were surgically confirmed and had clinical follow-up to monitor patient survival. RESULTS Of the 393 MCTA studies that evaluated congenital cardiopathies, 21 cases of APVD were observed, with 7 (33.3%) cases of total APVD, and 14 (66.7%) of partial APVD. No cases of APVD were found in the cardiac studies performed to evaluate coronary arteries. Fifteen patients were men (71%) and six were women (29%), with ages ranging from 7 days to 35 years (mean 3.3 years, standard deviation 8.9 years). Anomalous pulmonary venous drainage was found in only two adult patients (24 and 35 years). Of the total APVD cases, three were supracardiac, three infracardiac, and one cardiac. All are in Table 1 with cases of partial APVD. 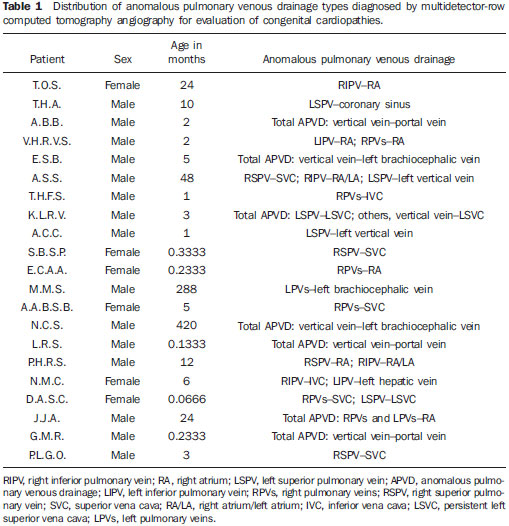 Supracardiac-type total APVD was seen in two cases in which four pulmonary veins drained into a vertical vein that drained into the left brachiocephalic vein. In another case, the left superior pulmonary vein drained directly into the left persistent superior vena cava, while the other pulmonary veins drained into a collector tube which also drained into the left persistent superior vena cava. Infracardiac-type total APVD was found in patients in whom four pulmonary veins drained into a vertical vein that drained into the portal vein. Cardiac-type APVD was characterized by four pulmonary veins draining directly into the right atrium. Among partial APVD cases, seven involved only the right side (50%), three involved only the left side (21.4%), and four cases presented with abnormality on both sides (28.6%). The partial APVD cases presented with a high variation in drainage types (Table 1). Nine deaths (42.8%) were recorded, eight (88.9%) in the first six months of life. The other death occurred in a two-year-old child. Of the patients who progressed to death, three had total APVD (33.3%), and the other had partial APVD. Figures 1 to 5 demonstrate the main types of APVD found at the authors’ institution. 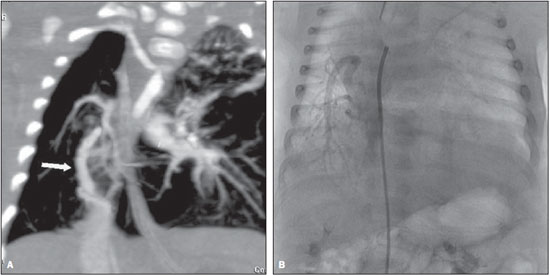 Figure 1. Multiplanar reconstruction of MCTA (A) A male, one-month-old patient, demonstrating partial anomalous pulmonary venous drainage with right pulmonary veins draining into the inferior vena cava in the shape of a curved “Turkish sword” (scimitar), confirmed by conventional angiography (B). 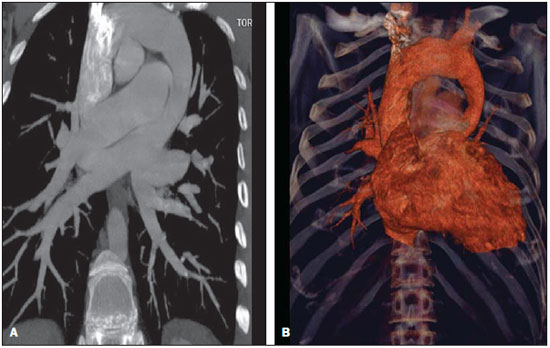 Figure 2. Multiplanar (A) and three-dimensional (3D) (B) reconstruction of MCTA in a male, 35-year-old patient submitted to examination because of suspicion of a mediastinal tumor, demonstrating a total anomalous pulmonary venous connection represented by all the four veins draining into the vertical vein that drains into the left brachiocephalic vein, towards the superior vena cava. 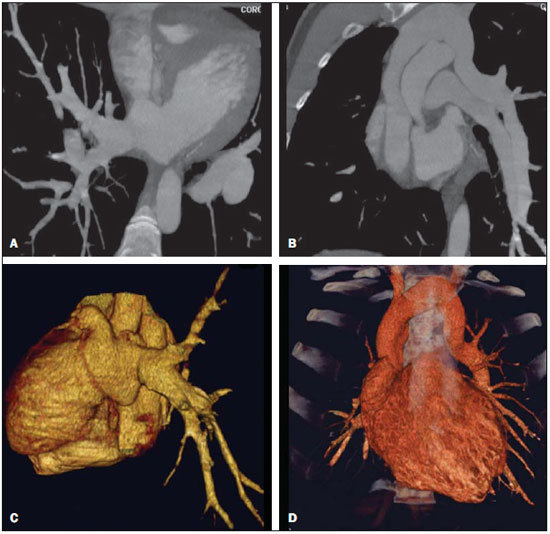 Figure 3. Multiplanar (A,B) and 3D (C,D) reformation of MCTA in a male, 24-year-old patient with partial anomalous pulmonary venous drainage in which the right pulmonary veins drain into the left atrium and the left pulmonary veins drain into the vertical vein towards the left brachiocephalic vein. 