Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 4 - July / Aug. of 2007
Vol. 40 nº 4 - July / Aug. of 2007
|
ORIGINAL ARTICLE
|
|
Quantitative evaluation of lateral forces on the patella: static and kinematic magnetic resonance imaging |
|
|
Autho(rs): Je Hoon Yang, Guilherme Tadeu Sauaia Demarchi, Emerson Garms, Yara Juliano, Luiz Aurélio Mestriner, Moises Cohen, Ricardo Dizioli Navarro, Artur da Rocha Corrêa Fernandes |
|
|
Keywords: Knee, Knee joint, Patella, Patellofemoral pain syndrome, Magnetic resonance imaging, Biomechanics, Chondromalacia patellae |
|
|
Abstract:
IMaster in Clinical Radiology, MD, Collaborator, Department of Imaging Diagnosis, Universidade Federal de São Paulo-Escola Paulista de Medicina (Unifesp-EPM), São Paulo, SP, Brazil
INTRODUCTION Anterior knee pain is a frequent complaint in the dailypractice of orthopedists, especially from the young femalepopulation. Most frequently, femoropatellar instability isconsidered as the number-one cause of anterior kneepain(1–3). Biomechanical evidence shows thatthe last 30° of extension are critical within the full rangein the femoropatellar joint dynamics. Lateral forces on thepatella at this angle are higher, and so is the risk forsubluxation(4). Since 1941, when Wibergdeveloped the anatomical classification of the patella, severalradiographic techniques for evaluating the femoropatellar jointat flexion angles 20° and 45° have beendescribed(5–7). The axial view of the patellaat up to 30° flexion is difficult to perform, but many of thetroublesome aspects only could be overcome by utilizing computedtomography (CT) and magnetic resonance imaging(MRI)(8,9). Still, these techniques do notallow the evaluation of the femoropatellar joint with activequadriceps contraction and therefore many biomechanical aspectsof the femoropatellar joint still remain to be appropriatelystudied. Kinematic MRI has recently emerged as a highly sensitivemethod to determine the presence of lateral displacement of thepatella(10,11) ultimately supplying clinicallysignificant information concerning femoropatellar jointdynamics. To date, there is no report in the literature regarding thedetermination of the critical range of flexion concerningfemoropatellar joint functional forces by means ofcross-sectional tomographic images. The present study was aimed at evaluating the validity ofcombining static and kinematic MRI in the dynamic study of thefemoropatellar joint during active quadriceps contraction,correlating the resulting data with biomechanical fundamentalsreported in the literature.
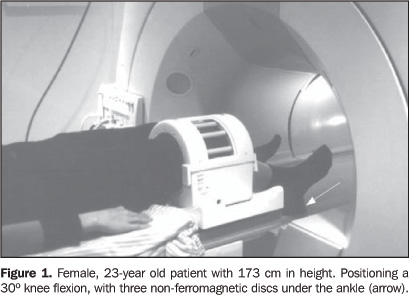
MATERIALS AND METHODS Study population Transversal study developed in the period betweenNovember/2001 and March/2003, evaluating 20 healthy volunteers(40 knees) and 25 patients (43 knees). The study was conducted incompliance with the Declaration of Helsinki VI (Edinburgh,October/2000) and under the approval of the Committee for Ethicin Research of Universidade Federal de São Paulo. Writtenfree informed consent was obtained from all the participatingindividuals. Asymptomatic volunteers: 10 men (20 knees), aged 28.7 ±4.6 years (mean ± 1 standard deviation [SD]); and 10 women(20 knees), aged 28.4 ± 4.7 years (mean ± 1 SD) whohad never visited a physician for knee-related complaints. Thosewho presented with a history of previous surgery or traumainvolving the femoropatellar joint were excluded. Also, thosewith a ventral trochlear prominence on sagittal MRI referenceimages were excluded, considering that these factors constitutelandmarks indicating higher risk for femoropatellarinstability(12). The selection of patients was performed by specializedorthopedists among patients referred to our institution.Twenty-five consecutive patients (43 knees) presenting withfemoropatellar instability were selected. The sample includedeight knees in five male patients [age 25 ± 1.6 years(mean ± 1 SD)] and 35 knees in 18 female patients [age21.6 ± 6.4 years (mean ± 1 SD)]. Physicalexamination demonstrated lateral hypermobility of the patella;increased lateralization of the patella during extension;positive apprehension test. All the female patients, oneexcepted, presented clinically with bilateral, not necessarilysymmetrical, femoropatellar