Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 4 - July / Aug. of 2007
Vol. 40 nº 4 - July / Aug. of 2007
|
CASE REPORT
|
|
Focal nodular hyperplasia of the liver: a case report and review of the literature |
|
|
Autho(rs): Marise Silva Teixeira, Francisca Teresa Veneziano Faleiros, Beatriz Lotufo Griva, Yoshio Kiy, Sonia Maria Moriguchi, Altamir Santos Teixeira, Bonifácio Kategawa, Kunie Iabuki Rabello Coelho, Cláudio Antonio Rabello Coelho |
|
|
Keywords: Focal nodular hyperplasia, Scintigraphy, Computed tomography, Ultrasonography |
|
|
Abstract:
IMD at Department of Pediatrics, Faculdade de Medicina de Botucatu – Universidade Estadual Paulista Júlio de Mesquita Filho (Unesp), Botucatu, SP, Brazil
INTRODUCTION Focal nodular hyperplasia (FNH) is the second most frequentbenign tumor of the liver, surpassed in prevalence only byhepatic hemangiomas, and corresponding to 8% of all the primaryhepatic tumors(1). Most of times, FNH is foundas a solitary nodule smaller than 5 cm in diameter, althoughlarger lesions with more than 15 cm in diameter have already beenfound(1). Usually, the course of the disease isasymptomatic, and, most of times, the lesion is incidentallyfound either at a clinical examination, as an imaging finding, orduring autopsy(2). Macroscopically, FNHpresents as a well circumscribed, lobulated and non-encapsulatedlesion(3). Typical histological alterationsinclude a dense, central star-like scar with radiating fibroussepta dividing the tumor into severalnodules(3). Microscopically, these fibroussepta are composed of biliary structures surrounded byinflammatory cells, Kupffer cells and vascular malformationsincluding arteries and capillaries(3). Developments in imaging studies have made the diagnosis easierwithout necessity of laparotomy or surgical, besides thedifferentiation between FNH and other benign diseases of theliver and hepatocellular carcinoma(2).
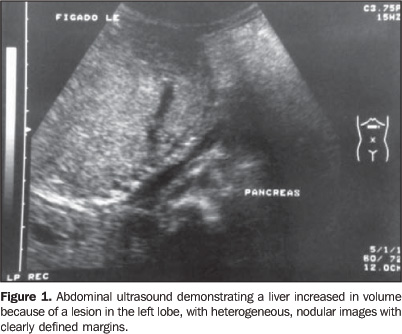
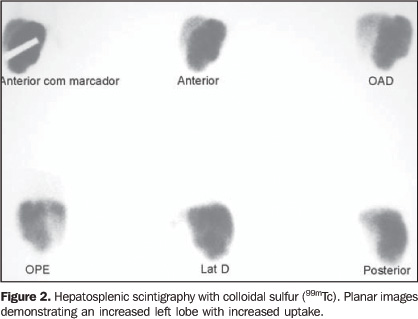
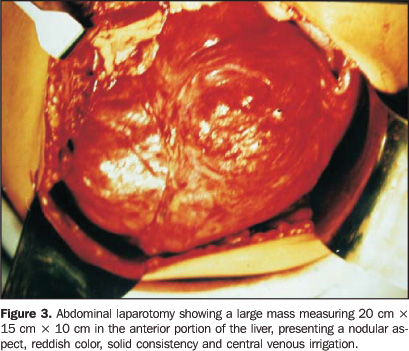
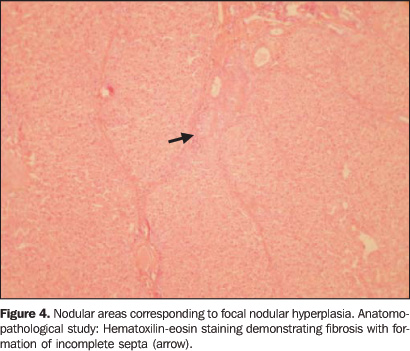
CASE REPORT The present study reports the case of a black, female,19-year-old patient who, at six year of age, had presentedcomplaining of mesogastric pain and abdominal distention.Clinically, the patient presented a good general condition,flushed and hydrated. Weight and height were near the 25thpercentile, according to her chronological age (weight: 20.4 kg,height: 116 cm). The liver was palpable at 6.5 cm from the rightcostal border, and at 11.5 cm from the xiphoid appendix,painless, with an irregular surface and hardened consistency.Liver function tests were normal. Ultrasound evidenced hepatomegaly with lobulated margins (Figure 1). Hepatosplenic scintigraphy was suggestive of FNH, since it has shown the left lobule increased in volume and with increased uptake (Figure 2). Laparotomy has evidenced a large mass measuring 20 cm × 15 cm × 10 cm in the anterior portion of the liver, presenting a nodular aspect, reddish color, solid consistency and central venous irrigation, suggesting a tumor-like process (Figure 3). Open biopsy was performed, confirming the diagnosis suggested by the hepatosplenic scintigraphy (Figure 4). These studies were performed at the time of the diagnosis.
