Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 5 - Sep. / Oct. of 2010
Vol. 43 nº 5 - Sep. / Oct. of 2010
|
ORIGINAL ARTICLE
|
|
Low-dose dobutamine myocardial perfusion scintigraphy in the identification of viable myocardium |
|
|
Autho(rs): Renata Freire de Moraes1; José Cláudio Meneghetti2; Adelanir Antonio Barroso3 |
|
|
Keywords: Left ventricular dysfunction; Dobutamine; Scintigraphy. |
|
|
Abstract: INTRODUCTION
The universe of patients presenting with ischemic cardiomyopathy is increasing worldwide, mainly because of the decrease in mortality rates as a consequence of the effective treatment of acute coronary syndromes. Two thirds of the patients with heart failure present coronary artery disease as the main etiology(1). The long-term prognosis for heart failure is quite unfavorable, being accountable for 20% of all hospitalizations of individuals above 65 years of age, with an annual mortality rate close to 45%(2). Ischemic ventricular dysfunction may result from the presence of scar or hibernation, stunning and ischemic preconditioning as adaptive responses of the myocytes to the decrease in blood flow, reducing their metabolism in order to remain alive(2,3). The progression of ischemic cardiomyopathy can be modified with the recovery of myocardial contractility, once the coronary blood flow is reestablished(4). The identification of viable myocardium has become essential in the medical propedeutic, as in the presence of living tissue, post-revascularization contractility recovery may be obtained, with improvement in the patient’s quality of life and decrease in mortality(4–8). In a meta-analysis, Allmann et al.(9) have observed a significant association between revascularization and improvement in the survival of patients with coronariopathy and ventricular dysfunction, but with myocardial viability at imaging studies and that, the more deteriorated the left ventricular function, the better was the result. The annual mortality rate among patients with myocardial viability who were surgically treated was as low as 3.2% as compared with a rate of 16% for those submitted to pharmacological treatment. More than 40% of revascularized patients presented improvement in the left ventricle ejection fraction. A greater postoperative mortality was observed in the absence of myocardial viability, reflecting the high risk of the procedure in the absence of clinical benefit. Thallium-201 scintigraphy and stress echocardiography are the most utilized imaging methods for investigating of myocardial viability, considering the smaller availability of methods such as positron emission tomography and magnetic resonance imaging(10). Thallium-201, a potassium analog, identifies the cellular integrity, and echocardiography evaluates the contractile reserve through the inotropic stimulus of dobutamine(11). Both methods evaluate different parameters of myocardial viability, with differences in accuracy: thallium-201 presents a high sensitivity, while echocardiography presents a high specificity(12,13). Gated SPECT images allow the evaluation of the myocardial contractility, making the investigation of the contractile reserve possible, with the simultaneous evaluation of cellular integrity, which potentially would increment the specificity of scintigraphy in the investigation of viable myocardium(14). The objective of the present study was to evaluate the increase in specificity of dual isotope myocardial perfusion gated SPECT (99mTc-sestamibi/thallium-201), a highly sensitive method to detect viable myocardium, with addition of data on contractile reserve simultaneously acquired by low-dose dobutamine gated SPECT. MATERIALS AND METHODS Cellular integrity and contractile reserve of 260 myocardial segments were evaluated by means of scintigraphic techniques in 13 previously infracted patients with ischemic cardiomyopathy referred to the Unit of Nuclear Medicine for investigation of myocardial viability. The patients were subsequently revascularized and underwent scintigraphic follow-up for evaluation of postrevascularization contractile performance. The present study was approved by the Committee for Ethics