Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 6 - Nov. / Dec. of 2010
Vol. 43 nº 6 - Nov. / Dec. of 2010
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Pedro José de Santana Júnior1; Kim-Ir-Sen Santos Teixeira2; Pedro Paulo Teixeira e Silva Torres3; Ana Caroline Vieira Aurione4; Diogo Neves Jacó1; Glauco Santana Batista1 |
|
|
Male, 41-year-old, ventilation-dependent patient coming from Goiânia, GO, complaining of pain in the right hemithorax for 40 days. Additionally, the patient reported dyspnea at moderate stress and occasional dry cough. At clinical examination, decreased chest expansion and abolished vesicular murmur at the right lung base were observed. The patient was referred to the Unit of Radiology and Imaging Diagnosis to undergo chest radiography and computed tomography (CT).
Images description Figure 1. Digital chest radiograph. Mediastinal widening associated with opacification of the lower third of the right hemithorax. Right lung volume decrease.  Figure 1. Digital chest radiography. Figure 2. Chest CT, mediastinal window, contrast-enhanced coronal section. Homogeneous contrast-enhancement of a solid, lobulated, pleurodiaphragmatic mass at right. Pleural effusion at right. 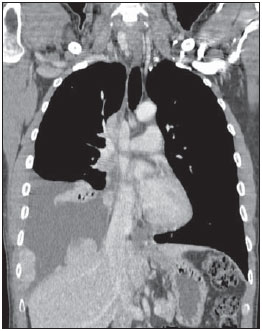 Figure 2. Chest CT, mediastinal window, contrastenhanced coronal section. Figure 3. Chest CT, mediastinal window, contrast-enhanced sagittal section. Homogeneous contrast-enhancement of anterior, mediastinal, solid, lobulated mass. Observe the loss of fat cleavage plane between the lesion and the pericardium, and base vessels.  Figure 3. Chest CT, mediastinal window, contrast-enhanced sagittal section. Figure 4. Chest CT, mediastinal window, non-contrast-enhanced (A) and contrast-enhanced (B) axial sections. Homogeneous contrast-enhancement of anterior, mediastinal, solid, lobulated mass. Observe the lobulated contour of the lesion, as well as the loss of fat cleavage plane between the lesion, the pericardium and the pleura. 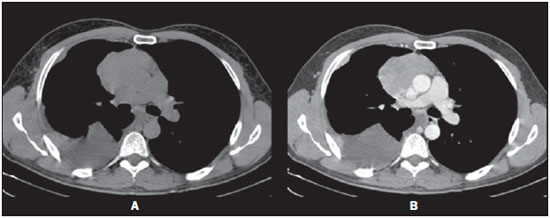 Figure 4. Chest CT, mediastinal window, non-contrastenhanced (A) and contrastenhanced (B) axial sections. Diagnosis: Invasive thymoma with pleural implants (drop metastases). COMMENTS Thymoma is a rare tumor-like entity. However, it is the most common primary neoplasia of the anterior mediastinum and the most frequent primary tumor of the thymus. Such disease predominantly affects adult individuals at the 5th–6th decades of life, with no gender predominance, and is rarely observed in children and in young individuals(1–3). Approximately 50% of the diagnoses are achieved in asymptomatic individuals submitted to chest radiography for other causes. In 25%–30% of cases, patients present signs and symptoms related to compression of adjacent mediastinal structures such as trachea, recurrent pharyngeal nerve and esophagus, manifesting as cough, dyspnea, chest pain, respiratory infections and dysphagia. Invasion of adjacent vascular structures may produce superior vena cava syndrome(2,4). About one third of patients with thymoma present myasthenia gravis and, conversely, 10%–15% of the patients with myasthenia have a thymoma. Association with other systemic diseases halve also been described, as follows: acquired hypogammaglobulinemia, erythrocyte cells aplasia, skin disorders, endocrinological disorders and even connective tissue disorders. Distant metastasis rarely occurs in cases of thymoma, but most commonly extends to the pleura, bones, liver, kidneys and nervous system(5,6). Differential diagnoses for thymoma include anterior mediastinal lesions, including thymic lesions, lymphomas, germ cell tumor (GCT) and thyroid goiter. It is important to remind that lymphomas may present either as a primary anterior mediastinal lesion or with thymic infiltration. In men, the most common CGT presentation is the seminoma, affecting patients in the third decade of life, usually extending towards to the left side of the midline and with mediastinal lymphadenomegaly(7). In the present case, the patient’s age range, the fact that the pleural implants were only at the right side, and the absence of mediastinal lymphadenomegaly and thyroid alterations corroborated the diagnosis of thymoma. The most frequent radiographic finding of thymoma is a mass with soft tissues density, measuring 5–10 cm, and generally with lobulated margins. The most frequent site is close to large vessels and to the pericardium, less frequently close to the cardiophrenic angle and cardiac border, and rarely in the