Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 5 - Sep. / Oct. of 2010
Vol. 43 nº 5 - Sep. / Oct. of 2010
|
ORIGINAL ARTICLE
|
|
CT enterography: a preliminary experience in the evaluation of small bowel diseases |
|
|
Autho(rs): Luciana Costa-Silva1; Tatiana Martins2; Maria do Carmo Friche Passos3 |
|
|
Keywords: Enterography; Computed tomography; Small bowel; Crohn’s disease. |
|
|
Abstract: INTRODUCTION
Traditionally, the radiological study of the small bowel has always been performed by means of barium studies, such as conventional enteroclysis and small bowel follow-through, this later being, for many years, considered the standard imaging method(1). However, as a consequence of advances obtained with the introduction of multidetector computed tomography and the wide variety of available enteric contrast media, CT enterography has become the method of choice in the evaluation of small bowel diseases, being increasingly utilized(2). This is a method that provides high spatial resolution, allowing the visualization of the lumen and the mucosal relief, with the main advantage of evaluating the parietal thickness, in addition to eventual association with mesenteric and extraintestinal findings(3). The most common indications for the examination include the detection and follow- up of inflammatory bowel diseases, particularly Crohn’s disease, investigation of small bowel tumors, abdominal pain and diarrhea of unknown origin, and obscure gastrointestinal bleeding. It allows identification of hypervascular lesions, bowel dilatation, stenosis, fistulas, hyperenhancing bowel segments, as well as other abdominal findings. Thus, CT enterography has extensive clinical applicability, particularly in Crohn’s disease, providing data on activity and possible associated complications(2,4,5). The aim of this study is to demonstrate how this method can contribute with the diagnostic elucidation and clinical management of bowel diseases. The small bowel has always been considered as a structure of difficult propedeutic evaluation, because of its extensive length, presence of folds, its position in the digestive tube between the stomach and the large bowel, its tortuosity and loops overlapping(6). CT enterography, with its thin slices and multiplanar reconstruction, minimizes such limitations and many times provides a greater amount of data than other imaging methods such as capsule endoscopy and enteroscopy, enhancing the role of radiological studies in the enteral assessment(6,7). Considering the simplicity and swiftness of this noninvasive method, it is important to disseminate the technique describing its main findings. MATERIALS AND METHODS From May 2008 to March 2009, 35 patients (mean age, 43.46 years, standard deviation: 19.18 years, 62.9% women) were submitted to CT enterography in a private institution for suspicion of small-bowel lesions and were retrospectively evaluated. The present study was not submitted to the analysis by a Committee for Ethics in Research as it did not exist in the institution at the time of data collection. Patients were instructed to drink 70 g of polyethylene glycol diluted in 1,000 ml of water, divided in two doses: 40 minutes and 20 before the examination. Immediately before the images acquisition, the patients were instructed to drink 350 ml of water to allow an appropriate distention of the stomach, duodenum and proximal jejunum. The studies were performed by using a 16-detector row CT scanner (Philips Medical Systems; Best, The Netherlands). Contrast- enhanced biphasic CT images (arterial and enteric phases) were acquired at 30 and 55 seconds by using automatic power injector, 1.5 mm section thickness and 1.5– 2.0 ml/kg of non-ionic iodinated contrast medium per body