Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 3 - May / June of 2007
Vol. 40 nº 3 - May / June of 2007
|
REVIEW ARTICLE
|
|
Magnetic resonance imaging in the staging of cervical cancer |
|
|
Autho(rs): Claudia C. Camisão, Sylvia M.F. Brenna, Karen V.P. Lombardelli, Maria Célia R. Djahjah, Luiz Carlos Zeferino |
|
|
Keywords: Cervical cancer, Staging, Magnetic resonance imaging |
|
|
Abstract:
IMD, Radiologist at Hospital São Lucas, Head for the Service of Radiology of Hospital do Câncer (HC II) – Instituto Nacional de Câncer (INCA), Rio de Janeiro, RJ, Fellow Master Degree at Universidade Estadual de Campinas (Unicamp), Campinas, SP, Brazil
INTRODUCTION Presently, uterine cervix carcinoma represents a significant public health problem. Despite the longer survival of patients because of earlier diagnoses and more effective therapies, this disease still remains as the leading cause of cancer-related death of women in the majority of developing countries(1). Cervical carcinoma is a slow-growing disease, usually invading the vagina and the paracervical space along the parametrium and uterosacral ligaments. Also, bladder, rectum, pelvic and paraaortic lymph nodes may be invaded(2). The pattern of pelvic dissemination of cervical carcinoma restricts the utilization of surgical treatment for early stages of the disease, given the lack of a safety margin in the resection of tumors which may have already affected the paracervical space. The staging recommended by International Federation of Gynecology and Obstetrics (FIGO) is widely adopted both for therapy planning and post-therapy follow-up, however it has shown to be inaccurate in the estimation of the actual tumor extent. Additionally, the FIGO staging system does not take into consideration relevant prognostic factors such as the tumor volume, vascularization, endophytic or exophytic growth, stromal invasion and lymph nodes involvement(3,4). Considering this flaw, the FIGO Committee on Gynecologic Oncology started recommending that the definite staging is based on the surgeon's and pathologist´s intraoperative findings (Figure 1)(5).
In cases where cervical carcinoma is locally advanced (above IIb), the majority of specialized centers have opted for exclusive radiotherapy or radiotherapy in association with chemotherapy. Therefore, the clinical finding that could not be intraoperatively confirmed should be based predominantly on highly accurate studies. However, in developing countries, basic imaging equipment is not always widely available in health services; so the gynecological examination ends up being the main alternative for staging of cervical carcinomas. The involvement of the parametrium evaluated by rectal examination is a parameter which frequently characterizes a locally advanced carcinoma(6). Mistakes may occur, especially due to underestimation of the disease extent as a consequence of limitations of the clinical-gynecological examination(7).
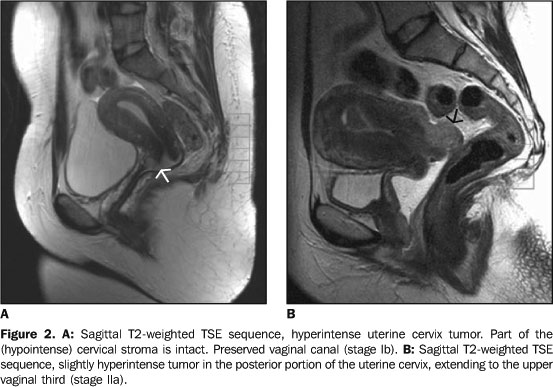
MAGNETIC RESONANCE IMAGING Magnetic resonance imaging (MRI) can evaluate the actual extent of the disease because of its high spatial and contrast resolution for pelvic tissues and organs. Some advantages of MRI are short acquisition time with multiplanar images, comfort for the patient, absence of ionizing radiation, and, mainly, the high reproducibility in the evaluation of musculotendinous structures in the pelvis which are of great relevance in the parametrium evaluation(8). T2-weighted images provide excellent details of the cervical anatomy and normal uterus, besides identifying the primary tumor and its extent. The normal cervical stroma presents a low density signal on this sequence, and about 95% of tumors of uterine cervix appear as slightly hyperintense masses in relation to the surrounding stroma(9) (Figure 2). Pre-invasive lesions of uterine cervix carcinoma cannot be identified on T2-weighted images, but may be described as an area of marked early impregnation in the arterial phase of MRI dynamic studies(10).