in Research of the authors’ institutions, and the patients signed a term of free and informed consent for participating in the research protocol. The mean patients’ age was 58.9 years; 12 patients were men (92.3%) and one, woman (7.6%). The mean time elapsed from myocardial infarction ranged between 3 and 15 months and all the patients presented segmental contractile dysfunction at echocardiography. In this group, 7 patients (54%) had been previously revascularized, 11 (84.6%) reported angina, all of them (100%) presented hypertension, 9 (69.2%) dyslipidemia, and 5 (38.4%), diabetes. Seven patients (53.8%) reported regular use of beta blockers, seven (53.8%) used vasodilators and six (46.1%), calcium channel blockers. Dual isotope perfusion myocardial scintigraphy was performed with stress images (99mTc-sestamibi), rest and redistribution (thallium-201 chloride) for myocardial viability investigation. Stress images (99mTc-sestamibi) were acquired in synchronization with electrocardiography (gated SPECT), allowing the evaluation of contractile function through the analysis of parietal motility and systolic thickening (contractility), ejection fraction and cardiac volumes. A second acquisition (low-dose dobutamine gated SPECT) was added for evaluation of the myocardial contractile reserve. The improvement of the contractile dysfunction at the post-revascularization scintigraphic study (99mTc-sestamibi gated SPECT) was considered as parameter of myocardial viability. Images acquisition protocol A two-day protocol with rest/redistribution and stress phases in different days was utilized for images acquisition with the patients lying in the supine position, with the arms elevated above the head, in a VariCam® scintillation chamber (Elscint; Haifa, Israel) with detectors at 90° to each other, coupled with an eNtegra® workstation (General Electric Medical Systems; Milwaukee, WI, USA). A high-resolution collimator was utilized on a circular 180° orbit, initiating in a 45°oblique right anterior incidence with angular step of 6°, 64 × 64 matrix, zoom of 1.28 and 10% window at the photopeak and 140 keV for 99mTcsestamibi acquisitions and 72 and 163 keV for thallium-201 images. Attenuation correction was not performed. Rest and redistribution images were acquired after 4 hour-fasting, with an intravenous dose of 130 MBq of thallium-201 chloride (IPEN-CNEN), with rest images being acquired after 20 minutes in 30 steps of 35 seconds, and redistribution images four to six hours after, in 30 steps of 45 seconds. For the physical or pharmacological stress images acquisition, the ingestion of a light meal was allowed up to two hours previously to the examination, and the patients were encouraged to interrupt the use of beta blockers, calcium channel blockers and vasodilators for a period of 48 hours. Physical stress was achieved with maximum isotonic exercise on a treadmill utilizing the Bruce’s protocol with continuous hemodynamic and electrocardiographic monitoring. The 99mTc-sestamibi dose of 925 MBq was injected at the peak of the stress, as the submaximum heart rate was achieved 60 seconds before the end of the exercises, and the images were acquired 60 minutes afterwards. Pharmacological stress (dipyridamole) required previous suspension of xanthines, caffeine and derivatives. An intravenous dipyridamole dose (0.56 mg/kg) was administered over five minutes under continuous hemodynamic and electrocardiographic monitoring. The radiopharmaceutical drug was injected two minutes after completion of the coronary vasodilator infusion and the images were acquired 90 minutes afterwards. Two sets of CT images (gated SPECT) were acquired under stress and basal conditions and with low-dose dobutamine, with the cardiac cycle divided into eight pictures and images acquired in 30 steps of 30 seconds (Figure 1). Once the first acquisition was completed, continuous infusion of dobutamine (5 µg/kg/min) was started through peripheral vein by means of an infusion pump for five minutes, increasing to 10 to 15 µg/kg/min, coinciding with the beginning of images acquisition to its completion (15 minutes on average). 