instability. Patients presenting witha history of acute traumatic dislocation or habitual dislocationof the patella, as well as those with a history of surgery in theknee, were excluded. Q-angle was not an inclusion criterion,considering the possibility of false-negative values in cases swere not included in the selection criteria because such valuescould become falsely reduced in cases of patellarposition-related abnormalities and valgism of extensormechanisms(13). Positioning All of the volunteers and patients underwent both static andkinematic MRI in a 1.5 T whole-body MRI scanner (15 mT/m gradientstrength) (Gyroscan ACS NT 15, Powertrak 1000; Philips MedicalSystem, Best, Netherlands). The knees were positioned at 30º flexion with the quadrature knee coil at the inner end of the examination table. Aiming at allowing this flexion arc, the knee was positioned at a height of 18 cm (coil base = 5 cm + foam cushion under the coil = 3 cm + examination table thickness = 10 cm). Lateral, but not rotatory, motion was restrained by the coil. Palpable external anatomical landmarks were adopted as reference points: the most prominent point of the greater trochanter; the lateral femorotibial joint space, a point located cranial and anteriorly to the fibular head; and the anterior margin of the tibial diaphysis. From these points two imaginary lines were determined: one between the greater trochanter and the lateral femorotibial joint space, and another parallel to the anterior margin of the tibial diaphysis. A universal 360° goniometer was positioned on the intersection between these two lines, and the intersection angle was considered as the knee flexion angle. Non-ferromagnetic, 1 cm-thick discs were placed under the ankle so that 30°, 20º, 10° flexion and full extension were achieved. After that, the examination table was inserted into the magnet bore (Figure 1).
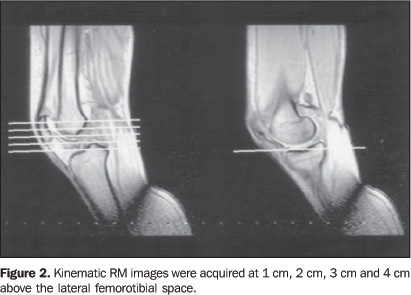
Images acquisition Before static and kinematic MR images acquisition, effectiveknee flexion angles were measured on referential sagittal MRimages, at the intersection between the greater axis of the femurand the anterior margin of the tibia. Images acquisitionproceeded, provided the results of this measurement were between26° and 34°. Static MRI involved acquisition of sections at 30°,20°, 10° flexion and at full extension. The number ofdiscs under the ankles required to achieve these flexion degreeswas determined as previously described. Axial, spin-echoT1-weighted sequences were performed with repetition time(RT)/echo time (ET) 457/13 ms; rectangular field-of-view (FOV),90%; 256 × 160 image matrix on a 160 × 144 mm FOV;number of sections 19; section thickness/gap, 4.5/0.5 mm. Kinematic MRI involved acquisitions at 1 cm, 2 cm, 3 cm, and 4 cm up from the lateral femorotibial joint space. The option for the lateral space took into consideration the lower curvature in relation to the medial femorotibial joint space (Figure 2)(14). A turbo spin-echo sequence was performed with RT/ET 325/79 ms; rectangular FOV, 70%; 128 × 80 image matrix; 160 × 112 mm FOV; turbo factor, 24; section thickness, 8 mm. These parameters associated with a partial k-space reconstruction algorithm allowed an image to be obtained every 525 ms without motion artifacts. The individuals were given instructions to extend the knees from 30° flexion to full extension, starting and finishing according to the gradient switching noise. These movements were practiced before the effective images acquisition. The single-slice- multiphase technique generated eight sequential axial images in 4.2 seconds. Imaging was considered as satisfactory if uniform extension was achieved in all of the four planes. The entire process of a knee examination, including patients positioning, instructions, test runs, static and kinematic MRI, took about 25 minutes.
Images evaluation Each knee received an identification number and was separatelyevaluated. Exact flexion angles could not be directly determined in the kinematic MRI, so "flexion sectors" instead of flexion degrees were adopted as reference. The 30° flexion range was divided into eight sectors (I to VIII), and each kinematic MRI frame was classified according to the estimated flexion range (Table 1).