weight at a rate of 3 ml/sec. Main indication for the studies included diagnostic evaluation or management of Crohn’s disease (n = 14; 40.0% of the cases) and evaluation of abdominal pain of unknown origin (n = 11; 31.4% of the cases). Other indications included investigation of neoplasias in seven patients, chronic diarrhea of unknown origin in two, and management of celiac disease in one patient. All the images were reviewed at the workstation by a single radiologist with a 13-year experience in abdominal imaging. Several parameters were evaluated at CT enterography: small bowel wall thickness, pattern of enhancement, pattern of distribution and aspect of connivent valves, bowel loops diameter, extent and localization of the disease, besides extraparietal alterations, such as engorged vasa recta, perienteric inflammatory changes and lymphadenomegaly. The presence of fistulas, abscesses, stenosis and bowel dilatation were also investigated. Bowel loops with a mean diameter of 25.0 mm, achieving 35.0 mm in the jejunum and 30.0 mm in the ileum were considered normal, with the usual parietal thickness ranging from 1.0 to 2.0 mm. It is known that, on average, the jejunum presents four to seven folds every 2.5 cm, and the ileum, three to five folds in the same length(8). One of the findings in celiac disease was the reversal jejunoileal fold pattern. In the evaluation of bowel tumor, the presence of focal thickening or vegetative lesions was evaluated. Nodes whose smallest axis was over 10 mm were interpreted as pathological. Pathologic mural enhancement refers to segmental hyperattenuation of bowel loops relative to nearby normalappearing. Hyperenhancement is one of the main criteria indicating active inflammatory Crohn’s disease. Subsequently, CT findings were correlated with clinical, laboratory, endoscopic and, whenever present, histopathological data; and in all the cases were discussed with the respective assistant-physician. Previously to the examination, the patients answered a questionnaire on the signs and symptoms. After CT enterography, the patients answered questions on their tolerance and acceptance towards the method. RESULTS The examination was well-tolerated by all the patients tolerated, with appropriate ingestion of the neutral oral contrast, which allowed adequate luminal distension (Figure 1). Among the 35 patients included in the present study, CT enterography demonstrated abnormalities in 25. Among the 14 patients whose indication was evaluation of Crohn’s disease, signs of disease activity were observed in eight patients (57%), with identification of mural thickening and hyperenhancement in 100% of the cases (Figure 2). In the other six cases, signs compatible with the presence of Crohn’s disease were observed, although without suggesting the presence of inflammatory activity at the moment of the examination. The presence of fistulas was demonstrated in seven patients (87% of the patients with activity) (Figures 3 and 4). 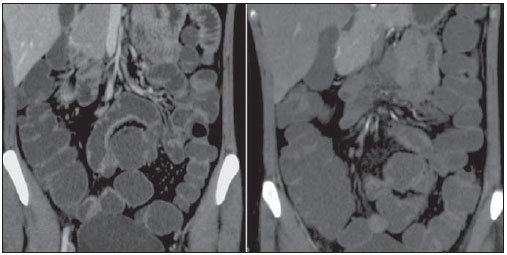 Figure 1. CT enterography, coronal section of a 30-year-old female patient. The study was performed after oral ingestion of non-absorbable neutral contrast medium (polyethylene glycol), demonstrating good distension of different intestinal segments, from the jejunum to the ileum, with appropriate contrastenhancement of the intestinal walls. 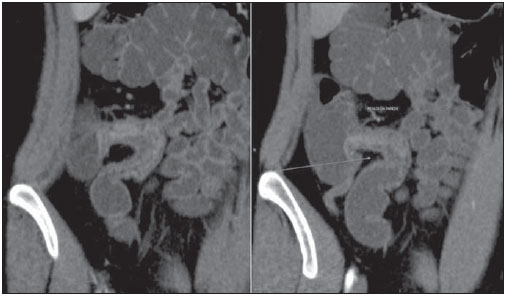 Figure 2. Female, 22-year-old patient. Slightly increased C-reactive protein level. Mild to moderate thickening of the terminal ileum walls, in association with parietal stratification and mildly increased contrastenhancement indicative of Crohn’s disease with mild inflammatory activity. 