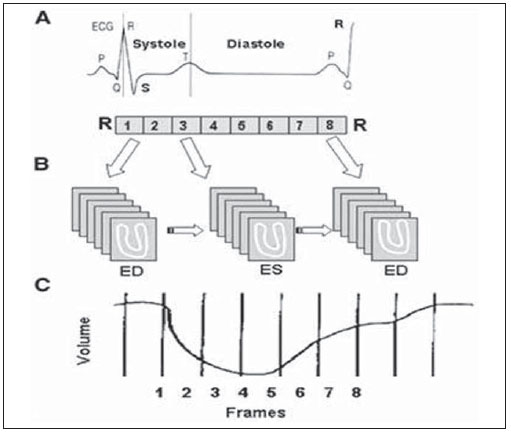 Figure 1. Gated SPECT acquisition and processing. A: Electrocardiographic representation of the cardiac cycle. B: Acquisition of images representative of the cardiac cycle divided into eight frames. C: Timeactivity curve of the tracer during the cardiac cycle. Images processing The images were processed by filtered retroprojection (Butterworth filter) at a cutoff frequency of 0.25 and order 5 for thallium-201 chloride and cut-off frequency of 0.5 and order 5 for 99mTc-sestamibi. For the analysis of results, the Cedars- Sinai Quantitative SPECT QGS/QPS application (Berman, Germano) (Elgems GE) was utilized, with the division of the heart into 20 segments and automatic quantification of the perfusion, parietal contractility and motility at different moments of the study (Figures 2 and 3). The method allows an increase in the number of relevant parameters that may be objectively measured and with reproducibility(15). 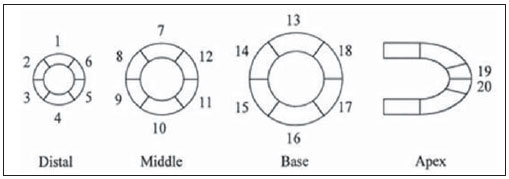 Figure 2. Myocardial segmentation model. Myocardial segments: distal anterior (1), medial (7), basal (13); distal anteroseptal (2), medial (8), basal (14); distal inferoseptal (3), medial (9), basal (15); distal inferior (4), medial (10), basal (16); inferolateral (5), medial (11), basal (17); anterolateral (6), medial (12), basal (18); distal antero-apical (19), distal infero-apical (20). 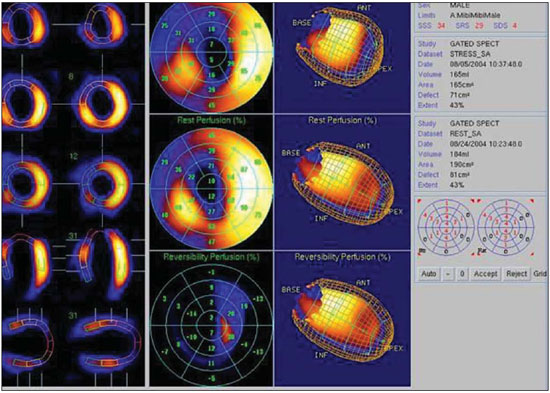 Figure 3. Graphic representation of functional gated SPECT images. From left to right: images of the heart at end-systole and diastole to evaluate systolic thickening; polar perfusion maps for analysis of perfusion reversibility, three-dimensional representation of the heart with delimitation of the epicardium and endocardium for visualization of parietal motility; value of ejection fraction, final diastolic and systolic volumes; schematic representation of the quantification of functional parameters of 20 myocardial segments of the left ventricle. Follow-up From the third month following myocardial revascularization, 99mTc-sestamibi gated SPECT was performed with images acquisition 45 minutes after intravenous 99mTc-sestamibi injection under basal conditions. Results analysis In order to evaluate perfusional viability, the statistically significant difference between the scores of the myocardial segments at the stress and rest and rest and redistribution images was analyzed. The difference between scores regarding systolic thickening and parietal motility under basal conditions and inotropic stimulus was evaluated to determine the myocardial contractile reserve. For analysis of post-revascularization improvement in contractility, differences between scores of contractility under basal and post-revascularization conditions were compared. Values for final diastolic and systolic volumes and left ventricle ejection fraction (LVEF) were analyzed under basal, inotropic and post-revascularization conditions. In the evaluation of the method specificity, the presence of contractile reserve in the segments with contractile dysfunction, myocardial viability at thallium-201, and improvement of contractility in the postrevascularization follow-up were taken into consideration. Statistical analysis Descriptive analysis of the studied variables was performed. Frequency distribution tables were constructed for categorical variables, and for the continuous variables, central trend measurement and scatterplots were calculated. The marginal homogeneity test was utilized for comparison of perfusion, contractility and parietal motility patterns of the myocardial segments in different situations. The McNemar’s test was utilized to evaluate the relationship between postrevascularization improvement and contractile reserve. Given the asymmetrical character of the distribution, the non-parametric paired Wilcoxon test was utilized to compare the measurements of final diastolic and systolic volumes and ejection fraction. A level of significance corresponding to 5% was considered in the analyses in the present study. The SPSS 12.0 and Statxact 6.0 softwares were utilized. RESULTS No symptom related to the intravenous dobutamine