Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 6 - Nov. / Dec. of 2007
Vol. 40 nº 6 - Nov. / Dec. of 2007
|
ORIGINAL ARTICLE
|
|
Value of sonographic endometrial findings in patients under tamoxifen therapy |
|
|
Autho(rs): Arildo Corrêa Teixeira, Linei A.B.D. Urban, Ricardo Salfer Schwarz, Caroline Pereira, Thaís Cristina Cleto Millani, Ana Paula Passos |
|
|
Keywords: Ultrasound, Hysteroscopy, Tamoxifen |
|
|
Abstract:
IProfessor of Gynecology and Obstetrics at Hospital de Clínicas da Universidade Federal do Paraná (UFPR), MD, Ultrasonographist at Clínica DAPI - Diagnóstico Avançado por Imagem, Curitiba, PR, Brazil
INTRODUCTION Tamoxifen has been utilized for almost three decades as an adjuvant treatment for breast cancer, and also is effective in the chemoprophylaxis of this disease. However, this drug presents endometrial proliferation as a side effect, with a low, but real, risk for the development of endometrial cancer(1,2). This risk is of almost two cases of cancer for every 1000 women under tamoxifen therapy during a year, similar to the postmenopausal women submitted to single-dose hormone replacement therapy(2,3). Studies have demonstrated that the majority of cases of endometrial cancers in women under tamoxifen therapy were found at their early stages, and the treatment has been successfully instituted; however, in women who have developed endometrial cancer whose diagnosis was made at later stages, the prognosis has been poorer. Considering these findings, the monitoring of the endometrium of the patients under tamoxifen therapy is recommended aiming at the early diagnosis of these lesions, either by means of ultrasound (US), or hysteroscopy, or uterine curettage, or endometrial biopsy. So, the main objective of the present study was to analyse the main echotextural changes in the endometrium by means of US, in a group of patients under tamoxifen therapy for determining the abnormalities that could occur in the uterine mucosa, besides the correspondent hysteroscopy, and eventually, anatomopathological findings.
MATERIALS AND METHODS The present study retrospectively included 25 patients with breast cancer under tamoxifen therapy referred to the Department of Ultrasound at Hospital das Clínicas da Universidade Federal do Paraná (HC-UFPR) in the period between January 2003 and December 2005, and presenting with endometrial thickening > 5 mm. No patient had undergone hormone replacement therapy or presented gynecologic disease previously to the breast cancer diagnosis. Clinical data evaluated were: age, time of diagnosis, duration of tamoxifen therapy, and presence of symptoms. Transvaginal US was performed with a Sonoline Sienna Ultrasound Imaging System (Siemens, Germany), with a multifrequency 6.5 MHz transducer and color Doppler. The following items were evaluated: endometrial echotexture and endometrial thickness measurement on a longitudinal plane, larger anteroposterior diameter from the echogenic interface at the endometrium-myometrium junction from one side to another. The patients were divided into three groups, according to the thickening degree: thickening between 5-8 mm, 9-15 mm, and above 15 mm. Echotexture was described as homogeneous, heterogeneous with cystic areas, and with an image of a polyp inside. Hysteroscopy was performed with a Storz hysteroscope, with 4.1 mm-diameter, 5.0 mm diagnostic shirt, and a Xenon light source. The uterine cavity distension was accomplished with carbon dioxide (CO2) gas with intrauterine pressure being maintained at a level accepted as safe (between 80 mmHg and 100 mmHg). During the hysteroscopic examination, areas of interest or under suspicion were biopsied. Hysteroscopic findings were described as normal (with no endometrial atypia) or abnormal (endometrial atrophy, cystic atrophy and/or hyperplasia). The analysis of these tissues as performed by pathologists in the Department of Pathological Anatomy at UFPR. The results were considered as normal, provided a regular endometrial maturation was found, or abnormal, in case of atrophy, polyps, simple hyperplasia with or without atypias, fibroids, or endometrial carcinoma.
