Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 4 - July / Aug. of 2010
Vol. 43 nº 4 - July / Aug. of 2010
|
CASE REPORT
|
|
Primary acalvaria: a case report |
|
|
Autho(rs): Lívia Teresa Moreira Rios1; Marília da Glória Martins2; Vanda Maria Ferreira Simões3; Marynéa do Vale Nunes4; Patrícia Franco Marques5; Silvia Helena Cavalcante de Souza Godoy6 |
|
|
Keywords: Primary acalvaria; Skull defect; Congenital malformation. |
|
|
Abstract: INTRODUCTION
Acalvaria is a rare congenital malformation of unknown pathogenesis characterized by the absence of the flat bones of the cranial vault, dura mater and associated muscles, whit normal skull base and facial bones. The brain tissue is usually preserved although in some cases it may be abnormally developed(1-4). This abnormality has been described as a fatal condition and is scarcely described in the literature(5). The present case report describes imaging findings of primary acalvaria characterized by the absence of the flat bones of the cranial vault. CASE REPORT A 15-year-old primigravida at 38 weeks' gestation was referred to the authors' institution for specialized prenatal follow-up. Previous ultrasonography performed at the 31st gestational week had identified fetal unilateral hydrocephalus. There was no maternal history of teratogenic medication, recent infection, diabetes mellitus, hypertension or exposure to drugs during the current pregnancy. Cesarean section was indicated. A female neonate was born at term weighting 2815 grams. At clinical examination, the neonate's face was apparently normal, with presence of skin on the frontal region. Cerebral hemispheres prominence and a large defect of the cranial vault were the most obvious findings. The abnormality was characterized by the partial absence of the scalp and o the flat bones of the cranial vault, with a thin membranous layer overlying the brain tissue from which one could observe leakage of cephalorachidian fluid compatible with the pia mater (Figure 1). Frontal and parietal bones could not be palpated. The newborn was referred to the neonatal intensive-care unit where the investigation was pursued.  Figure 1. Clinical examination demonstrates partial absence of the scalp and of the flat bones of the cranial vault. Thin membranous layer overlying the cerebral hemispheres from which leakage of liquor compatible with the pia mater can be observed (arrow). Note the presence of areas with less resistance with exposure of the brain tissue. Immediately after birth, skull radiography demonstrated absence of frontal, parietal and temporal bones, and presence of facial and occipital bones (Figure 2). The findings were confirmed by computed tomography that also demonstrated unilateral ventricular dilatation (Figure 3). Abdominal ultrasonography and echocardiography did not demonstrate any abnormality.  Figure 2. Skull radiography immediately after birth demonstrates absence of the flat bones of the cranial vault. Normal facial bones. 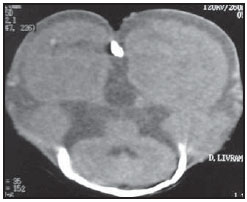 Figure 3. Skull computed tomography performed at the second day of life, confirming both clinical and radiological findings. Preserved occipital bone. The brain remained covered by the pia mater for five days. As a result of the growth process, at the sixth day of life, the brain tissue started breaking-up the thin membrane, becoming completely exposed at the tenth day of life. An attempt to close the bone defect was made with a bovine pericardium patch at the 12th day of life. The reconstruction progressed with a local infectious process and partial suture dehiscence. After two months of life, signs of hypoxic ischemic neurological deterioration could already be observed. After four months of life, transfontanel ultrasonography demonstrated the presence of cystic areas in the brain resulting from hypoxicischemic vascular lesion (Figure 4). The neonate progressed to death at the fifth month of life because of respiratory and infectious complications. 