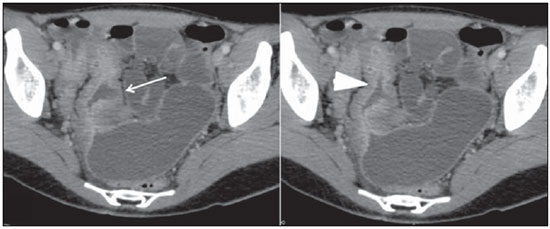 Figure 3. CT enterography image in the axial plane, of 18-year-old patient with diarrhea and abdominal pain of undefined etiology. Significant parietal thickening of the distal ileum, with parietal stratification and increased contrast-enhancement (arrowhead), associated to a blind fistula (arrow) on the medial wall. Definite diagnosis: Crohn’s disease. 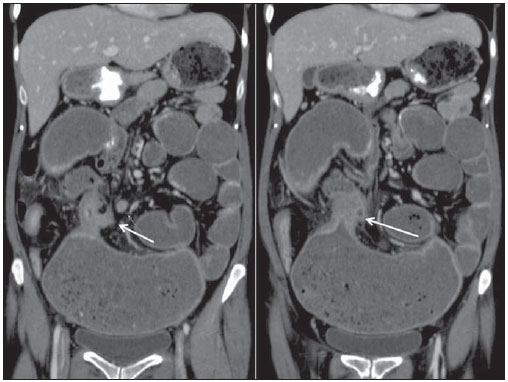 Figure 4. 36-year-old patient with Crohn’s disease. CT enterography demonstrates severe thickening of the distal ileum, with stenosis and significant upstream dilation. There is linear pathway originating from he above mentioned segment towards the transverse colon, characterizing enterocolic fistula (arrows). In two cases previously unsuspected carcinoid tumors were identified (Figure 4). The patients were surgically treated, and anatomopathological results confirmed the diagnosis. In a patient whose indication was celiac disease, CT enterography demonstrated typical findings of the disease, with the classical aspect of reversed jejunoileal fold pattern, with smooth and regular appearance of jejunal loops related to villous atrophy and increased number of connivent valves in the ileum, characterizing the “jejunization” pattern (Figure 5). 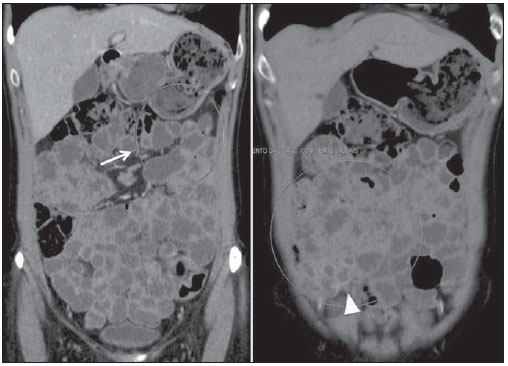 Figure 5. Female, 46-year-old patient, diagnosed with celiac disease. CT enterography demonstrates reversed pattern of the jejunoileal folds with loss of conniving valves and villous atrophy of the jejunum (arrow) associated to ileal jejunization represented by the high number of ileal folds (arrowhead). DISCUSSION CT enterography is a study based on distension of bowel loops by neutral peroral enteric contrast medium associated with intravenous iodinated contrast injection(9). Such method differs from conventional abdominal and pelvic computed tomography mainly by the utilization of neutral oral contrast medium(2,3). While water is the most readily available neutral enteric contrast agent, other agents that distend the small bowel wall to a greater extent – such as methylcellulose solution, polyethylene glycol solution, lactulosis and low-attenuation barium suspensions – are increasingly being employed. Considering that the satisfactory luminal distension is indispensable for the appropriate interpretation of the images, water is not considered as a good contrast medium for enterography, as it is rapidly absorbed along the intestine(4). Thus, nonabsorbable agents such as polyethylene glycol are preferred(10). Macari et al have considered that appropriate luminal distension is achieved when the small bowel diameter corresponds to at least 2 cm(9). Other authors consider the distension ideal in the presence of intraluminal contrast separating the intestinal walls, allowing the identification of folds, without loops collapsing(11,12). Satisfactory intestinal distension was achieved in all examinations performed in the present study with the oral polyethylene glycol, allowing an appropriate evaluation, without masking or simulating alterations that could lead to false-negative or false-positive results. In spite of controversies on the best way to administer the contrast medium, recent studies, such as the one developed by Wold et al., have demonstrated that there is no statistically significant difference between enterography and enteroclysis regarding intestinal loops distension(11). As regards the acceptance of contrast medium ingestion, the authors could observe that all patients included in the present study presented good tolerance to the amount and the interval of administration of the oral contrast medium, which is in agreement with data reported in the literature, leading to increased use of the technique over enteroclysis(11,13). However, inpatients were