Along these 13 years of follow-up, a conservative approach has been adopted, and the progression has shown hepatic enlargement documented by abdominal ultrasound. Hepatosplenic scintigraphy has evidenced increase of the left lobe with heterogeneously decreased radionuclide uptake. Biliary tract scintigraphy has shown a hyperconcentrating left lobe, with a more heterogeneous aspect. Abdominal helical computed tomography, performed at 16 years of age, also demonstrated findings suggestive of FNH (Figure 5).
DISCUSSION Developments in imaging techniques have contributed to theincrease in the number of diagnosis of benign hepatic tumors, thedifferential diagnosis between FNH and hepatic adenoma beingextremely important in the clinical practice, considering therisk of rupture and bleeding of hepaticadenomas(1). The apparent increase in theincidence of FNH starting in 1960, although coinciding with thetime where oral contraceptives were made available in the UnitedStates, may be just a result of the development of imagingdiagnosis techniques and the improvement in the quality ofultrasound studies(4,5). The FNH pathogenesis is still to be defined, despite a studyreporting a simultaneous occurrence of hemangioma, FNH andhepatic adenoma, suggesting that these three lesions aredifferent manifestations of a samemalformation(6). A pre-existing vascularanomaly could cause a local hyperplastic response ofhepatocytes(7). The possible role of sexualhormones, including oral contraceptives, in the FNH developmenthas been suggested due to the higher prevalence in women (80% to95% of cases)(8) and potential spontaneousregression of the FNH as a result of an interruption in the useof oral contraceptives(10). However, theassumption that a FNH may not be associated with the use of oralcontraceptives is evidenced by the occurrence of this type oflesion even before the introduction of oral contraceptives, andby the presence of FNH in children, men and women who have neverutilized them(5,8). Actually, the use of oralcontraceptives may be associated with the development of FNH,even accelerating its growth, but their possible implication inthe occurrence of this lesion has not beendemonstrated(3,8). Nevertheless, new studiesare necessary to clarify the role of oral contraceptives in theoccurrence of FNH(2). The definition of the type of lesion is essential, and, amongthe lesions more easily confused with FNH, hepatic adenoma shouldbe highlighted because of its unequivocal relationship with theuse of oral contraceptives, especially in high doses and duringlong periods of time(2). In contrast to theusually conservative approach adopted for FNH, in case of hepaticadenoma a surgical excision is performed because of the risk ofbleeding and, mainly, malignization(2). Incases of FNH surgical intervention is reserved for those whichpresent with symptoms, complications, progressive lesions oradjacent organs compression(2,9). FNH complications such as abdominal discomfort, intratumoralhemorrhage and intraperitoneal rupture are rare, although somecases of intraperitoneal rupture have been described in theliterature and, in this circumstance the surgical approach havebeen necessary(10,11). Potential malignant transformation of FNH has not beenreported, although FNH