Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 4 - July / Aug. of 2007
Vol. 40 nº 4 - July / Aug. of 2007
|
REVIEW ARTICLE
|
|
Evaluation of the lacrimal system by radiological methods |
|
|
Autho(rs): Fabiano Celli Francisco, Antonio Carlos Pires Carvalho, Gilberto Torres Neto, Vivian Frida Murta Francisco, Luis Alberto Moreira de Souza, Marina Celli Francisco, Lea Mirian Barbosa da Fonseca, Bianca Gutfilen, Adhemar Azevedo de Mendonça Júnior |
|
|
Keywords: Dacryocystography, Lacrimal system, Obstruction of the lacrimal system |
|
|
Abstract:
IPhysician Assistant at Clínica Radiológica Emílio Amorim, Fellow Master Degree at Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil
INTRODUCTION The main indication for the evaluation of the lacrimalpathways is epiphora which is the excessive tearing of anyetiology. It may originate in the excessive tear production,resulting in inadequate evaporation and drainage due to the largevolume of tears. Another even more common situation is epiphoracaused by the inefficient tears drainage secondary to the partialor complete obstruction of the lacrimalsystem(1,2). Other processes requiring radiological investigation arediverticula, fistulas, peri- or intraluminal masses andobstruction secondary to surgicalintervention(3). Imaging study of the lacrimal system in patients with epiphoraallows the diagnosis of lacrimal obstructions and their possiblecomplications and, from the therapeutic point of view, isrelevant, since it provides safer information for indicating thesurgery and the type of procedure to beperformed(4). The aims of the present study are to demonstrate imagingmethods available for assessment of the lacrimal pathways and thereasoning of the imaging study which we consider as the method ofchoice.
ANATOMY OF THE LACRIMAL PATHWAYS Each lacrimal drainage system is formed by lower and upper lacrimal canaliculi, common canaliculus, lacrimal sac, and nasolacrimal duct. The tear penetrates the lacrimal pathway through the lower and upper lacrimal ostia (lacrimal point), minute orifices (0.3 mm in diameter) seen on the medial margin of the lower and upper eyelids(5) (Figure 1).
The lower and upper lacrimal canaliculi present a verticalportion measuring 2 mm, and a horizontal portion measuring about8 mm. As the horizontal portion meets the vertical one, itsinternal diameter increases, achieving 2mm(2,6). The junction of the lower and upper lacrimal canaliculi occursin 90% of patients, constituting the common canaliculus, alsotermed Maier's sinus or ampulla of lacrimal canaliculus. In theother 10%, the canaliculi connect the lacrimal sac independently.The Maier's sinus meets the lateral wall of the lacrimal sac atthe level of the junction between the upper and middle thirds.This opening is guarded by a fold of mucous membrane calledRosenmüller's valve(2,6). Some authorsquestion the existence of this valve, arguing that it is just anangulation of about 58º formed by the junction between thecommon canaliculus and the lacrimal sac(5). The lacrimal sac is lodged in a deep groove formed by thelacrimal bone. It is the wider portion of the lacrimal pathwayand measures about 4–8 mm in anteroposterior diameter, 1–2 mmtransversally, and 10–12 mm in length. At its distal end there isa fold of mucous membrane denominated Krause's valve. Below thisvalve, the lacrimal pathway continues as the nasolacrimal ductthrough an extent of 12–18 mm (10 mm through the bonenasolacrimal canal), up to the inferior nasal meatus. In themiddle of the intra-osseous portion of the nasolacrimal ductthere is a fold of mucous membrane called Taillefer's valve, and,at the end of the duct, the Hasner'svalve(6,7).
LACRIMAL PATHWAYS EVALUATION The first contrast-enhanced radiographs of the lacrimalpathways were performed by Ewing in 1909(8),utilizing a bismuth subnitrate solution, aiming at demonstratinga lacrimal abscess. Currently, the lacrimal pathways study is divided intofunctional and anatomical evaluations. The functional evaluationis performed by means of staining tests, scintigraphy andmagnetic resonance imaging. The anatomical evaluation isperformed by means of dacryocystography with conventionalradiographs, linear computed tomography and magnetic resonanceimaging(1). Dacryocystography Dacryocystography demonstrates the lacrimal pathways by meansof radiography after contrast agentinjection(1). Currently, oil-soluble andwater-soluble contrast media are available. The oil-solublecontrast media are more slowly eliminated, however they tend toobstruct the lacrimal ducts, particularly if they present withsome alteration. Also, they may cause a false appearancepolycystic sac, since the oil is poorly miscible with thelacrimal secretion(9). Oil-soluble contrastmedia should not be utilized in the suspicion of tumors,traumatism or fistulae, considering the risk of leakage andpermanence in the subcutaneous tissue for many years, inducingthe formation of granulomas(10). Other studies report that the use of water-soluble contrastmedia result in more real information because of itscharacteristics (pH and viscosity, for example) more similar totears. In a normal lacrimal pathway, the contrast mediumcompletely disappears after ten minutes. Contrast medium tracesmay be found only in the nasopharinx(9,11). Initially, the patient is submitted to panoramic radiography of the face. Anesthetic eye drops are instilled, lacrimal canaliculi are characterized and, after contrast medium administration, radiographic images acquisition is performed (Figure 2). Additional views, with different degrees of obliquity may be obtained to demonstrate the lacrimal pathways.