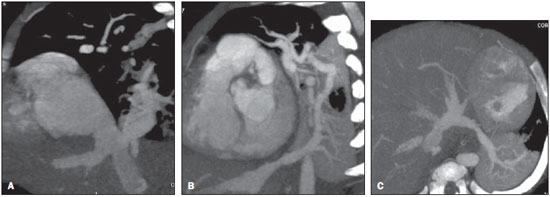 Figure 4. Multiplanar reconstruction of MCTA in a female, 6-month-old patient with partial anomalous pulmonary venous drainage, demonstrating that the right inferior pulmonary vein drains into the inferior vena cava (A) and the left inferior pulmonary vein drains into the left hepatic vein (B,C). 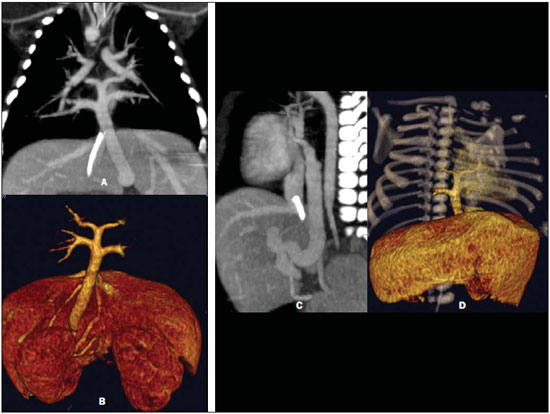 Figure 5. Multiplanar (A,C) and 3D (B,D) reformatation of the MCTA in a male, 7-day-old patient, demonstrating total anomalous pulmonary venous drainage, with all pulmonary veins draining into a vertical vein that drains into the portal vein. DISCUSSION Although APVD is a rare congenital cardiac anomaly, with a prevalence of <1% reported in the literature, we observed a prevalence of 5.34%, probably because the study was conducted at a center of reference for congenital cardiopathies. In agreement with other studies, we found the prevalence of APVD to be higher at specialized institutions(1–6). Most patients with partial APVD are asymptomatic, and the condition is incidentally diagnosed after chest radiography or computed tomography(5,7–10). The method of choice for diagnosis is transthoracic echocardiography or by conventional angiography, but these have some disadvantages. These include operator dependency, dependence on the patient’s acoustic window, and difficulty in evaluating extracardiac structures, particularly the pulmonary venous drainage with its posterior positioning. Another disadvantage is invasiveness, with higher risks for death, especially in patients with obstructed APVD(10–12). Magnetic resonance imaging has also been used to diagnose APVD(10,13–15), but has not been adopted at the authors’ institution because of the difficulty in monitoring in the examination room. This method also has lower spatial resolution for patients weighing less than 10 kg. Computed tomography angiography is a valuable method for evaluating several vascular alterations in adults, particularly in cases of aortic conditions such as aneurysms and dissections(16–18). The main disadvantages of this method are the necessity for apnea, requiring general anesthesia of pediatric patients, and the use of iodinated contrast media and ionizing radiation, which is similar to conventional angiography. In 2000, Kim et al. reported the application of helical computed tomography angiography in neonates and children with total APVD, which had not been studied before. However, those examinations were performed without apnea(12). We found no studies that used MCTA for diagnosing APVD, and only one study using magnetic resonance imaging. Other studies used magnetic resonance imaging to evaluate congenital abnormalities in general(10,13–15). In this study, the majority of cases were partial APVD, which is consistent with reports in the literature, and the consideration that most patients with total APVD die in their first years of life. The patients in our study were not asymptomatic, and multidetector-row CT angiography had been requested with a precise indication for preoperative evaluation, since most patients presented with the disease in association with severe congenital cardiopathy(5,7–9,10). Patients with total APVD rarely survive to adulthood, and this abnormality almost always requires emergency neonatal surgery, as soon as the