coexistence with hepatocellular carcinomahas rarely been described(8). The following non-invasive diagnostic techniques areincreasingly utilized(3,8,12): a) ultrasound;b) computed tomography, allowing high accuracy in thedifferentiation between the most frequent types of centrallyscarred hepatic tumors, including FNH, fibrolamellarhepatocelullar carcinoma and giant cavernous hemangioma; c)hepatosplenic scintigraphy; d) magnetic resonance imaging. Anuseful finding in the diagnosis of FNH is the evidence ofincrease in the hepatic uptake at hepatosplenic scintigraphy,allowing the differential diagnosis with other hepatic masses.Ultrasound, computed tomography and magnetic resonance imagingmay demonstrate benign hepatic masses, with typical, although notuniversal, the presence of a central scar. Although lessfrequently, a characteristic radiating hypervascular malformationmay be found(3). Notwithstanding the great usefulness of imaging techniques forthe diagnosis of this tumor, if doubts persists about thediagnosis, a hepatic biopsy becomes mandatory, considering itssignificance as a highly specific diagnosticmethod(3).
REFERENCES 1. Biecker E, Fischer HP, Strunk H, Sauerbruch T. Benign hepatic tumours. Z Gastroenterol 2003; 41:191–200. [ ] 2. Choi BY, Nguyen MH. The diagnosis and management of benign hepatic tumors. J Clin Gastroenterol 2005;39:401–412. [ ] 3. Kehagias D, Moulopoulos L, Antoniou A, et al. Focal nodular hyperplasia: imaging findings. Eur Radiol 2001;11:202–212. [ ] 4. Cherqui D, Rahmouni A, Charlotte F, et al. Management of focal nodular hyperplasia and hepatocellular adenoma in young women: a series of 41 patients with clinical, radiological, and pathological correlations. Hepatology 1995;22:1674–1681. [ ] 5. Kerlin P, Davis GL, McGill DB, Weiland LH, Adson MA, Sheedy PF. Hepatic adenoma and focal nodular hyperplasia: clinical, pathologic, and radiologic features. Gastroenterology 1983; 84(5 Pt 1):994–1002. [ ] 6. Di Carlo I, Urrico GS, Ursino V, Russello D, Puleo S, Latteri F. Simultaneous occurrence of adenoma, focal nodular hyperplasia, and hemangioma of the liver: are they derived from a common origin? J Gastroenterol Hepatol 2003;18: 227–230. [ ] 7. Ohmoto K, Honda T, Hirokawa M, et al. Spontaneous regression of focal nodular hyperplasia of the liver. J Gastroenterol 2002;37:849–853. [ ] 8. Vilgrain V. Focal nodular hyperplasia. Eur J Radiol 2006;58:236–245. [ ] 9. Okada T, Sasaki F, Kamiyama T, et al. Management and algorithm for focal nodular hyperplasia of the liver in children. Eur J Pediatr Surg 2006;16:235–240. [ ] 10. Koch N, Gintzburger D, Seelentag W, Denys A, Gillet M, Halkic N. Rupture of hepatic focal nodular hyperplasia. About two cases. Ann Chir 2006;131:279–282. [ ] 11. Demarco MP, Shen P, Bradley RF, Levine EA. Intraperitoneal hemorrhage in a patient with hepatic focal nodular hyperplasia. Am Surg 2006; 72:555–559. [ ] 12. Machado MM, Rosa ACF, Herman P, et al. Avaliação dos tumores hepáticos ao Doppler. Radiol Bras 2004;37:371–376. [ ]
Received January 12, 2006. Accepted after revision November 11, 2006.
* Study developed at Hospital das Clínicas de Botucatu – Universidade Estadual Paulista Júlio de Mesquita Filho (Unesp), Botucatu, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554