not evaluated in the present study. In such cases, sometimes because of the patients’ poor general condition, the utilization of the technique may not be feasible, and enteroclysis may be necessary, in spite of being more time consuming, uncomfortable and more expensive for the patient. CT enterography allows the evaluation of each intestinal segment without loop superimposition, providing data on the parietal involvement and allowing the evaluation of the surrounding mesentery, perienteric fat and other abdominal structures. The judicious interpretation of the images is based on the analysis of the lesion location in the small bowel, on the pattern and intensity of the parietal contrast uptake, involvement extent, the degree of parietal thickening, besides other associated findings. The main clinical application of CT enterography is the evaluation of patients with suspected or confirmed(3) Crohn’s disease. The main advantage of the method in the study of the intestinal transit in Crohn’s disease is the possibility of evaluating bowel wall and perienteric structures with a noticeable higher accuracy in the evaluation of fistulas and abscesses, with both intra- and interobserver reproducibility(14). The early recognition of fistulas and abscesses is of paramount relevance, in an attempt to reduce hospital stay time and complications in patients with penetrating and stenosing presentations of Crohn’s disease, considering the highest rate of hospitalization and reoperation along the disease progression among these patients(15)(Figure 6). 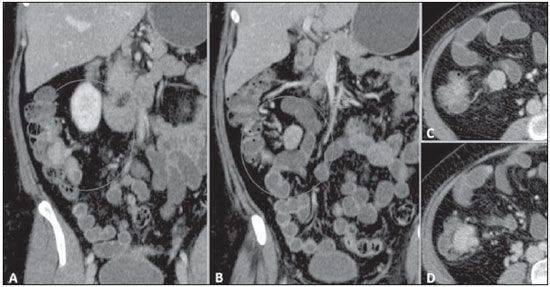 Figure 6. CT enterography, coronal (A,B) and axial plane (C,D): expansile hypervascular lesion in the terminal ileum. Regional mesenteric lymphadenomegaly. Anatomopathological study: terminal ileum carcinoid with lymph node involvement. Findings such as mural thickening, mural hyperenhancement, parietal stratification, increased attenuation of the perienteric fat, lymphadenomegaly, engorged of the vasa recta (the comb sign), fistulas or abscesses have been associated to active inflammatory Crohn’s disease(16)(Figure 7). Parietal thickening and enhancement represent the most sensitive criteria, and were observed in all the patients with active disease in the present series(2,4,17,18). Vasa recta engorgement and densification of perienteric fat are the most specific findings indicating disease activity(18). 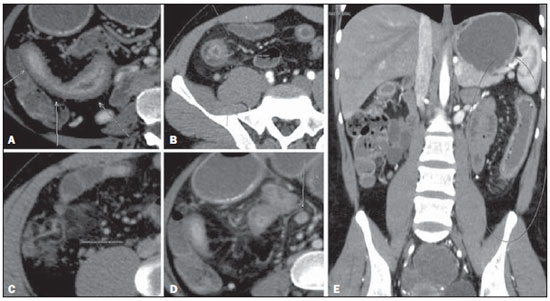 Figure 7. Crohn’s disease with moderate to severe inflammatory activity. On A and B, increased parietal contrast uptake, thickening and stratification of the terminal ileum wall (related to mucosal enhancement and submucosal edema) can be observe on axial sections; on C, densification of perienteric mesenteric fat; on D, reactional mesenteric lymphadenomegaly; on E, engorgement of intestinal vessels (vasa recta) related to the affected segment, image in the coronal plane. Another important application of CT enterography in patients presenting with Crohn’s disease coursing with abdominal pain is the differential diagnosis of parietal stenosis, whether of fibrotic/cicatricial origin or secondary to edema/spasm in cases of inflammatory activity (Figure 8). It is known that patients with active disease may benefit from the use of steroids, while for those patients with chronic disease, surgery seem to be the best alternative(4,19). 