Prognostic parameters influencing in an appropriate therapy choice, and which may be evaluated by means of gynecological examination, can be evaluated by MRI with a good cost-effectiveness ratio, considering that patients with cervical cancer submitted to MRI as the initial staging method, require less tests or procedures in comparison with those submitted to a traditional staging method(11,12). As a matter of fact, MRI has shown a better accuracy than the clinical examination and computed tomography (CT) as staging methods, particularly in the parametrial evaluation. Comparative studies of the three methods (MRI, CT and clinical examination) have demonstrated 92% accuracy for MRI compared with 78% for clinical examination, and 70% for CT(13). With the arrival of new turbo sequences and phased-array coils, sensitivity reported for parametrial invasion was 100%(14). Other authors highlight a 98% negative predictive value for parametrial invasion in T2-weighted turbo spin-echo (TSE) and short tau inversion recovery (STIR) sequences(15,16). The correlation between uterine cervix carcinoma staging proposed by FIGO and MRI findings is described in Table 1(17).
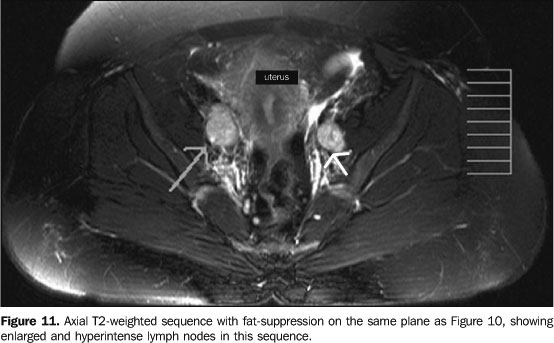
Examination technique MRI for staging of uterine cervix tumors should cover from the plane passing through the inferior renal pole to the vulva, including the paraaortic and pelvic regions. The anterior saturation band should be utilized as a routine to reduce respiratory and peristaltic artifacts. On the other hand, the posterior saturation band is dispensable. The use of antiperistaltic agents four to six hours before the examination also is recommended to reduce artifacts resulting from intestinal peristalsis(3,10). The phased-array coil improves the signal-noise ratio, allowing the acquisition of more detailed images than the formerly utilized body coils, and, consequently improving the imaging resolution. However, body coils may be useful for obese patients with a very protuberant abdomen, or for retroperitoneal evaluation(18). The utilization of endorectal and endovaginal coils has been described as means to produce high-signal images, but, despite the high degree of definition, their use is limited because of the lack of consensus about their advantages over the phased-array coils(19). The staging of uterine cervix tumors requires three planes in the T2-weighted TSE sequence in high resolution, i.e., 512 matrix, small field-of-view (FOV), sections always < 5 mm (preferably 3–4 mm), with gap of zero, all of them obtained in the axial plane. Additionally, a T1-weighted TSE sequence in the true axial plane of the pelvis with large FOV is essential for acquisition of a global pelvic view(17). Sagittal images are useful for demonstrating the relation between tumor and cervix, uterine body, vagina and adjacent organs such as bladder and rectum. On the other hand, axial images are relevant for detection of parametrial and pelvic wall invasion, ureteral and lymph nodes involvement. The coronal plane, in conjunction with the sagittal and axial planes, is useful in the parametrial evaluation, and particularly necessary for measurement of the tumor volume (Figure 3). T2-weighted TSE is the sequence of choice in the evaluation of lymph nodes involvement, since in this sequence, muscles and vessels appear hyperintense, differently from lymph nodes. Fat suppression improves even more the identification of structures or lesions surrounded by adipose tissues like parametrium and lymph nodes(15,20) (Figure 4). Many times, the use of contrast is not necessary in the staging, since, in most of cases, precontrast sequences provide the necessary information. Besides, dynamic sequences frequently underestimate the tumor volume and the depth of the stromal invasion, and should not be utilized for these purposes(21). However, the use of contrast agent may be useful for facilitating the identification of fistulous tracts in advanced diseases or in the post-therapy follow-up(10).