infusion was reported by the patients during the proposed scintigraphic study. Seven (53.8%) patients underwent pharmacological stress while six (46.2%) underwent isotonic exercise. Angioplasty with implant placement was performed in nine (69.2%) patients, and myocardial revascularization surgery was performed in four patients (30.7%). The post-revascularization follow-up was performed in a mean period of 8.8 months after the procedures. Functional parameters in basal conditions and under inotropic stimulus Tables 1 and 2 demonstrate statistically significant differences between the two moments (p-value < 0.001), with better contractility and parietal motility with lowdose dobutamine in relation to the basal study. 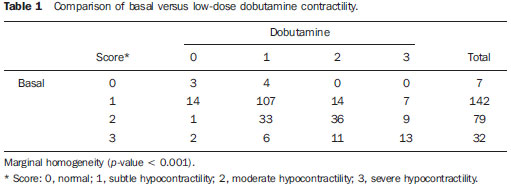 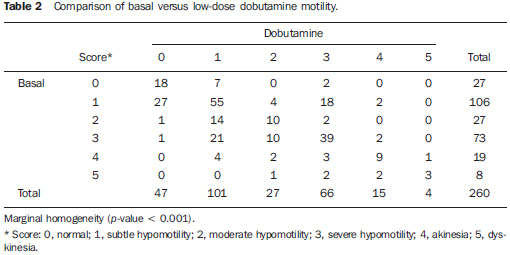 On average, the final diastolic and systolic volumes were smaller with the use of dobutamine (143.7 and 87.8) and greater in the basal study (151 and 100.6). The mean LVEF was smaller under basal condition (35%) than under dobutamine stimulus (41%). Functional parameters under basal conditions and in the postrevascularization follow-up Tables 3 and 4 demonstrate comparisons between contractility and parietal motility in the segments under basal condition and post-revascularization. Statistically significant differences were observed between the two moments (Table 3, p-value < 0.001; Table 4, p-value = 0.003), with greater post-revascularization contractility and parietal motility as compared with basal motility. 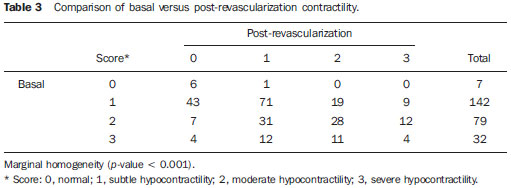 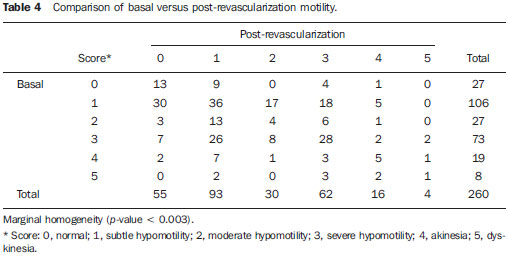 On average, the final diastolic and systolic volumes were smaller after revascularization (136.6 and 85), as compared with the basal study (151 and 100.6). The mean LVEF was smaller under basal condition (35%) and greater after revascularization (41%). Analysis of contractile performance in the post-revascularization scintigraphic follow-up of myocardial segments with contractile dysfunction but viable at thallium-201 Fifty-eight (22.4%) myocardial segments with contractile dysfunction presented stress-induced ischemia and 63 (24.3%) presented persistent hypoperfusion but viable at thallium-201. Overall, 98 myocardial segments (37.8%) were viable, i.e., presented stress-induced ischemia, viability at thallium-201 or both simultaneously. As basal and post-revascularization contractility of the 98 segments are compared, statistically significant differences are observed between the two moments (p-value = 0.008), with improvement in the contractility after revascularization. Table 5 shows that 58 segments presented no post-revascularization improvement and that contractile reserve was not observed in most of them (84.5%). The McNemar’s test demonstrated a borderline p-value (0.061), demonstrating a tendency towards a statistically significant result. 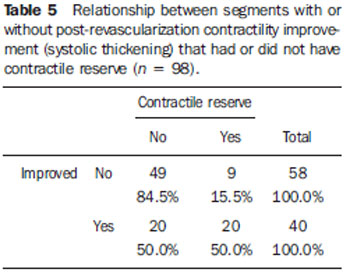 As basal and post-revascularization parietal motility of the 98 viable segments at thallium-201 are compared, no statistically significant difference can be confirmed between the two moments (p-value > 0.05). Additionally, the authors observed that 59 segments demonstrated no improvement in motility after revascularization. Among these segments, the majority (78%) did not present contractile reserve. However, according to the p-value demonstrated by the McNemar’s test (> 0.05), such result is not statistically significant. DISCUSSION The protocol described in the present study is simple and easy to perform. The patients presented good tolerance to the proposed scintigraphic procedure, and did not present symptoms during the intravenous dobutamine infusion. According to Kasama et al.