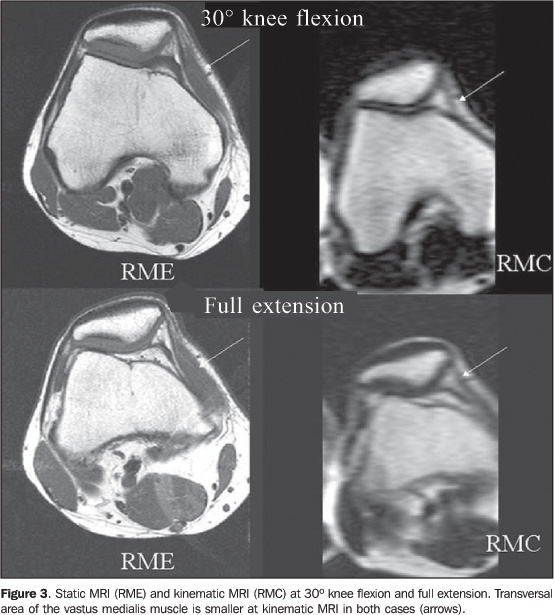
The images corresponding to the same flexion sector in fourkinematic MRI acquisitions were compared with the correspondingstatic MR images. The transversal area of the vastus medialis muscle was adopted as a parameter indicating the presence of quadriceps contracture at kinematic MRI. Static RM images at 30º flexion were compared with those from the sector I of kinematic MRI, and the static MR images at full extension, with those from the sector VIII of kinematic MRI. This comparison was made between images acquired from the corresponding distances from the lateral femorotibial joint space (Figure 3). A transversal area of the vastus medialis muscle at kinematic MRI smaller than that at static MRI constituted an indication of the presence of quadriceps contraction.
Quantitative analysis Bisect offset (BSO), lateral patellar displacement (LPD) and patellar tilt angle (PTA) were measured both on static and kinematic MRI(15) (Figure 4).
Two images from a same flexion degree (static MRI) or from asame flexion sector (kinematic MRI), acquired at 1 cm, 2 cm, 3cm, and 4 cm up from the lateral femorotibial joint space, wereselected for measurements: one demonstrating the largesttransversal area of the patella, and the other, the mostrepresentative image of the intercondylar groove. Referencepoints were superposed utilizing the above mentioned parameters,according to Brossmann et al.(15). Data from asymptomatic volunteers and patients on both static and kinematic MRI were compared independently for each of the three parameters, and separately for each group of individuals (asymptomatic volunteers and patients) (Table 2). Considering that the static MRI presents four fixed flexion degrees, and the kinematic MRI, eight flexion sectors, the comparison was made as per Table 2.
A "delta" was defined, corresponding to the difference between parameters resulting from static and kinematic MRI. The values resulted from an arithmetical subtraction of variables for each parameter and for each individual (asymptomatic volunteers and patients). The results of this arithmetical subtraction for each parameter (BSO, LPD and PTA) were named BSO-delta, LPD-delta and PTA-delta for all the acquisitions at 30°, 20°, 10° and full extension of each knee. Flexion degrees and flexion sectors were combined (Table 2). Statistical analysis Considering the nature of the variables studied,non-parametric tests were utilized for statistical analysis. 1. Asymptomatic volunteers versus patients –Non-parametric Mann-Whitney test for both static and kinematicMRI data. 2. Static versus kinematic MRI – Non-parametricWilcoxon signed rank test for asymptomatic volunteers andpatients, separately evaluated. 3. Asymptomatic volunteers versus patients fordelta-parameters – Non-parametric MannWhitney test Null hypothesis rejection level = 0.05 or 5% (statisticalsignificance = p < 0.05). Significant z andp values are marked with an asterisk.
RESULTS Asymptomatic volunteers versus patients Statistically significant differences (p < 0.05)were found between measurements in asymptomatic volunteers andpatients for the three parameters, both by static and kinematicMRI, at 30° flexion up to full extension. Static MRI versus kinematic MRI Asymptomatic volunteers – Differences found betweenstatic and kinematic MRI measurements were statisticallysignificant for BSO and LPD at 20° and 10° flexion. ForPTA, statistically significant differences were found at 30°and 20° flexion (p < 0.05). Patients – Differences found between static and kinematic MRI measurements were statistically significant for BSO and LPD from 30° flexion up to full extension. For PTA, statistically significant differences were not found. Patients showed significantly higher mean values for LPT by static MRI than asymptomatic volunteers. Kinematic MRI did not present significant variations (Table 3).
Delta-parameters, asymptomatic volunteers versuspatients Statistically significant differences were found between findings in asymptomatic volunteers and patients for BSO-delta and LPD-delta at 30° and 20° flexion (p < 0.05). No statistically significant difference was found for PTA-delta (Table 4).