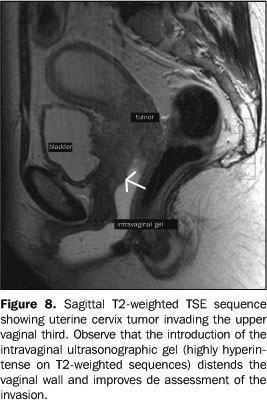
TUMOR GROWTH PATTERNS The tumor arises in the cervical canal and extends peripherally towards the cervical stroma, progressively replacing it. A full-thickness stromal invasion may occur, and, by contiguity, a parametrial invasion (IIb). Cervical canal obstruction is usual, and frequently causes the endometrial cavity to be distended with blood, serous fluid or purulent material(22) (Figure 5). Tumors extending into the uterine cavity are associated with a worst prognosis and higher prevalence of distant metastases(2). Clinically, tumors with endophytic growth are difficult to be measured, since the largest component cannot be directly visualized and evaluated in a gynecological examination. The clinical evaluation of exophytic tumors is easier, but MRI facilitates the identification of a possible vaginal invasion. Evaluation of parametrium and pelvic wall The parametrium is the connective tissue between the layers of the broad ligament. Medially it is contiguous with the uterus, cervix and proximal vagina; extending laterally to the pelvic wall. Inferiorly, it is nearly the cardinal ligament. It is predominantly consisted of fat through which run uterine vessels, nerves and lymphatic vessels(11). Parametrial invasion (above IIb) is a significant prognostic factor influencing in the diagnosis and therapeutic choice. On T2-weighted sequences, the interface between the normal cervical stroma and the parametrium appears like a hypointense ring or halo surrounding the cervix. A preserved hypointense halo represents a high negative predictive value for parametrial invasion(15,17). The indicator of parametrial invasion is the segmental interruption or complete absence of this halo in the interface between the cervical stroma and the parametrial fat, or yet, the clear protrusion of the tumor into the parametrium(13,23). Some authors correlate the complete replacement of the cervical stroma and the tumor extension into the uterine body with the parametrial invasion. In these cases, 94% of the parametrium is invaded, with direct relation between the size of the tumor and the parametrial involvement(15,22). Loss of parametrial fat may be an indicator of invasion, but this is a non-specific sign, since peritumoral inflammation also may result in loss of fat simulating invasion. Contrast-enhanced T1-weighted sequences have demonstrated higher accuracy than the T2-weighted in parametrial evaluation(10) (Figure 6). In cases where the tumor extends into the parametrium it may reach the ureter, causing hydronephrosis (IIIb). Hydronephrosis associated with mass in the uterine cervix are specific signs of parametrial invasion(12). Parametrial invasion up to the pelvic wall (IIIb) is diagnosed when the tumor cannot be separated from the pelvic wall at clinical examination. At MRI, this diagnosis is made when the distance between the tumor and the pelvic wall is < 3 mm, or when T2-weighted sequences show partial or complete loss of a normal hyposignal of the pelvic wall musculature (piriform muscle, internal obturator muscle, levator ani muscle or coccygeal muscle) (Figure 7). In these cases, iliac vessels become compressed and narrowed by the tumor, and the bone destruction may occur by direct extension of a diffusely infiltrated tumor(25). Vaginal involvement MRI is highly sensitive in the detection of vaginal invasion, with 93% accuracy(11). The sign of vaginal involvement is better characterized on high-resolution T2-weighted sequences, showing the segmental interruption of the normal hypointense signal of the vaginal wall, or yet a hyperintense vaginal thickening (tumor), or the mass itself in contiguity with the vaginal wall (Figure 8). Vaginal invasion corresponds to stage IIa; when this invasion extends up to the lower vaginal third, corresponds to stage IIIa(25). Additionally, the use of intravaginal ultrasonographic gel during the MRI acquisition is recommended to distend and fill the cavity with a highly hyperintense material on T2-weighted sequences in order to improve the tumor contrast (slightly hyperintense on T2-weighted sequences) and the vaginal wall contrast ((hypointense on T2-weighted sequences). This procedure improves the sensitivity in the evaluation of the vaginal invasion. About 20 ml of gel applied at the moment of the examination are sufficient(10).