(16), who have performed gated SPECT with low-dose dobutamine in 26 patients with dilated myocardiopathy, dobutamine in low doses presents a powerful chronotropic effect and minimum arrhythmogenic or vascular effect. The size of the sample was considered as a limiting factor in the present study. The investigation of viable myocardium by means of perfusion and myocardial metabolism studies by nuclear medicine is in agreement with initial reports on myocardial viability. The radioisotope techniques require few viable cells to demonstrate cellular integrity, but these cells may be insufficient for post-revascularization contractile recovery. It seems that the presence of a minimum amount of viable myocardium is required for the detection of contractile reserve(17). In an attempt to improve the specificity of thallium-201, a widely utilized method, some authors have reported experiments with low-dose dobutamine gated SPECT, similarly to stress echocardiography, to allow the analysis of perfusion and myocardial contractile reserve during a single examination. Different authors have also demonstrated that this technique is quite reproducible in relation to stress echocardiography and magnetic resonance imaging( 18,19). Yoshinaga et al.(20), in a study with 23 patients comparing 99mTc-sestamibi gated SPECT under low-dose dobutamine and with echocardiography and positronemission tomography, demonstrated a good correlation of the results of contractile reserve between the two methods. Leoncini et al.(21), in a study with 63 patients with 99mTc-sestamibi gated SPECT under lowdose dobutamine have observed 79% sensitivity and 78% specificity in the prediction of the post-revascularization increase in LVEF under inotropic stimulus. Simões et al.(22) have demonstrated the increase in methods accuracy from 0.69 to 0.84 with data regarding contractile reserve obtained by means of thallium-201 gated-SPECT under low-dose dobutamine. Duncan et al.(23) have studied 16 patients with 99mTc-sestamibi gated SPECT and confirmed the effectiveness of the method in the prediction of post-revascularization increase in ejection fraction, similarly to results reported by Leoncini et al.(21). For the 13 patients evaluated in the present study, myocardial viability at thallium-201 was considered in the presence of perfusional reversibility between the perfusion phases, regardless the uptake degree. Kitsiou et al.(24) have demonstrated that reversible thallium defects are more accurate in the prediction of post-revascularization contractile recovery than irreversible thallium defects with uptake > 50%, frequently corresponding to subendocardial fibrosis that cannot improve contractility after revascularization. The presence of myocardial ischemia is required for the contractile performance recovery after revascularization, i.e., that is, the artery accountable by the blood supply in the territory must be stenotic, or otherwise, in the presence of cellular structural damage the post-revascularization contractile recovery will not occur(25). Candell-Riera et al.(26) have performed an investigation on contractile reserve by means of low-dose dobutamine gated SPECT in patients with coronariopathy and reported that a negative contractile reserve was observed particularly in viable myocardial segments which did not recover contractility after revascularization and were supplied by a patent coronary artery. Positive contractile reserve was considered in the presence of improvement in the contractility of the investigated myocardial segments, independently of the increase in LVEF with inotropic stimulus. The increase in LVEF varied among the patients according to the viability parameters. The greater the myocardial viability at the perfusion evaluation, the greater was the increase in LVEF increase low-dose dobutamine. In order for the LVEF to increase after revascularization, a mass of at least 25% of viable tissue is necessary(27). In the evaluation of functional parameters, an increased final diastolic and systolic volumes and decreased mean LVEF value was observed under basal conditions, demonstrating the presence of significant ischemic cardiomyopathy among the patients. With dobutamine stimulus, the cardiac volumes decreased and the LVEF values presented statistically significant increase, like under basal conditions and after revascularization as the same parameters are considered. According to Schinkel et al.