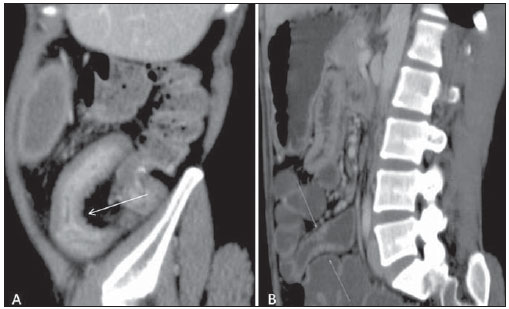 Figure 8. Crohn’s disease. Active inflammation (A) versus fibrostenosis (B), reformatted images in the sagittal plane. Increased contrast-enhancement in the mucosa, submucosal edema and parietal thickening (arrow on A). On B, a subtle parietal thickening is observed, however the enhancement of the involved segment is similar to that of the adjacent intestinal loops. In spite of the wide applicability and the excellent results of CT enterography in the evaluation of Crohn’s disease, such method involves the use of ionizing radiation. It is known that the disease affects mainly young adults who, usually, will be submitted to several examinations along their lives. Thus, other propedeutic methods such as ultrasonography or MR enterography may be considered. Intestinal tract tumors may also be detected at CT enterography. Small bowel neoplasias are rare, representing approximately 3% to 6% of all cancers of the digestive tract(20). Carcinoid tumors tend to appear as thickening areas or polyps with intensely contrast enhancement, most frequently in the ileum(2). In the present study, two cases were identified in this site. Because of technical characteristics related to a more appropriate loops distension and greater capacity to evaluate parietal hyperenhancing, CT enterography can best demonstrate such tumors. Celiac disease is a self-immune disorder whose definite diagnosis is achieved by means of intestinal biopsy(21). However, some imaging findings are suggestive of the disease, particularly in advanced stages, when the usual jejunoileal folds pattern reversal can be identified, most clearly demonstrated on coronal reconstructions(22). Nonspecific alterations such as loops dilation, folds separation, intussusception and extraintestinal alterations, such as lymphadenomegaly and even eventual complications of the disease may also be observed(2,21). Another indication for CT enterography reported in some studies is the evaluation of gastrointestinal bleeding, overt or occult. It seems that this method and the endoscopic capsule play complementary roles and that, because of the inherent difficulties of the later such as the identification of the lesion site, visualization impaired by the presence of fluid and intraluminal blood or absence of loops distension, CT enterography may in some cases demonstrate lesions otherwise undetectable by the endoscopic capsule(23,24). Further studies are necessary to define its role in the evaluation of intestinal hemorrhages. CONCLUSION The preliminary study allows the observation that CT enterography has demonstrated to be useful in the diagnosis of intestinal disorders, particularly in the evaluation of the inflammatory bowel diseases. It is an image method with a cost similar to that of the conventional abdominal computed tomography, swift and with good acceptance and tolerance by patients. Its applicability has increased and, certainly, it will be increasingly utilized in the clinical and radiological practice. REFERENCES 1. Horsthuis K, Stokkers PCF, Stoker J. Detection of inflammatory bowel disease: diagnostic performance of cross-sectional imaging modalities. Abdom Imaging. 2008;33:407–16. 2. Paulsen SR, Huprich JE, Fletcher JG, et al. CT enterography as a diagnostic tool in evaluating small bowel disorders: review of clinical experience with over 700 cases. Radiographics. 2006;26:641–57. 3. Hara AK, Alam S, Heigh RI, et al. Using CT enterography to monitor Crohn’s disease activity: a preliminary study. AJR Am J Roentgenol. 2008;190:1512–6. 4. Hara AK, Swartz PG. CT enterography of Crohn’s disease. Abdom Imaging. 2009;34:289–95. 5. Booya F, Akram S, Fletcher JG, et al. CT enterography and fistulizing Crohn’s disease: clinical benefit and radiographic findings. Abdom Imaging. 2009;34:467–75. 6. Hara AK, Leighton JA, Sharma VK, et al. Imaging of small bowel disease: comparison of capsule endoscopy, standard endoscopy, barium examination, and CT. Radiographics. 2005;25:697–711. 7. Fidler J. Feature section, small bowel disease: CT imaging. Abdom Imaging. 2009;34:281. 