Lymph node involvement Several studies have demonstrated the significance of the lymph node involvement as a factor of worsening in the survival prognosis of women affected by uterine cervix tumor(3,26). There are three drainage routes from the cervical lymph nodes through which the tumor propagates (Figure 9): the lateral route, along the external iliac vessels; the hypogastric route, along the internal iliac vessels; and the presacral route, along the uterosacral ligament. All of the three routes drain into the common iliac lymph nodes, through which the tumor may reach the paraaortic lymph nodes. Generally, the paracervical and parametrial lymph nodes are the first to be affected, followed by the obturator lymph nodes and, subsequently, the external and internal iliac lymph nodes(27). T2-weighted are the sequences of choice for evaluation of pelvic lymph nodes, since in these sequences vessels and musculature become hypointense, facilitating the differentiation from lymph nodes which are slightly hyperintense on T2-weighted sequences (Figure 10). T2-weighted TSE fat suppressed sequences allow the suppression of the adipose tissue surrounding the lymphatic vessels, improving the accuracy in the detection of pelvic adenomegalies(12) (Figure 11). Up to the present moment, the suspicion of lymph node metastasis by means of MRI is limited to the increase in the size of the lymph node. Lymph nodes > 10 mm in axial diameter are considered as abnormal. Also, some higher limits are suggested for determined specific sites, as follows: for lymph nodes in the internal iliac chain, 7 mm; for common iliac lymph nodes, 9 mm; and for external iliac lymph nodes, 10 mm. Positron emission tomography with fluoro-deoxy-D-glucose (PET-FDG) seems to offer higher specificity than MRI for enlarged pelvic lymph nodes(3). When lymph node central necrosis is identified, the positive predictive value for malignancy is 100%. It has been already demonstrated that lymph nodes with necrosis or signal intensity similar to the tumor presented worst prognosis. The diagnosis of lymph node necrosis may improve with the use of endovenous contrast(25,28).
Most recently, improvement has been demonstrated in the MRI sensitivity for detection of metastatic lymph nodes in uterine cervix tumors, utilizing a new type of lymph node-specific contrast agent called ferumoxtran-10, with nanoparticles of iron oxide (USPIO). However the utilization of this contrast agent is not a consensus yet(29). Considering that the FIGO staging system does not take the lymph nodes involvement into consideration, the detection of enlarged pelvic lymph nodes on MRI corresponds to stage IIIb, as well as the diagnosis of enlarged paraaortic lymph node corresponds to stage IVb(12). Invasion of bladder and rectum Invasion of bladder or rectum (IVa) may be difficult to be detected only by a physical examination. MRI has shown to be a reliable method for detection of bladder invasion with 83% sensitivity, specificity near 100%, and 99% accuracy. When the bladder presents invaded by the tumor, its wall, which normally is hypointense, shows a focal or diffuse area with increase in the signal intensity on T2-weighted sequences, or simply a vegetating mass into the lumen is observed(10,30). For defining the bladder invasion, it is important to observe that signal alteration is present both for the bladder muscle and mucosa, otherwise the tumor may be just contiguous to the bladder(4). Other indicative signs of invasion are hyperintensity on the internal surface of the posterior wall, nodularity or irregularity in the bladder wall (Figure 12). On the other hand, the vesico-ureteral junction is poorly evaluated because of the difficult visualization of a non-dilated ureter on MRI. Direct invasion of the ureter is not frequent, however, in the setting of ureter invasion, a tumor extension is observed along the uterosacral ligaments. Findings, usually, are: focal thickening or segmental interruption of the hypointense signal on the anterior rectal wall(10).
FINAL CONSIDERATIONS Even though MRI is not utilized by the majority of oncology services for staging uterine cervix tumors, and, up to this moment, it has not been officially approved by FIGO yet, it is the best imaging method in terms of accuracy for assessment of tumors, and plays an essential role in the therapeutic planning and follow-up(31). MRI has shown to be better than the clinical examination, and, when utilized as the initial staging method, reduces the number of invasive procedures and radiological studies such as urography, cytoscopy and rectosigmoidoscopy, with lower cost for the management of the disease. Additionally, the correct assessment of the tumor extent and volume allows optimizing the planning of the fields for external pelvic radiotherapy and brachytherapy. A recent study has demonstrated that the MRI-aided radiotherapy planning may reduce the possibility of geographic errors as compared with the conventional radiotherapy planning(32). It is important that the radiologist interpreting a pelvic MRI for uterine cervix tumor, is familiarized with the findings and, mainly, provides information regarding tumor volume, invasion of parametrium, vagina and adjacent organs, besides indicating the tumor growth type and lymph nodes involvement. Acknowledgments The authors thank the International Federation of Gynecology and Obstetrics (FIGO), for the free authorization for reproduction of the scheme for staging of cervical carcinoma; Rubens de Andrade, who has designed the figures; and the technician Marcello C. Galdino, for his dedication to the performance of the examinations.