(28), the main objectives of myocardial revascularization are the improvement in LVEF (global systolic function), decrease in diastolic and systolic volumes (reverse remodeling), besides the improvement in segmental contractility and consequential improvement of heart failure symptoms, improvement in the quality of life and decrease in the mortality (sudden death). For the purposes of assessing the contractile reserve, the improvement of parietal motility and systolic thickening in the myocardial segments with contractile dysfunction but viable at thallium-201, were isolatedly evaluated. The separate analysis of the systolic thickening, as a functional parameter of contractile reserve, demonstrated results with borderline statistical significance, demonstrating a tendency towards high specificity in the investigation on contractile reserve with values close to those observed in the literature for stress echocardiography(11). The analysis of systolic thickening was statistically more significant than that of parietal motility, in agreement with data reported in the literature. Imaging methods utilized the evaluation of myocardial walls thickening such as echocardiography, computed tomography, magnetic resonance imaging and gated SPECT, allow the analysis of systolic thickening that is considered as a more sensitive indicator than parietal motility(29). CONCLUSION Dual isotope myocardial perfusion scintigraphy (gated SPECT), with addition of data on contractile reserve simultaneously acquired by low-dose dobutamine gated SPECT tends to present an effective contribution in the assessment of myocardial viability. Acknowledgments To Prof. Dr. Alfonso Barbato, Dr. Cristina Harumi Yamashiba, and the staff of Nuclear Medcenter. REFERENCES 1. Gheorghiade M, Bonow RO. Chronic heart failure in the United States: a manifestation of coronary artery disease. Circulation. 1998;97:282–9. 2. Mesquita CT, Félix RCM. Viabilidade miocárdica: uma visão crítica. Programa de Educação Continuada da Sociedade Brasileira de Cardiologia. Aterosclerose. 2004;2:27–32. 3. Canty JM, Fallavollita JA. Hibernating myocardium. J Nucl Cardiol. 2005;12:104–19. 4. Dellegrottaglie S, Perrone-Filardi P, Pace L, et al. Prediction of long-term effects of revascularization on regional and global left ventricular function by dobutamine echocardiography and rest Tl- 201 imaging alone and in combination in patients with chronic coronary artery disease. J Nucl Cardiol. 2002;9:174–82. 5. Soares Junior J. Diagnóstico da viabilidade do miocárdio. In: Thom AF, Smanio PEP. Medicina nuclear em cardiologia – da metodologia à clínica. São Paulo, SP: Atheneu; 2007. p. 199–212. 6. Di Carli MF, Asgarzadie F, Schelbert HR, et al. Quantitative relation between myocardial viability and improvement in heart failure symptoms after revascularization in patients with ischemic cardomiopathy. Circulation. 1995;92:3436–44. 7. Marwick TH, Zuchowski C, Lauer MS, et al. Functional status and quality of life in patients with heart failure undergoing coronary bypass surgery after assessment of myocardial viability. J Am Coll Cardiol. 1999;33:750–8. 8. Beller GA. Noninvasive assessment of myocardial viability. N Engl J Med. 2000;343:1488–90. 9. Allman KC, Shaw LJ, Hachamovitch R, et al. Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol. 2002;39: 1151–8. 10. Nelson C, McCrohon J, Khafagi F, et al. Impact of scar thickness on the assessment of viability using dobutamine echocardiography and thallium single-photon emission computed tomography: a comparison with contrast-enhanced magnetic resonance imaging. J Am Coll Cardiol. 2004;43: 1248–56. 11. Yao SS, Chaudhry FA. Assessment of myocardial viability with dobutamine stress echocardiography in patients with ischemic left ventricular disfunction. Echocardiography. 2005;22:71–83. 12. Bax JJ, Maddahi J, Poldermans D, et al. Sequential (201)Tl imaging and dobutamine echocardiography to enhance accuracy of predicting improved left ventricular ejection fraction after revascularization. J Nucl Med. 2002;43:795–802. 13. Bax JJ, Maddahi J, Poldermans D, et al Preoperative comparison of different noninvasive strategies for predicting improvement in left ventricular function after coronary artery bypass grafting. Am J Cardiol. 2003;92:1–4. 