diagnosis is made, to avoid irreversible pathological alterations in the pulmonary vascular bed. In adulthood, patients may present with fatigue or dyspnea with stress because of the blood volume overload produced by the left-to-right shunt(5,7–10,19–23). The two adult patients were found in this study to be asymptomatic. One had total APVD and the other had partial APVD. The latter underwent tomography because of suspicion of a mediastinal tumor from enlargement of the mediastinum observed on a chest radiograph. In cases of partial APVD, the right side is usually more involved than the left side with a ratio of 2:1 to 10:1. In cases of left-side APVD, the pulmonary veins generally demonstrate venous return to a vertical vein that drains into the left brachiocephalic vein, with the typical “snowman” sign on radiography and/or computed tomography(8–10). Our data corroborate the previous findings. Seven (50%) of the partial APVD patients presented with involvement of only the right side, and four demonstrated partial APVD in both sides (28.6%). Only three (21.4%) presented with partial APVD isolatedly involving the left side. Partial APVD may lead to hemodynamic changes such as blood volume overload in the left ventricle and pulmonary circulation, resulting in congestive heart failure. Additionally, systemic and pulmonary venous blood mixing occurs in the right atrium, leading to arterial desaturation(5,7,8,19–23). Total APVD is incompatible with life in the absence of a coexisting interatrial communication that allows the passage of oxygenated blood into the left heart chambers. More than 75% of children with total APVD die in the first year of life (7,8,19–23). In this study, nine patients died, eight in the first months of life (88.89%), consistent with reports in the literature. Of the patients who died, three presented with total APVD (33.33%). The first successful surgery for repair of total APVD was performed in 1951. Since then, surgical mortality rates have decreased, but remain high, particularly in patients younger than three years of age who have severe pulmonary hypertension or pulmonary venous obstruction that determines preoperative hemodynamic instability(5,7). Early diagnosis of APVD and its immediate repair are of paramount importance for the prognosis of these children, considering that clinical and hemodynamic deterioration worsens the surgical outcomes in these patients(5). Of the total APVD cases in this series, four occurred in patients who were younger than five months of age, one was in a four-month-old patient, and another was in a 35-year-old patient. The latter represents a rare case report in the literature. Surgical treatment consists of the reinsertion of the four pulmonary veins into the left atrium, and is indicated as soon as the diagnosis is made, to prevent hemodynamic changes and lesions on the pulmonary vascular bed, which generally occur in the first years of life(1–7,9,11,12,19–23). Occlusion of a catheterized or central vein is a frequent complication, occurring in approximately 23% of patients submitted to central venous access procedures. Symptomatic occlusion occurs in 1% to 4% of cases, presenting with sudoresis, pain, and