neck or in other mediastinal compartment (Figures 1 and 3). On lateral views, opacity can be observed in the retrosternal space. Areas of calcification can be observed on plain radiographs(1). CT is the method of choice for the diagnosis of thymoma because of its sensitivity and capacity of demonstrating tumor infiltration of fat planes, vascular structures, adjacent lung and pleural dissemination(1,2,5). In most of cases, the images demonstrate a homogeneously contrast-enhanced solid lesion, however areas of lower density may be observed within the lesion, possibly corresponding to cysts, necrosis or hemorrhage. Generally, such lesions extend towards one of the sides of the anterior mediastinum – in the present case the lesion extended towards the right side (Figure 4). In this patient, a predominantly pleural involvement was observed, this presentation being rarely described in the literature. In cases where the disease is present, unilateral involvement is observed, manifesting either as nodular or diffuse pleural masses, pleural effusion and even with circumferential thickening. The presence of pleurodiaphragmatic implants (drop metastases) is compatible with the invasive thymoma presentation (Figure 2), typically occurring in the ipsilateral pleural space, with possibility of coalescence and development of a tumor crust(1,2). Magnetic resonance imaging does not add significant information as compared with computed tomography of the thymus, but the multiplanar evaluation may be important in cases of dubious CT, besides being an excellent method for defining vascular invasion by the lesion, without requiring the utilization of intravenous contrast media(8). Although surgical management is the most widely known treatment for thymomas, chemotherapy was chosen in the present case, because of the finding of multiple implants. The patient was referred to the oncology ambulatory, where stage IVa was determined according to the system proposed by Masaoka et al.(9). At the time the present report was completed, the patients had already completed the second chemotherapy cycle (cisplatin, doxorubicin and prednisone) with satisfactory clinical progression. REFERENCES 1. Nasseri F, Eftekhari F. Clinical and radiologic review of the normal and abnormal thymus: pearls and pitfalls. Radiographics. 2010;30:413–28. 2. Nishino M, Ashiku SK, Kocher ON, et al. The thymus: a comprehensive review. Radiographics. 2006;26:335–48. 3. Kallás E, Hueb AC, Kallás IE, et al. Timoma do mediastino médio: relato de caso. Rev Bras Cir Cardiovasc. 2005;20:189–91. 4. Santana L, Givica A, Camacho C; Armed Forces Institute of Pathology. Best cases from the AFIP: thymoma. Radiographics. 2002;22 Spec No:S95–S102. 5.Tecce PM, Fishman EK, Kuhlman JE. CT evaluation of the anterior mediastinum: spectrum of disease. Radiographics. 1994;14:973–90. 6. Shimosato Y, Mukai K. Tumors of the thymus and related lesions. In: Shimosato Y, Mukai K, editors. Atlas of tumor pathology: tumors of the mediastinum, fasc 21, ser 3. Washington, DC: Armed Forces Institute of Pathology; 1997. p. 158–68. 7. Lee KS, Im GJ, Han CH, et al. Malignant primary germ cell tumors of the mediastinum: CT features. AJR Am J Roentgenol. 1989;153:941–51. 8. Inaoka T, Takahashi K, Mineta M, et al. Thymic hyperplasia and thymus gland tumors: differentiation with chemical shift MR imaging. Radiology. 2007;243:869–76. 9. Masaoka A, Monden Y, Nakahara K, et al. Followup study of thymomas with special reference to their clinical stages. Cancer. 1981;48:2485–92. 1. MDs, Residents in Radiology and Imaging Diagnosis at Hospital das Clínicas da Universidade Federal de Goiás (HC-UFG), Goiânia, GO, Brazil. 2. PhD, Associate Professor and Head of Department of Radiology and Imaging Diagnosis at Hospital das Clínicas da Universidade Federal de Goiás (HC-UFG), Goiânia, GO, Brazil. 3. MD, Radiologist at Clínica Multimagem Diagnósticos, Goiânia, GO, Brazil. 4. Graduate Student of Medicine, Faculdade de Medicina da Universidade Federal de Goiás (UFG), Goiânia, GO, Brazil. Mailing Address: Dr. Pedro José de Santana Júnior Rua T-36, nº 3485 Edifício Solar dos Tocantins, ap. 104, Setor Bueno Goiânia, GO, Brazil, 74223-050 E-mail: psantanajr@hotmail.com Study developed at Department of Radiology and Imaging Diagnosis, Hospital das Clínicas da Universidade Federal de Goiás (HC-UFG), Goiânia, GO, Brazil. |
|
GN1© Copyright 2025 - All rights reserved to Colégio Brasileiro de Radiologia e Diagnóstico por Imagem
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554