REFERENCES 1. Ferlay F, Bray F, Pisanni P, Parkin DM. Globocan 2002: Cancer incidence, mortality and prevalence worldwide. IARC CancerBase No. 5, version 2.0. Lyon: IARC Press, 2004. [ ] 2. Eifel PJ, Berek JS, Thigpen JT. Cancer of cervix, vagina and vulva. In: DeVita VT Jr, Hellman S, Rosenberg SA, editors. Cancer: principles and practice of oncology. Philadelphia, PA: Lippincott, 1997;1433–1475. [ ] 3. Narayan K, Mckenzie AF, Hicks RJ, Fisher R, Bernshaw D, Bau S. Relation between FIGO stage, primary tumor volume, and presence of lymph node metastases in cervical cancer patients referred for radiotherapy. Int J Gynecol Cancer 2003;13:657–663. [ ] 4. Soutter WP, Hanoch J, D'Arcy T, Dina R, McIndoe G.A, deSouza N.M. Pretreatment tumor volume measurement on high-resolution magnetic resonance imaging as a predictor of survival in cervical cancer. Br J Obstet Gynaecol 2004;111:741–747. [ ] 5. Benedet JL, Bender H, Jones H, Ngan HY, Pecorelli S. FIGO staging classifications and clinical practice guidelines in the management of gynecologic cancers. FIGO Committee on Gynecologic Oncology. Int J Gynaecol Obstet 2000;20: 209–262. [ ] 6. DiSaia PJ, Creasman WT. Clinical gynecologic oncology. 6th ed. St. Louis, MO: Mosby, 2002; 53–95. [ ] 7. Bipat S, Glas AF, van der Velden J, Zwinderman AH, Bossuyt PMM, Stoker J. Computed tomography and magnetic resonance imaging in staging of uterine cervical carcinoma: a systematic review. Gynecol Oncol 2003;91:59–66. [ ] 8. Bezerra MRL, Soares AFF, Faintuch S, et al. Identificação das estruturas músculo-ligamentares do assoalho pélvico feminino na ressonância magnética. Radiol Bras 2001;34:323–326. [ ] 9. Seki H, Azumi R, Kimura M, Sakai K. Stromal invasion by carcinoma of the cervix: assessment with dynamic MR imaging. AJR Am J Roentgenol 1997;168:1579–1585. [ ] 10. Chiang SH, Quek ST. Carcinoma of the cervix: role of MR imaging. Ann Acad Med Singapore 2003;32:550–556. [ ] 11. Hricak H, Powell CB, Yu KK, et al. Invasive cervical carcinoma: role of MR imaging in pretreatment work-up-cost minimization and diagnostic efficacy analysis. Radiology 1996;198:403–409. [ ] 12. Pannu HK, Corl FM, Fishman EK. CT evaluation of cervical cancer: spectrum of disease. RadioGraphics 2001;21:1155–1168. [ ] 13. Kim SH, Choi BI, Han JK, et al. Preoperative staging of uterine cervical carcinoma: comparison of CT and MRI in 99 patients. J Comput Assist Tomogr 1993;17:633–640. [ ] 14. Vorgias G, Katsoulis M, Argyrou K, et al. Preoperative imaging of primary intra-abdominal gynaecological malignancies: diagnostic accuracy of CT-scan and MRI. A Greek cohort study. Eur J Gynaecol Oncol 2002;23:139–144. [ ] 15. Lam WW, So NM, Yang WT, Metreweli C. Detection of parametrial invasion in cervical carcinoma: role of short tau inversion recovery sequence. Clin Radiol 2000;55:702–707. [ ] 16. Tanaka YO, Nishida M, Yamaguchi M, Kohno K, Saida Y, Itai Y. MRI of gynaecological solid masses. Clin Radiol 2000;55:899–911. [ ] 17. Okamoto Y, Tanaka YO, Nishida M, Tsunoda H, Yoshikawa H, Itai Y. MR imaging of the uterine cervix: imaging-pathologic correlation. RadioGraphics 2003;23:425–445. [ ] 18. Gauger J, Holzknecht NG, Lackerbauer