14. Candell-Riera J, Romero-Farina G, Milá M, et al. Low-dose dobutamine gated-SPECT analysis of left ventricular segmental wall thickening in ischemic cardiomiopathy. Rev Esp Cardiol. 2008; 61:1061–9. 15. Germano G, Berman DS. Clinical gated cardiac SPECT. Armonk, NY: Futura Publishing; 1999. 16. Kasama S, Toyama T, Kumakura H, et al. Myocardial contractile reserve determined by dobutamine stress Tc-99m tetrofosmin quantitative gated SPECT predicts late spontaneous improvement in cardiac function in patients with recentonset dilated cardiomyopathy. J Nucl Cardiol. 2003;10:607–14. 17. Baumgartner H, Porenta G, Lau YK, et al. Assessment of myocardial viability by dobutamine echocardiography, positron emission tomography and thallium-201 SPECT: correlation with histopathology in explanted hearts. J Am Coll Cardiol. 1998;32:1701–8. 18. Strach K, Meyer C, Schild H, et al. Cardiac stress MR imaging with dobutamine. Eur Radiol. 2006;16:2728–38. 19. Heilmaier C, Bruder O, Meier F, et al. Dobutamine stress cardiovascular magnetic resonance imaging in patients after invasive coronary revascularization with stent placement. Acta Radiol. 2009;50:1134–41. 20. Yoshinaga K, Morita K, Yamada S, et al. Low-dose dobutamine electrocardiograph-gated myocardial SPECT for identifying viable myocardium: comparison with dobutamine stress echocardiography and PET. J Nucl Med. 2001;42:838–44. 21. Leoncini M, Sciagrà R, Maioli M, et al. Usefulness of dobutamine Tc-99m sestamibi-gated single-photon emission computed tomography for prediction of left ventricular ejection fraction outcome after coronary revascularization for ischemic cardiomyopathy. Am J Cardiol. 2002;89: 817–21. 22. Simões MV, Almeida-Filho OC, Pintya AO, et al. Prediction of left ventricular wall motion recovery after acute myocardial infarction by Tl-201 gated SPECT: incremental value of integrated contractile reserve assessment. J Nucl Cardiol. 2002;9:294–303. 23. Duncan BH, Ahberg AW, Marini D, et al. Regional left ventricular response to low-dose dobutamine infusion during ECG-gated Tc-99m-sestamibi SPECT image acquisition accurately predicts global left ventricular function after revascularization in patients with coronary artery disease and left ventricular dysfunction. J Am Coll Cardiol. 2000;35:446A. 24. Kitsiou AN, Srinivasan G, Quyyumi AA, et al. Stress-induced reversible and mild-to-moderate irreversible thallium defects: are they equally accurate for predicting recovery of regional left ventricular function after revascularization? Circulation. 1998;98:501–8. 25. Travin MI, Bergman SR. Assessment of myocardial viability. Semin Nucl Med. 2005;35:2–16. 26. Candell-Riera J, Romero-Farina G, Milá M, et al. Negative contractile reserve with low-dose dobutamine in patients with ischemic cardiomyopathy investigated by gated myocardial perfusion SPECT. Rev Esp Cardiol. 2010;63:181–9. 27. Vitola JV, Delbeke D. Nuclear cardiology & correlative imaging. A teaching file. New York, NY: Springer; 2004. 28. Schinkel AFL, Poldermans D, Elhendy A, et al. Assessment of myocardial viability in patients with heart failure. J Nucl Med. 2007;48:1135–46. 29. Camici PG, Prasad SK, Rimoldi OE. Stunning, hibernation, and assessment of myocardial viability. Circulation. 2008;117:103–14. 1. PhD, Nuclear Physician at Division of Nuclear Medicine, Department of Molecular Imaging and Diagnosis of Instituto Hermes Pardini, Belo Horizonte, MG, Brazil. 2. Doctor Professor, Director for the Unit of Nuclear Medicine and Molecular Imaging of Instituto do Coração (InCor) – Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil. 3. Master, Nuclear Physician, Director for Nuclear Medcenter, Belo Horizonte, MG, Brazil. Mailing address: Dra. Renata Freire de Moraes Instituto Hermes Pardini, Divisão de Medicina Nuclear Rua dos Aimorés, 66, Funcionários Belo Horizonte, MG, Brazil, 30140-070 E-mail: renatafreire@yahoo.com.br Received January 10, 2010 Accepted after revision August 11, 2010 Study developed in the Department of Radiology at Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, and in the Unit of Nuclear Medicine at Hospital Socor/Nuclear Medcenter, Belo Horizonte, MG, Brazil |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554