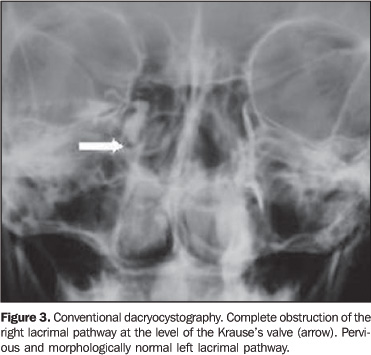
Although this study is inexpensive and easy to perform, with low radiation dose, and allowing the identification of the site of obstruction, presence or not of lacrimal pathways dilatation and some alteration of adjacent structures, dacryocystography may present some inconclusive results(1) (Figure 3).
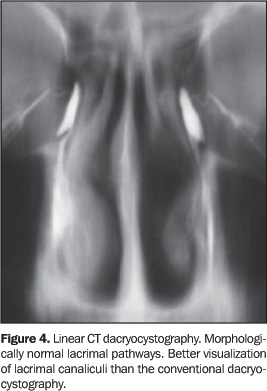
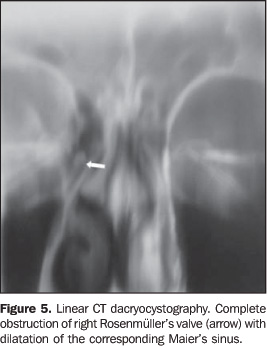
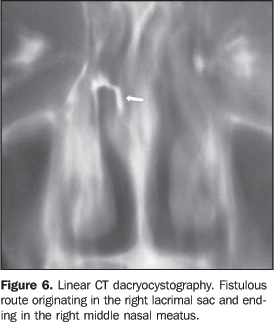
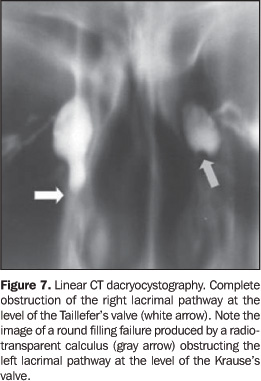
Linear tomography-dacryocystography The demonstration of the lacrimal pathways also may beperformed by means of linear tomography. The technique is very similar to the conventionaldacryocystography, starting with facial radiographs andinstillation of anesthetic eye drops. Lacrimal canaliculi arecharacterized and the patient's head is fixed. After collimationrestricted to the area of interest, the watersoluble contrastmedium is administered and, simultaneously, the acquisition oflinear tomographic images is performed. Generally, four imagesare sufficient to demonstrate the lacrimal pathways. Thewater-soluble contrast medium is chosen for the already mentionedreasons. Some authors(9,12) recommend a bilateralevaluation to allow the comparison with the contralateral pathwayand mainly for detecting asymptomatic alterations. We agree withthis technique, since in experienced hands, the cannulation oflacrimal canaliculi is very fast and painless, besides allowingan early diagnosis in a significant number of cases, avoiding anew exposure of the patient to ionizing radiation and additionalonus. All the patients will benefit from the comparison with thecontralateral pathway, a significant factor in some diagnosticcircumstances. With this technique, Takano &Mendonça(9) have found alterations in8.3% of asymptomatic contralateral lacrimal pathways. Linear tomography-dacryocystography is inexpensive and easy to perform in comparison with the most recent methods and with lower radiation dose than computed tomography. This method allows demonstrating lacrimal canaliculi (Figure 4), the site of obstruction, lacrimal pathways dilatation (Figure 5), fistulae (Figure 6), lacrimal calculi (Figure 7), a higher number of alterations in adjacent structures than the conventional dacryocystography and, in experienced hands, does not present inconclusive results and complications.
This method does not present metal or paramagnetic artifacts (Figure 8). Computed tomography dacryocystography Computed tomography dacryocystography allows the documentationnot only of lacrimal pathways, but also of adjacent bones andsoft tissues(13). Anesthetic eye drops are instilled with the patient supine. The lacrimal canaliculi are cannulated, and the patient´s head is fixed. Acquisition of helical axial images is performed simultaneously with the injection of water-soluble contrast medium. This set of images may be three-dimensionally reconstructed (Figures 9 and 10), facilitating the images interpretation by other specialists accustomed to interpreting coronal images. The comparison with the previous methods demonstrates that CTdacryocystography is a very expensive method, demanding a highradiation dose, although is extremely useful in the diagnosis oflacrimal pathways obstruction associated with intranasaldiseases, facial fractures and maxillofacialtumors(14,15). MRI dacryocystography Many authors have described MRI applications in the evaluationof lacrimal pathways. MRI is the method of choice for evaluationof the orbit, since it provides best images of soft tissues. Theadministration of diluted gadolinium may be performed asfollows: 1 – Eyedrops may be instilled into the conjunctival sac of each eye. This is a non-invasive method, allowing a functional evaluation of the lacrimal pathways(16) (Figure 11). 2 – Another alternative is the lacrimal canaliculi catheterization, followed by diluted gadolinium administration (Figure 12). The catheters are removed and coronal, T1-weighted images are acquired. Some authors suggest acquisition of coronal T1- and T2-weighted images with fat-suppression, both before and after contrast medium administration(17). Some studies report that CT and MRI sensitivity issimilar(16,17). Although MRI is a moreexpensive method, it does not utilize ionizing radiation,allowing acquisition of 3D images, and providing additionalinformation on adjacent soft tissues. Therefore it may be addedto the protocol for study of lacrimalpathways(18).