DISCUSSION The results of the present study demonstrate statisticallysignificant differences at 30° and 20° flexion forBSO-delta and LPD-delta, thus indicating that the lateral andmedial forces on the patella were higher in the patients group atthese flexion degrees. These parameters result from thearithmetical subtraction of values resulting from measurements bystatic and kinematic MRI, with and without active quadricepsmuscle contraction. These data are compatible with those reported in a study aboutthe femoropatellar dynamics. In the last 30° of extension,the tibial tubercle rotates externally, generating tension overthe quadriceps tendon and the patella is laterally dislocated,thus increasing the femoropatellar contactpressure(16–18). Tension on the lateralretinaculum is maximal between 30° and 20° flexion, andso is the risk of subluxation(1,11,19). Static sectional images, with "loaded quadriceps" could do thesame, but this is not a consensus. Sasaki & Yagi and Schutzeret al. demonstrated greater LPD and PTA under quadricepscontraction at static CT(20,21), but theclassification of Schutzer et al. for patients affected byfemoropatellar pain has not considered quadricepscontraction(22). Delgado-Martínez et al.have reported that CT scans performed with under quadricepscontraction did not provide any significant information ascompared with "unloaded quadriceps" imagingmodalities(23). There are several quantitative parameters described forevaluation of femoropatellar joint, but with no consensus in theliterature. Finding reliable anatomical references, as well asperforming appropriate measurements, not always isfeasible(24). A subjective evaluation could bean alternative. Apparently, it would be easier to distinguishbetween different grades of lateral subluxation, with lowinter-observer variation(11), however, suchapproach could not be adopted in the present study due to theabsence of accurate references to allow data reproducibility inthe comparison between static and kinematic MRI. The posterior intercondylar plane was adopted for all of thethree parameters. It has the advantage of not being affected bythe presence of hypoplastic lateral femoralcondyles(23). On the other hand, accordingDelgado-Martínez et al., the inter- and intra-observercorrelation coefficients were higher when the anteriorintercondylar plane was adopted(24). A reliable method for measuring patellar tracking is still tobe achieved, and, also, a definition for patellar normality isstill to be found(25,26). Reference valuesreported for static MRI are not valid for kinematic MRI,considering that mild lateral subluxation undetectable by staticMRI can be found at kinematic MRI at fullextension(27). Brossmann et al. have reportedstatistically significant differences between static andkinematic MRI in the group of asymptomatic volunteers for BSO andPTA from 10° flexion up to fullextension(15). The findings of the presentstudy are very similar. Statistically significant differenceswere found for all of the three parameters in this flexion range.For BSO and PLD these findings were observed from 20ºflexion up to full extension. According to Kujala et al., femaleand male femoropatellar joint behave differently at staticMRI(9). According to Csintalan et al. there aresignificant differences between female and male femoropatellarjoint biomechanics(28). These aspects emphasizethe necessity of further studies to define reference values forboth healthy female and male groups. An aspect to be emphasized in the present study is the coilpositioning. According to McNally and Muhle et al., current MRIdevices, in closed configuration, allow movement amplitudebetween 30° flexion up to fullextension(11,29). In the present study, therewas a concern whether there was enough space for all of theindividuals if they were positioned as above mentioned. Thesystem suggested by the present study certainly the availablespace is larger because the coil is placed 3 cm above the innerend of the examination table, so the knee movement can be easilyachieved in a greater space inside the magnet bore that otherwisewould be occupied by the examination table. Images acquisition was performed in dorsal decubitus with noresistance to extension. In ventral decubitus, the patella wouldbe fixed on the examination table, and its movement wouldtherefore be constrained(11). Individualspositioning and images acquisition were performed with nospecific positioning device. However, in strict compliance