8. Federle MP, Jeffrey RB, Desser TS, et al. Diagnostic imaging: abdomen. Salt Lake, UT: Amirsys; 2004. 9. Macari M, Megibow AJ, Balthazar EJ. A pattern approach to the abnormal small bowel: observations at MDCT and CT enterography. AJR Am J Roentgenol. 2007;188:1344–55. 10. Mazzeo S, Caramella D, Battolla L, et al. Crohn disease of the small bowel: spiral CT evaluation after oral hyperhydration with isotonic solution. J Comput Assist Tomogr. 2001;25:612–6. 11. Wold PB, Fletcher JG, Johnson CD, et al. Assessment of small bowel Crohn disease: noninvasive peroral CT enterography compared with other imaging methods and endoscopy – feasibility study. Radiology. 2003;229:275–81. 12. Megibow AJ, Babb JS, Hecht EM, et al. Evaluation of bowel distention and bowel wall appearance by using neutral oral contrast agent for multidetector row CT. Radiology. 2006;238:87–95. 13. Fletcher JG. CT enterography technique: theme and variations. Abdom Imaging. 2009;34:283–8. 14. Lee SS, Kim AY, Yang SK, et al. Crohn disease of the small bowel: comparison of CT enterography, MR enterography, and small-bowel followthrough as diagnostic techniques. Radiology. 2009;251:751–61. 15. Veloso FT, Ferreira JT, Barros L, et al. Clinical outcome of Crohn’s disease: analysis according to the Vienna classification and clinical activity. Inflamm Bowel Dis. 2001;7:306–13. 16. Huprich JE, Fletcher JG. CT enterography: principles, technique and utility in Crohn’s disease. Eur J Radiol. 2009;69:393–7. 17. Bodily KD, Fletcher JG, Solem CA, et al. Crohn disease: mural attenuation and thickness at contrast- enhanced CT enterography – correlation with endoscopic and histologic findings of inflammation. Radiology. 2006;238:505–16. 18. Baker ME, Walter J, Obuchowski NA, et al. Mural attenuation in normal small bowel and active inflammatory Crohn’s disease on CT enterography: location, absolute attenuation, relative attenuation, and the effect of wall thickness. AJR Am J Roentgenol. 2009;192:417–23. 19. Higgins PD, Caoili E, Zimmermann M, et al. Computed tomographic enterography adds information to clinical management in small bowel Crohn’s disease. Inflamm Bowel Dis. 2007;13:262–8. 20. Masselli G, Polettini E, Casciani E, et al. Smallbowel neoplasms: prospective evaluation of MR enteroclysis. Radiology. 2009;251:743–50. 21. Soyer P, Boudiaf M, Fargeaudou Y, et al. Celiac disease in adults: evaluation with MDCT enteroclysis. AJR Am J Roentgenol. 2008;191:1483–92. 22. Tomei E, Marini M, Messineo D, et al. Computed tomography of the small bowel in adult celiac disease: the jejunoileal fold pattern reversal. Eur Radiol. 2000;10:119–22. 23. Huprich JE, Fletcher JG, Alexander JA, et al. Obscure gastrointestinal bleeding: evaluation with 64-section multiphase CT enterography – initial experience. Radiology. 2008;246:562–71. 24. Singh V, Alexander JA. The evaluation and management of obscure and occult gastrointestinal bleeding. Abdom Imaging. 2009;34:311–9. 1. Master, MD, Radiologist, Assistant Professor at Department of Supplementary Propedeutics, Faculdade de Medicina da Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil. 2. MD, Radiologist, Specialist in Radiology and Imaging Diagnosis, Ecoar Medicina Diagnóstica, Belo Horizonte, MG, Brazil. 3. PhD, Associate Professor-2 at Department of Medical Practice, Universidade Federal de Minas Gerais (UFMG), Belo Horizonte, MG, Brazil. Mailing address: Dra. Luciana Costa Silva Rua Antônio de Albuquerque, 1021/901, Lourdes Belo Horizonte, MG, Brazil, 30112-011 E-mail: costaluciana@terra.com.br Received February 17, 2010 Accepted after revision September 16, 2010 Study developed at the Unit of Radiology and Imaging Diagnosis, Ecoar Medicina Diagnóstica, Belo Horizonte, MG, Brazil |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554