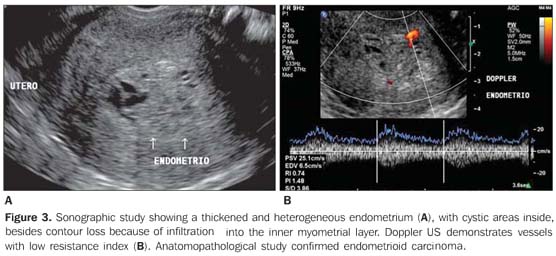
RESULTS The mean age of the 25 patients included in the present study was 62.6 years (age range = 37-77 years). The mean time for the diagnosis of cancer was 4.3 years (ranging between one and 13 years) and mean time under tamoxifen therapy was three years (ranging between one and seven years). All of the patients received a 20 mg/day-dose. Twenty patients were asymptomatic and five presented with bleeding at the moment of examination. Transvaginal ultrasound demonstrated a mean endometrial thickness of 16.4 mm (ranging between 5 mm and 58 mm). Among the patients, 16% (4/25) presented endometrial thickening between 5 mm and 8 mm, 40% (10/25) between 9 mm and 15 mm, and 44% (11/25) > 15 mm. Echotexture was homogeneous in 80% (20/25) of cases, with cystic areas in 16% (4/25) and polyp image in 4% (1/25). Hysteroscopic study performed at last 56 days after the transvaginal US demonstrated 40% (10/25) of cases with atrophy, 16% (4/25) with cystic atrophy, 28% (7/25) with polyp, and 16% (4/25) with hyperplastic lesion. Anatomopathological study was performed in 17 cases. The samples were insufficient in 11.7% (2/17) of cases. In the other cases, with appropriate samples, a normal endometrium was observed in 40% (6/15), atrophy in 6.6% (1/15), polyp in 33.3% (5/15) and hyperplasia in 13.3% (2/15). One case (6.6%; 1/15) of endometrioid adenocarcinoma. The correlation between mean time under tamoxifen therapy and sonographic, hysteroscopic and histological findings is demonstrated on Table 1.
Table 2 correlates clinical data with imaging (US and hysteroscopy) and anatomopathological findings.
Table 3 demonstrates the correlation between sonographic, hysteroscopic and anatomopathological findings.
DISCUSSION Tamoxifen is successfully utilized in the adjuvant therapy of breast cancer, and its effect as a powerful selective estrogen receptor modulator is well established in the literature. On the other hand, tamoxifen effect on other tissues such as the uterus, for example, is more complex, acting simultaneously as a powerful estrogen agonist and antagonist(2,4). The mechanism of action, like the one of other antiestrogenic agents, would be the antagonism to estrogen-specific receptors. It acts competitively binding to estrogen receptors in the tumor-like tissue or other tissues to form a nuclear complex that reduces the DNA synthesis, inhibits the estrogen effects, resulting in an interruption of the cellular growth. However, several authors consider that the tamoxifen mechanism of action is complex and is still to be elucidated(4-6). The presence of hyperestrogenismrelated endometrial disease (polyps, hyperplasia and endometrial carcinoma) in 53.2% of the patients included in the present study confirms, in agreement with the literature, that tamoxifen therapy increases the incidence of endometrial lesion related to the agonist effect of this drug, although most of times there is no progression to cancer(2). A consensus is still to be reached in the literature as regards the association between tamoxifen therapy duration and degree of endometrial lesion(1,3,6). Gerber et al.(3), in a prospective study with 274 women have not found a relation between tamoxifen therapy duration and endometrial thickness. Donne et al.(1) have not observed any relation between therapy duration and degree of endometrial lesion, but the incidence of endometrial cancer was higher in patients exposed to tamoxifen for more than four years. In the present study no relation was found between the presence of endometrial lesion and tamoxifen therapy duration. However, the sole case of carcinoma occurred in a patient who had been using tamoxifen for more than five years, suggesting that the prolonged use of tamoxifen may be related to an increase in the incidence of endometrial cancer. The endometrial involvement secondary to the tamoxifen therapy should be prompt and adequately diagnosed. Ultrasonography constitutes a non-invasive, low-cost imaging method that is well tolerated by the patients, and, when transvaginally performed, can indirectly visualize the uterine cavity. Several authors have described endometrial alterations in breast cancer patients treated with tamoxifen. Zarbo et al.(7), in a prospective study, have reported the follow-up of 219 women with breast cancer and treated with tamoxifen during six years, and described 26.9% prevalence of endometrial alterations represented mainly by polyps and cystic atrophy. In Brazil, Feitosa et al.(6) have observed a 36.6% prevalence of endometrial alterations, 26.6% represented by polyps, and 46% by cystic atrophy. The present study demonstrated 33.3% prevalence of polyps, 13.3% of hyperplasia, and 6.6% of carcinoma.