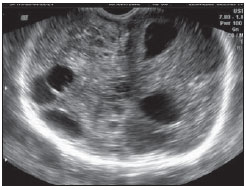 Figure 4. Follow-up brain ultrasonography at the fourth month of life demonstrated cystic areas resulting from hypoxic-ischemic vascular lesion. DISCUSSION Primary acalvaria is a rare congenital malformation characterized by either complete or partial absence of the flat bones of the cranial vault, dura mater and associated muscles, with normal skull base and facial bones. Usually, the defect is covered by skin. The intracranial contents are generally complete, although some abnormalities may be associated(1-7). The etiology and pathogenesis of such abnormality still remain unknown. During the embryonic development, after the anterior neuropore closure around the fourth week migration of the membranous neurocranium occurs under the ectoderm. The condition is said secondary in cases where it is a result of amniotic band syndrome, neural tube defects or use of angiotensin-converting enzyme inhibitors during pregnancy. It is named hypocalvaria in the presence of hypoplastic cranial bones(6). Association with other malformations such as holoprosencephaly, hydrocephalus and micropolygyria, besides other facial, cardiac anomalies, omphaloceles, among others, may be observed(1,6). The rare reports found in the literature suggest a predilection for female fetuses with normal karyotype(7), in agreement with the description of the present case. Presence of skin covering the cranial vault and partial scalp absence were observed. The presence of ectoderm-derived skin and scalp and the absence of cranial vault, dura mater and associated muscle as a result of mesenchymal migration characterize primary acalvaria. In this case, association with an extensive type of aplasia cutis congenita cannot be ruled out. This disorder is characterized by the absence of a portion of skin; most of times (84%) manifesting as a defect on the scalp. The skull is affected in 14% to 30% of cases. Extensive and deep lesions are extremely rare, with a high mortality rate, and may involve the periosteum, the skull and the dura mater(8). REFERENCES 1. Harris CP, Townsend JJ, Carey JC. Acalvaria: a unique congenital anomaly. Am J Med Genet. 1993;46:694-9. 2. Raines C. Primary acalvaria. JDMS. 2006;22: 407-10. 3. Bianca S, Ingegnosi C, Auditore S, et al. Prenatal and postnatal findings of acrania. Arch Gynecol Obstet. 2005;271:256-8. 4. Khadilkar VV, Khadilkar AV, Nimbalkar AA, et al. Acalvaria. Indian Pediatr. 2004;41:618-20. 5. Evans C, Marton T, Rutter S, et al. Cranial vault defects: the description of three cases that illustrate a spectrum of anomalies. Pediatr Dev Pathol. 2009;12:96-102. 6. Barr M, Cohen MM Jr. ACE inhibitor fetopathy and hypocalvaria. The kiney-skull connection. Teratology. 1991;44:485-95. 7. Raupp P, Nork M, Kappel I. Primary acalvaria in a term newborn. J Pediatr. 2002;141:593. 8. Yang JY, Yang WG. Large scalp and skull defect in aplasia cutis congenita. Br J Plast Surg. 2000;53:619-22. 1. Master, Coordinator at Unit of Imaging Diagnosis of the Service of Obstetrics and Gynecology, Hospital Universitário da Universidade Federal do Maranhão (HU-UFMA), São Luís, MA, Brazil 2. PhD, Head of the Service of Obstetrics and Gynecology, Hospital Universitário da Universidade Federal do Maranhão (HU-UFMA), São Luís, MA, Brazil 3. PhD, Head of the Service of Neonatology, Hospital Universitário da Universidade Federal do Maranhão (HU-UFMA), São Luís, MA, Brazil 4. MD, Specialist, Coordinator of the Neonatal ICU, Service of Neonatology, Hospital Universitário da Universidade Federal do Maranhão (HU-UFMA), São Luís, MA, Brazil 5. MD, Specialist at the Neonatal ICU, Service of Neonatology, Hospital Universitário da Universidade Federal do Maranhão (HU-UFMA), São Luís, MA, Brazil 6. Fellow Master degree, MD, Neonatal ICU, Service of Neonatology, Hospital Universitário da Universidade Federal do Maranhão (HU-UFMA), São Luís, MA, Brazil Study developed at Universidade Federal do Maranhão (UFMA), São Luís, MA, Brazil Mailing address: Dra. Lívia Teresa Moreira Rios Avenida do Vale, Ed. Costa Rica, ap. 801, Jardim Renascença 65075-820. São Luís, MA, Brazil E-mail: ltlrios@terra.com.br Received April 17, 2010 Accepted after revision May 24, 2010 |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554