CA, et al. Breathhold imaging of the upper abdomen using a circular polarized-array coil: comparison with standard body coil imaging. MAGMA 1996;4: 93–104. [ ] 19. deSouza NM, Scoones D, Krausz T, Gilderdale DJ, Soutter WP. High-resolution MR imaging of stage I cervical neoplasia with a dedicated transvaginal coil: MR features and correlation of imaging and pathologic findings. AJR Am J Roentgenol 1996;166:553–559. [ ] 20. Follen M, Levenback CF, Iyer RB, et al. Imaging in cervical cancer. Cancer 2003;98(9 Suppl): 2028–2038. [ ] 21. Allen JR, Prost RW, Griffith OW, Erickson SJ, Erickson BA. In vivo proton (H1) magnetic resonance spectroscopy for cervical carcinoma. Am J Clin Oncol 2001;24:522–529. [ ] 22. Okuno K, Joja I, Miyagi Y, et al. Cervical carcinoma with full-thickness stromal invasion: relationship between tumor size on T2-weighted images and parametrial involvement. J Comput Assist Tomogr 2002;26:119–125. [ ] 23. Stehman FB, Randall ME, Michel H, Morken JV. Uterine cervix. In: Hoskins WJ, Perez CA, Young RC, editors. Principles and practice of gynecologic oncology. Philadelphia, PA: Lippincott Williams & Wilkins, 2005;743-822. [ ] 24. Scheidler J, Heuck AF, Steinborn M, Kimmig R, Reiser MF. Parametrial invasion in cervical carcinoma: evaluation of detection at MR imaging with fat suppression. Radiology 1998;206:125–129. [ ] 25. Taylor MB, Carrington BM, Davidson SE, Swindell R, Lawrance JAL. Staging of advanced cervical carcinoma using MRI-predictors of outcome after radical radiotherapy. Clin Radiol 2003; 58:532–541. [ ] 26. Landoni F, Maneo A, Colombo A, et al. Randomised study of radical surgery versus radiotherapy for stage Ib-IIa cervical cancer. Lancet 1997;350: 535–540. [ ] 27. Jeong YY, Kang HK, Chung TW, Seo JJ, Park JG. Uterine cervical carcinoma after therapy: CT and MR imaging findings. RadioGraphics 2003;23: 969–981. [ ] 28. Yang WT, Lam WWM, Yu MY, Cheung TH, Metreweli C. Comparison of dynamic helical CT and dynamic MR imaging in the evaluation of pelvic lymph nodes in cervical carcinoma. AJR Am J Roentgenol 2000;175:759–766. [ ] 29. Rockall AG, Sohaib SA, Harisinghani MG, et al. Diagnostic performance of nanoparticle-enhanced magnetic resonance imaging in the diagnosis of lymph node metastases in patients with endometrial and cervical cancer. J Clin Oncol 2005;23:2813–2821. [ ] 30. Kim SH, Han MC. Invasion of the urinary bladder by uterine cervical carcinoma: evaluation with MR imaging. AJR Am J Roentgenol 1997;168: 393–397. [ ] 31. Mayr NA, Taoka T, Yuh WTC, et al. Method and timing of tumor volume measurement for outcome prediction in cervical cancer using magnetic resonance imaging. Int J Radiat Oncol Biol Phys 2002;52:14–22. [ ] 32. Justino PB, Carvalho HA, Baroni RH, Blasbalg R, Leite CC.Valor da ressonância magnética no planejamento radioterápico dos tumores de colo de útero: resultados preliminares. Radiol Bras 2005;38:399–402. [ ]
Received August 9, 2005. Accepted after revision September 15, 2005.
* Study developed at Hospital do Câncer (HC II) – Instituto Nacional de Câncer (INCA), Ministério da Saúde (Ministry of Health), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554