withpreviously defined standards for both anatomical landmarks andexamination methods, images acquisition was allowed within thesesame standards so reducing the probability of sequential errors.In the absence of a specially designed positioning device, atwo-step evaluation was required. The first step was aimed atensuring quasi 30° of knee flexion, and the secondone, ensuring active quadriceps contraction along the wholeextension movement during the kinematic MRI examination. Asignificant part of the time was spent on this alone. It has evenbeen considered constructing a special positioning device,however, at such an early stage of the project, the decision wasto apply the aforementioned system first and check itsfeasibility, postponing the construction of a specific device tothe future. McNally(11) and Shellock et al.(30) utilized a quadrature body coil, and Brossmann et al., a surface RF coil(10,15). Surface coils achieve a higher signal/noise ratio over a limited field of view. On the other hand, the homogeneous signal reception presented by the quadrature coil, is absent in surface coils(31). A dedicated quadrature knee coil seems to be the natural option, considering the better signal/noise ratio in relation to the body coil, with a more homogeneous signal as compared with the surface coil. A dedicated quadrature knee coil, however, is not devoid of drawbacks — aiming at enabling free extension of the knee the patella was placed near its inner end of the coil (Figure 1C) so the final position of the outer coil end is on the middle portion of the thigh. Its diameter restriction may not allow the examination of all patients. At least in the present study, the majority of patients with clinical femoropatellar syndrome were young women with relatively thin thighs and therefore all the examinations could be performed without any hindrance. Considering a single radiologist who was aware of the clinicaldata performed all the measurements, the interobservervariability could not be evaluated. With a small study group likethe present one, sampling homogeneity becomes a critical issue.All of the patients demonstrated clear clinical signs offemoropatellar instability, the majority of them bilateral. As aresult, an independent statistical analysis for both male andfemale individuals could not be performed. It should be emphasized that several phases of data handlingare required before delta-parameters are defined. Concern israised about systematic errors that could possibly be generatedthroughout the process. Nonparametric tests have less test powerfor null hypothesis rejection, and also are often moreconservative than the parametric tests(32). This new positioning system, along with the staticMRI/kinematic MRI combination could become a very sensitivemethod for the evaluation of biomechanical femoropatellardisorders.
CONCLUSION Kinematic MRI, when performed in association with static MRI,demonstrates that there are greater lateral forces being exertedon the patella at a 30° to 20° range of knee flexion,particularly in individuals symptomatic for femoropatellarinstability. These evidences demonstrate the potential clinicalusefulness of adding kinematic MRI to the arsenal for evaluatingthe femoropatellar joint in patients suspicious forfemoropatellar instability with no significant finding at staticMRI. Acknowledgments The authors would like to acknowledge the support of theCoordenadoria de Aperfeiçoamento do Pessoal deNível Superior (Capes) – Conselho Nacional deEducação (National Education Council), Ministry ofEducation, Brazil.
REFERENCES 1. Inoue M, Shino K, Hirose H, Horibe S, Ono K. Subluxation of the patella. Computed tomography analysis of patellofemoral congruence. J Bone Joint Surg Am 1988;70:1331–1337. [ ] 2. Lin F, Wang G, Koh JL, Hendrix RW, Zhang LQ. In vivo and noninvasive three-dimensional patellar tracking induced by individual heads of quadriceps. Med Sci Sports Exerc 2004;36:93–101. [ ] 3. Wilk KE, Briem K, Reinold MM, Devine KM, Dugas J, Andrews JR. Rehabilitation of articular lesions in the athlete's knee. J Orthop Sports Phys Ther 2006;36:815–827. [ ] 4. Hungerford DS, Barry M. Biomechanics of the patellofemoral joint. Clin Orthop Relat Res 1979; (144):9–15. [ ] 5. Wiberg G. Roentgenographic and anatomic studies on the femoropatellar joint. With special reference to chondromallacia patellae. Acta Orthop Scand 1941;12:319–410. [ ] 6. Merchant AC, Mercer RL, Jacobsen RH, Cool CR. Roentgenographic analysis of patellofemoral