Among the evaluated sonographic findings, the main abnormalities observed in the present study were endometrial thickness and echotextural alterations. As regards thickness, it is known that the postmenopausal endometrium is shown as a subtle, white and homogeneous line with no more than 5 mm of thickness. Above 5 mm, the higher the thickness, the lower the US accuracy for ruling out the endometrial involvement. That is to say, an endometrial thickness of more than 5 mm does not indicate the presence of endometrial lesion, but rather that an echographic study cannot rule out its presence. Several studies have demonstrated that 40%-54% of patients under tamoxifen therapy present endometrial thickness between 6mm and 10 mm(8,9). Gerber et al.(3) have described a mean thickness of 9.2 mm in a group of tamoxifen users, as compared with 3.5 mm in the control group. However, it should be taken into consideration that many of these cases, actually, represent only an atrophy confirmed by hysteroscopy and anatomopathological study. Aiming at avoiding unnecessary procedures, Gerber et al.(3) have suggested a 10 mm cut-off to determine the necessity of diagnostic deepening in tamoxifen users. On the other hand, Franchi et al.(10) have suggested a 9 mm cut-off, after studying 163 patients both symptomatic and asymptomatic. The authors have divided them into two groups and observed histological alterations in 60% of patients in the group with > 9 mm, while only 6.1% of patients with < 9 mm presented alterations. However, it is important to note that the case of endometrial carcinoma observed in the present study was fund in a symptomatic patient with endometrial thickness of 7 mm, suggesting that symptomatic patients must be investigated, independently from their endometrial thickness. Echotextural findings have an increasing significance in the differentiation between benign and malignant lesions. In postmenopausal patients with no history of hormone replacement therapy, the pattern of atrophy presented at US may mimic a thickened aspect, leading to a great number of false-positive diagnoses, considering that when these women are submitted to hysteroscopy or uterine curettage, they present an endometrial atrophy pattern. The same echotextural endometrial pattern found in association with cystic areas in postmenopausal women, frequently simulating a neoplasm, is observed in tamoxifen users. The apparent increase in the endometrial thickness associated with cystic areas is due to the powerful antiestrogenic effect of tamoxifen on the uterus, causing edema and cystification of endometrial glands, while the overlying epithelium remains atrophic(1,3,11). Cechini et al.(12) have found 41% of cases with echographically abnormal endometrium, 46% of which were false-positive. In our study, 56.6% of tamoxifen users presented endometrial thickening at US, corresponding to atrophy and cystic atrophy at hysteroscopy, also demonstrating a high rate of false-positive results. Additionally, a low accuracy was observed in the identification of hyperplasia and polyps, because the majority of these findings could not be individualized at US. Several studies have emphasized the significance of hysteroscopy in the evaluation of the endometrial cavity with guided-biopsy aiming at a definite diagnosis(1,5). However, this is an invasive and expensive procedure, requiring specialized professionals and equipment. In the present study, hysteroscopy demonstrated high accuracy in the diagnosis of polyps, hyperplasia and neoplastic alterations. The presence of symptoms, such as vaginal bleeding, increases the probability of finding endometrial lesions at imaging studies in tamoxifen users. Deligdisch et al.(2) have found more pathological alteration in the group of symptomatic patients (52% of patients with polyps and 62% with carcinoma presented vaginal bleeding) than in the asymptomatic group. Gerber et al.(3) have described atrophy in 73% of asymptomatic patients, while only 25% of symptomatic patients presented this finding. The present study observed that the presence of symptoms is associated with the presence of lesion at hysteroscopy (all the symptomatic patients presented hyperestrogenism-related lesions characterized by polyps, hyperplasia or adenocarcinoma). However, symptoms absence does not mean absence of lesion, since 41.6% of asymptomatic patients presented polyps or hyperplasia at anatomopathological studies.