CONCLUSIONS The lacrimal system evaluation may be performed by means ofseveral imaging methods. It is up to the physician to choose themost appropriate imaging method, avoiding the delay between thedefinite diagnosis and the treatment. As an example of firstchoice, the authors suggest linear CT dacryocystography, leavingthe more expensive and less available methods for patients withproblems of lacrimal pathways associated with previous history offacial traumas, tumors in the medial portion of the face,intranasal diseases or maxillofacial surgery.
REFERENCES 1. Schellini SA, Hercules LA, Padovani CR, Nascimento SM, Lopes PS, Schellini RC. Dacriocistografia na propedêutica da via lacrimal excretora de adultos. Arq Bras Oftalmol 2005;68:89–92. [ ] 2. Schatz CS. Dacryocystography. In: Bergeron RT, Osborn AG, Som PM, editors. Head and neck imaging. 1st ed. St. Louis, MO: CV Mosby, 1984; 669–680. [ ] 3. Watkins LM, Janfaza P, Rubin PAD. The evolution of endonasal dacryocystorhinostomy. Surv Ophthalmol 2003;48:73–84. [ ] 4. Amin M, Moseley IF, Rose GE. The value of intubation dacryocystography after dacryocystorhinostomy. Br J Radiol 2000;73:604–607. [ ] 5. Linberg JV, Moore CA. Symptoms of canalicular obstruction. Ophthalmology 1988;95:1077–1079. [ ] 6. Clark R. Aparato lacrimal. In: González CF, Becker MH, Flanagan JC, editors. Diagnostico por la imagen en oftalmología. Barcelona: Ediciones Doyma, 1988;77–87. [ ] 7. Tucker SM, Linberg JV, Nguyen LL, Viti AJ, Tucker WJ. Measurement of the resistance to fluid flow within the lacrimal outflow system. Ophthalmology 1995;102:1639–1645. [ ] 8. Ewing AE. Roentgen ray demonstrations of the lacrimal abcess cavity. Am J Ophthalmol 1909; 24:1–4. [ ] 9. Takano BA, Mendonça-Júnior AA. Dacriocistografia: aspectos radiológicos nas alterações das vias lacrimais – análise de 24 casos. Radiol Bras 1996;29:23–29. [ ] 10. Munk PL, Burhenne LW, Buffam FV, Nugent RA, Lin DT. Dacryocystography: comparison of water-soluble and oil-based contrast agents. Radiology 1989;173:827–830. [ ] 11. Patrão ALS. Dacriocistografia. Rev Bras Oftalmol 1983;XLII:68–72. [ ] 12. Silva JAF, Kambara A. Dacriocistografia sob injeção contínua. Arq Bras Oftalmol 1980;43:183–187. [ ] 13. Moran CC, Buckwalter K, Caldemeyer KS, Smith RR. Helical CT with topical water-soluble contrast media for imaging of the lacrimal drainage apparatus. AJR Am J Roentgenol 1995;164:995–996. [ ] 14. Saraç K, Hepsen IF, Bayramlar H, Uguralp M, Toksoz M, Baysal T. Computed tomography dacryocystography. Eur J Radiol 1995;19:128–131. [ ] 15. Waite DW, Whittet HB, Shun-Shin GA. Technical note: computed tomographic dacryocystography. Br J Radiol 1993;66:711–713. [ ] 16. Karagulle T, Erden A, Erden I, Zilelioglu G. Nasolacrimal system: evaluation with gadolinium-enhanced MR dacryocystography with a three-dimensional fast spoiled gradient-recalled technique. Eur Radiol 2002;12:2343–2348. [ ] 17. Manfrè L, DeMaria M, Todaro E, Mangiameli A, Ponte F, Lagalla R. MR dacryocystography: comparison with dacryocystography and CT dacryocystography. AJNR Am J Neuroradiol 2000;21: 1145–1150. [ ] 18. Kirchhof K, Hähnel S, Jansen O, Zake S, Sartor K. Gadolinium-enhanced magnetic resonance dacryocystography in patients with epiphora. J Comput Assist Tomogr 2000;24:327–331. [ ]
Received June 15, 2005. Accepted after revision August 3, 2005.
* Study developed at Clínica Radiológica Emílio Amorim and Department of Radiology, Faculdade de Medicina da Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554