superior vena cava syndrome that can be managed with a combination of thrombolysis angioplasty and stent implantations(8–10). As previously described, this study neither analyzed postoperative complications nor causes of death. This topic deserves further investigation in future studies. In spite of requiring anesthesia, the use of iodinated contrast medium and ionizing radiation with MCTA is useful for diagnosing APVD because of its non-invasiveness, and the ability to evaluate intra- and extra-cardiac structures. This allows a thorough study of the thoracic anatomy and makes a positive contribution to the surgery, and improves patient prognosis. In particular, it allows the diagnosis of clinically unsuspected malformations. The main limitation of this study was the absence of a comparison with other diagnostic methods such as echocardiography and conventional angiography. We also did not address postoperative complications or causes of death in APVD patients. The absence of patient follow-up could be addressed in future investigations. CONCLUSION In spite of being rare, anomalous pulmonary venous drainage can be lethal unless it is diagnosed early. MCTA is a highly accurate and non-invasive method for diagnosing this condition. As an alternative to other, more invasive diagnostic methods, it can reduce costs and the morbimortality of APVD patients. Acknowledgements We thank Valdomiro Ferreira França for the support in the editing and finishing of the images. REFERENCES 1. Geva T, Van Praagh S. Anomalies of the pulmonary veins. In: Allen H, Gutgesell Clark E, Driscoll D, editors. Moss and Adams’ heart disease in infants, children, and adolescent. Philadelphia, PA: Lippincott Williams & Wilkins; 2001. p. 736–72. 2. Lupinetti FM, Kulik TJ, Beekman RH 3rd, et al. Correction of total anomalous pulmonary venous connection in infancy. J Thorac Cardiovasc Surg. 1993;106:880–5. 3. Reitz BA, Yuh DD. Cyanotic defects. In: Reitz BA, Yuh DD, editors. Congenital cardiac surgery. New York, NY: McGraw-Hill; 2002. p. 148–52. 4. Miller SW. Congenital heart disease. In: Miller SW, editor. Cardiac imaging: the requisites. Philadelphia, PA: Elsevier Mosby; 2005. p. 316–23. 5. Albert D, Girona J, Bonjoch C, et al. Retorno venoso pulmonar total anómalo en pediatría: importancia del diagnóstico ecocardiográfico y de la cirugía precoz. Rev Esp Cardiol. 2000;53:810–4. 6. Raisher BD, Grant JW, Martin TC, et al. Complete repair of total anomalous pulmonary venous connection in infancy. J Thorac Cardiovasc Surg. 1992;104:443–8. 7. Behrendt DM, Aberdeen E, Waterson DJ, et al. Total anomalous pulmonary venous drainage in infants. I. Clinical and hemodynamic findings, methods, and results of operation in 37 cases. Circulation. 1972;46:347–56. 8. Levy JM, Smyth SH. Partial anomalous pulmonary venous return: iatrogenic occlusion of the innominate vein producing right-to-left shunt. J Vasc Interv Radiol. 2002;13:423–5. 9. Cooley DA, Collins HA. Anomalous drainage of entire pulmonary venous system into left innominate vein: clinical and surgical considerations. Circulation. 1959;19:486–95. 10. Masui T, Seelos KC, Kersting-Sommerhoff BA, et al. Abnormalities of the pulmonary veins: evaluation with MR imaging and comparison with cardiac angiography and echocardiography. Radiology. 