congruence. J Bone Joint Surg Am 1974;56:1391–1396. [ ] 7. Maldague B, Malghem J. Radiologie de l'instabilité rotulienne: intérêt du cliché de profil et de la vue axiale à 30° rotation externe. Acta Orthop Belg 1989;55:311–329. [ ] 8. Delgado-Martins H. A study of the position of the patella using computerised tomography. J Bone Joint Surg Br 1979;61-B:443–444. [ ] 9. Kujala UM, Österman K, Kormano M, Komu M, Schlenzka D. Patellar motion analyzed by magnetic resonance imaging. Acta Orthop Scand 1989;60:13–16. [ ] 10. Brossmann J, Muhle C, Büll CC, et al. Cine MR imaging before and after realignment surgery for patellar maltracking – comparison with axial radiographs. Skeletal Radiol 1995;24:191–196. [ ] 11. McNally EG. Imaging assessment of anterior knee pain and patellar maltracking. Skeletal Radiol 2001;30:484–495. [ ] 12. Pfirrmann CWA, Zanetti M, Romero J, Hodler J. Femoral trochlear dysplasia: MR findings. Radiology 2000;216:858–864. [ ] 13. Fithian DC, Mishra DK, Balen PF, Stone ML, Daniel DM. Instrumented measurement of patellar mobility. Am J Sports Med 1995;23:607–615. [ ] 14. Warwick R, William P. Gray's Anatomy. 35th ed. Edinburgh: Longman Group Limited, 1973;391-394, 450–460. [ ] 15. Brossmann J, Muhle C, Schröder C, et al. Patellar tracking patterns during active and passive knee extension: evaluation with motion-triggered cine MR imaging. Radiology 1993;187:205–212. [ ] 16. Reilly DT, Martens M. Experimental analysis of the quadriceps muscle force and patello-femoral joint reaction force for various activities. Acta Ortop Scand 1972;43:126–137. [ ] 17. Kumagai M, Mizuno Y, Mattessich SM, Elias JJ, Cosgarea AJ, Chao EY. Posterior cruciate ligament rupture alters in vitro knee kinematics. Clin Orthop Relat Res 2002;(395):241–248. [ ] 18. Li G, DeFrate LE, Zayontz S, Park SE, Gill TJ. The effect of tibiofemoral joint kinematics on patellofemoral contact pressures under simulated muscle loads. J Orthop Res 2004;22:801–806. [ ] 19. Grood ES, Suntay WJ, Noyes FR, Butler DL. Biomechanics of the knee-extension exercise. Effect of cutting the anterior cruciate ligament. J Bone Joint Surg Am 1984;66:725–734. [ ] 20. Sasaki T, Yagi T. Subluxation of the patella. Investigation by computerized tomography. Int Orthop 1986;10:115–120. [ ] 21. Schutzer SF, Ramsby GR, Fulkerson JP. The evaluation of patellofemoral pain using computerized tomography. A preliminary study. Clin Orthop Relat Res 1986;(204):286–293. [ ] 22. Schutzer SF, Ramsby GR, Fulkerson JP. Computed tomographic classification of patellofemoral pain patients. Orthop Clin North Am 1986;17: 235–248. [ ] 23. Delgado-Martínez AD, Estrada C, Rodríguez-Merchán EC, Atienza M, Ordóñez JM. CT scanning of the patellofemoral joint. The quadriceps relaxed or contracted? Intern Orthop 1996;20: 159–162. [ ] 24. Delgado-Martínez AD, Rodríguez-Merchán EC, Ballesteros R, Luna JD. Reproducibility of patellofemoral CT scan measurements. Intern Orthop 2000;24:5–8. [ ] 25. Katchburian MV, Bull AMJ, Shih YF, Heatley FW, Amis AA. Measurement of patellar tracking: assessment and analysis of the literature. Clin Orthop Relat Res 2003;(412):241–259. [ ] 26. Laprade J, Lee R. Real-time measurement of patellofemoral kinematics in asymptomatic subjects. Knee 2005;12:63–72. [ ] 27. O'Donnell P, Johnstone C, Watson M, McNally E, Ostlere S. Evaluation of patellar tracking in symptomatic and asymptomatic individuals by magnetic resonance imaging. Skeletal Radiol 2005;34:130–135. [ ] 28. Csintalan RP, Schulz MM, Woo J, McMahon PJ, Lee TQ. Gender differences in patellofemoral joint biomechanics. Clin Orthop Relat Res 2002; (402):260–269. [ ] 29. Muhle C, Brossmann J, Heller M. Kinematic CT and MR imaging of the patellofemoral joint. Eur Radiol 1999;9:508–518. [ ] 30. Shellock FG, Foo TKF, Deutsch AL, Mink JH. Patellofemoral joint: evaluation during active flexion with ultrafast spoiled GRASS MR imaging. Radiology 1991;180:581–585. [ ] 31. Welker KM, Tsuruda JS, Hadley JR, Hayes CE. Radio-frequency coil selection for MR imaging of the brain and skull base. Radiology 2001;221: 11–25. [ ] 32. Applegate KE, Tello R, Ying J. Hypothesis testing III: counts and medians. Radiology 2003;228: 603–608. [ ]
Received October 8, 2006. Accepted after revision January 15, 2007.
* Study developed in the Department of Imaging Diagnosis and Department of Orthopedics and Traumatology, Universidade Federal de São Paulo-Escola Paulista de Medicina (Unifesp-EPM), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554