CONCLUSIONS Patients who are being treated with tamoxifen require a rigorous endometrial management, because of the increased risk for development of endometrial cancer. Transvaginal ultrasound should be recommended as an initial endometrial screening of breast cancer patients treated with tamoxifen, considering that the disease prognosis is highly dependent on an early diagnosis. In case endometrial alteration suggesting neoplasm is found, hysteroscopy is required for direct visualization of the endometrial cavity as well as a guided-biopsy aimed at a definite diagnosis. The presence of vaginal bleeding increases the risk for endometrial lesion, therefore, anatomopathological study should be performed in all of these cases, independently from the imaging findings. The present study demonstrated that the sole utilization of US in the assessment of these patients and based only on the in crease in the endometrial thickness presents a high rate of false-positive results (56%) leading to unnecessary surgical interventions. However there is a consensus in the literature that cut-offs above 9-10 mm require a more detailed diagnosis. It is important to emphasize the need for an association between clinical symptoms and imaging findings as criteria for establishing the strategy for management of this group of patients.
REFERENCES 1. Le Donne M, Lentini M, De Meo L, Benedetto V, Misiti M. Uterine pathologies in patients undergoing tamoxifen therapy for breast cancer: ultrasonographic, hysteroscopic and histological findings. Eur J Gynaecol Oncol 2005;26:623–626. [ ] 2. Deligdisch L, Kalir T, Cohen CJ, de Latour M, Le Bouedec G, Penault-Llorca F. Endometrial histopathology in 700 patients treated with tamoxifen for breast cancer. Gynecol Oncol 2000;78:181–186. [ ] 3. Gerber B, Krause A, Müller H, et al. Effects of adjuvant tamoxifen on the endometrium in postmenopausal women with breast cancer: a prospective long-term study using transvaginal ultrasound. J Clin Oncol 2000;18:3464–3470. [ ] 4. Fung MFK, Reid A, Faught W, et al. Prospective longitudinal study of ultrasound screening for endometrial abnormalities in women with breast cancer receiving tamoxifen. Gynecol Oncol 2003; 91:154–159. [ ] 5. Fong K, Kung R, Lytwyn A, et al. Endometrial evaluation with transvaginal US and hysterosonography in asymptomatic postmenopausal women with breast cancer receiving tamoxifen. Radiology 2001;220:765–773. [ ] 6. Feitosa FEL, Juaçaba SF, Medeiros FC. Alterações endometriais em pacientes com câncer de mama tratadas com tamoxifeno. RBGO 2002;24: 233–239. [ ] 7. Zarbo G, Caruso G, Zammitti M, Caruso S, Zarbo R. The effects of tamoxifen therapy on the endometrium. Eur J Gynaecol Oncol 2000;21:86–88. [ ] 8. Suh-Burgmann EJ, Goodman A. Surveillance for endometrial cancer in women receiving tamoxifen. Ann Intern Med 1999;131:127–135. [ ] 9. Marconi D, Exacoustos C, Cangi B, et al. Transvaginal sonographic and hysteroscopic findings in postmenopausal women receiving tamoxifen. J Am Assoc Gynecol Laparosc 1997;4:331–339. [ ] 10. Franchi M, Ghezzi F, Donadello N, Zanaboni F, Beretta P, Bolis P. Endometrial thickness in tamoxifen-treated patients: an independent predictor of endometrial disease. Obstet Gynecol 1999;93:1004–1008. [ ] 11. Seoud M, Shamseddine A, Khalil A, et al. Tamoxifen and endometrial pathologies: a prospective study. Gynecol Oncol 1999;75:15–19. [ ] 12. Cecchini S, Ciatto S, Bonardi R, et al. Risk of endometrial cancer in breast cancer patients under long-term adjuvant treatment with tamoxifen. Tumori 1998;84:21–23. [ ]
Received February 22, 2007. Accepted after revision April 10, 2007.
* Study developed in the Department of Echography, Maternidade do Hospital de Clínicas da Universidade Federal do Paraná (UFPR), and Clínica DAPI - Diagnóstico Avançado por Imagem, Curitiba, PR, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554