1991;181:645–9. 11. Vicente WVA, Dias-da-Silva PS, Vicente LM, et al. Correção cirúrgica de drenagem venosa pulmonar anômala total em adulto. Arq Bras Cardiol. 2006;87:e172–5. 12. Kim TH, Kim YM, Suh CH, et al. Helical CT angiography and three-dimensional reconstruction of total anomalous pulmonary venous connections in neonates and infants. AJR Am J Roentgenol. 2000;175:1381–6. 13. Didier D, Higgins CB, Fisher MR, et al. Congenital heart disease: gated MR imaging in 72 patients. Radiology. 1986;158:227–35. 14. Choe YH, Lee HJ, Kim HS, et al. MRI of total anomalous pulmonary venous connections. J Comput Assist Tomogr. 1994;18:243–9. 15. White CS, Baffa JM, Haney PJ, et al. MR imaging of congenital anomalies of the thoracic veins. Radiographics. 1997;17:595–608. 16. Chung JW, Park JH, Im JG, et al. Spiral CT angiography of the thoracic aorta. Radiographics. 1996;16:811–24. 17. Murayama S, Hashiguchi N, Murakami J, et al. Helical CT imaging of bronchial arteries with curved reformation technique in comparison with selective bronchial arteriography: preliminary report. J Comput Assist Tomogr. 1996;20:749–55. 18. Kopecky KK, Gokhale HS, Hawes DR. Spiral CT angiography of the aorta. Semin Ultrasound CT MR. 1996;17:304–15. 19. Atik FA, Irun PE, Barbero-Marcial M, et al. [Total anomalous drainage of the pulmonary veins – surgical therapy for the infradiaphragmatic and mixed anatomical types]. Arq Bras Cardiol. 2004; 82:259–63. 20. Serraf A, Belli E, Roux D, et al. Modified superior approach for repair of supracardiac and mixed total anomalous pulmonary venous drainage. Ann Thorac Surg. 1998;65:1391–3. 21. Cope JT, Banks D, McDaniel NL, et al. Is vertical vein ligation necessary in repair of total anomalous pulmonary venous connection? Ann Thorac Surg. 1997;64:23–9. 22. Shah MJ, Shah S, Shankargowda S, et al. L–R shunt: a serious consequence of TAPVC repair without ligation of vertical vein. Ann Thorac Surg. 2000;70:971–3. 23. Girard C, Neidecker J, Laroux MC, et al. Inhaled nitric oxide in pulmonary hypertension after total repair of total anomalous pulmonary venous return. J Thorac Cardiovasc Surg. 1993;106:369. 1. MDs, Unit of Cardiac Radiology of Med Imagem, Real e Benemérita Associação Portuguesa de Beneficência de São Paulo, São Paulo, SP, Brazil. 2. PhD, MD, Unit of Cardiac Radiology of Med Imagem, Real e Benemérita Associação Portuguesa de Beneficência de São Paulo, São Paulo, SP, Brazil. 3. Surgeon-in-Chief, Unit of Cardiac Surgery, Real e Benemérita Associação Portuguesa de Beneficência de São Paulo, São Paulo, SP, Brazil. 4. Physician Assistant at Unit of Cardiac Surgery, Real e Benemérita Associação Portuguesa de Beneficência de São Paulo, São Paulo, SP, Brazil. Mailing address: Dra. Letícia Yurie Kimura Rua Maestro Cardim, 476, ap. 83, Bela Vista São Paulo, SP, 01323-000, Brazil E-mail: lyk78@terra.com.br Received February 10, 2010. Accepted after revision May 12, 2010. * Study developed at the Unit of Cardiac Radiology of Med Imagem, Real e Benemérita Associação Portuguesa de Beneficência de São Paulo, São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554