Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 3 - May / June of 2007
Vol. 40 nº 3 - May / June of 2007
|
ICONOGRAPHIC ESSAY
|
|
Acute appendicitis: computed tomography findings - an iconographic essay |
|
|
Autho(rs): Marcelo Eustáquio Montandon Júnior, Cristiano Montandon, Gustavo Ribeiro Fiori, Carlos Alberto Ximenes Filho, Fernanda Coelho Barbosa da Cruz |
|
|
Keywords: Acute appendicitis, Vermiform appendix, Computed tomography |
|
|
Abstract:
ITitular Members of Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MDs, Radiologists at Clínicas da Imagem and Multimagem, and Hospital e Maternidade Jardim América, Goiânia, GO, Brazil
INTRODUCTION Acute appendicitis is the most important cause of abdominal pain requiring surgical intervention in the Western world(1,2). The early diagnosis of this disease is of paramount relevance for minimizing its morbidity. Imaging methods have represented a huge progress in the diagnosis of this entity, which used to be based essentially on clinical history, physical examination and laboratory tests results, considering that 20% to 33% of patients present with atypical symptoms(2). Diagnostic difficulty is higher in children, the elderly, and women in childbearing age. The disease may occur at any age range, with higher incidence in the second decade of life(1). The main imaging methods for acute appendicitis evaluation are ultrasonography (US) and computed tomography (CT). Patients presenting with typical clinical and laboratory signs may be directly referred for surgery and can dispense with imaging methods(1). However, imaging methods become essential when patients present with atypical symptoms, in retrocecal appendicitis, in obese patients, an in case of complications of the disease. The choice between US and CT is extremely variable, depending on some factors such as preference and experience of the institution, age, sex and biotype of the patient. Advantages of US include short acquisition time, non-invasiveness, low-cost besides not requiring preparation of the patients or contrast agent administration; however, is extremely operator-dependent(3). Considering the lack of ionizing radiation, and the fact of representing a good method for evaluation of acute gynecological conditions, US is recommended as the initial imaging test in women of childbearing age, pregnant women and children. CT represents an excellent diagnostic alternative for all the other cases, especially obese patients and in the complications of the disease (appendix perforation). The present study is aimed at describing the disease physiopathology; commenting main CT technical aspects; demonstrating and illustrating tomographic findings; and describing main differential diagnoses.
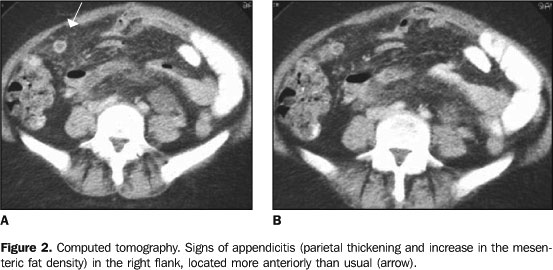
PHYSIOPATHOLOGY The adult appendix is a long diverticulum, measuring 10 cm in length, arising from the medial posterior wall of the cecum, about 3 cm below the ileocecal valve. The base is at a constant location, whereas the position of the tip of the appendix varies and may occupy several regions inside de abdominal cavity (Figure 2), including the pelvic region(1), the left iliac fossa, or even inside the inguinal canal. Clinical presentation is highly influenced by this wide variation in the topography of the appendix(1).
Obstruction of the appendiceal lumen due to the presence of fecalith (the most frequent one), lymphoid hyperplasia, foreign body or tumor(1). Appendicolith, a calcified fecalith, is less frequent but is associated with perforation and abscess formation(1,2). The obstruction of the lumen there is secretion accumulation leading to an increase in the intraluminal pressure, and determining stimulation of afferent visceral fibers between T8 and T10, with periumbilical epigastric pain as a consequence(1). This pain is not intense and usually poorly localized, with 2–5-hour duration. Anorexia, nausea and emesis may be present in this phase. The gradual increase in the intraluminal pressure exceeds the pressure of capillary perfusion, determining appendiceal walls ischemia, with loss of the epithelial integrity and bacterial mural invasion(1,2). Then, the pain migrates into the appendiceal region, generally in the right iliac fossa, and may be associated with signs of peritoneal irritation (positive sudden decompression). Fever is low or absent; the presence of high fever suggests perforation (1). In the absence of surgical intervention, appendicitis naturally progresses to perforation, with extension of the infection toward periappendiceal tissues. There may be a process blockage by the great omentum and/or small bowel loops, and, in some cases, a possible progress to intestinal obstruction(2). Local or distant abscess formation may occur. The appendicolith may migrate towards other sites of the abdominal cavity, determining collections formation(1,2). Other possible complications are infection dissemination to the abdominal wall, ureteral obstruction, venous thrombosis (portal system) and hepatic abscesses(1,2). Indiscriminate use of antibiotics may change the disease progress, difficulting an early diagnosis and increasing the morbidity. A delayed surgical intervention increases the risk for complications(1,2).
EXAMINATION TECHNIQUE Notwithstanding the advantages of helical CT over the conventional CT (sequential, transverse sections), with shorter acquisition time and possibility of images reconstruction with thinner slices, in our experience they present similar final results. Transverse multidetector CT followed by coronal reconstruction may improve the characterization of the appendix, but its sensitivity is the same only with the utilization of transverse sections(4). The images acquisition must cover the whole abdomen, from the xiphoid appendix to the pubic symphysis, since the appendix localization is highly variable and distant complications may coexist. Besides, the possibility of other differential diagnosis should be considered(3,5,6). In conventional CT equipment, the collimation (slice thickness) may range between 5 mm and 10 mm, possibly requiring thicker slices. We consider the evaluation of the whole abdomen with 10 mm collimation followed by thin slices (5 mm) on the right iliac fossa or on the suspicious region as sufficient. Many times, these thin slices are performed on the topography of the painful area indicated by the patients, facilitating the inflammatory process identification. In institutions where helical equipment is available, 5 mm-thick-slices are performed at 8 mm-intervals, followed by 5 mm-reconstruction, according to Lane et al.(6). Intravenous contrast agent is not routinely utilized(7,8), although it may be quite useful, especially in case of complications (perforated appendicitis), in young and thin patients (with paucity of peritoneal fat), in non-specific findings, and in the differential diagnosis of a malignant process(1). Retrograde contrast injection (500 ml 5% iodinated solution) by rectal via has been utilized by many authors, improving both the sensitivity and specificity of the method(4,5,9), but, in our services, we have utilized this technique only in dubious cases, reducing costs and making the procedure faster and more comfortable for the patient. The utilization of rectal-contrast reduces the incidence of false-positive results, since intestinal loops filled with fluid may be confused with distended appendices(2). The utilization of oral contrast is unnecessary in the majority of cases; it is helpful only in patients with non-specific abdominal pain, or when ileal opacification is necessary to solve any doubt in the case the rectal contrast is not elucidative(6). Finally, the fastest protocol in the evaluation of acute appendicitis is the one suggested by Lane et al.(6), who propose the use of non-contrast-enhanced helical CT covering the whole abdomen, with 5 mm-thick slices, 8 mm interval, and followed by 5 mm reconstruction.
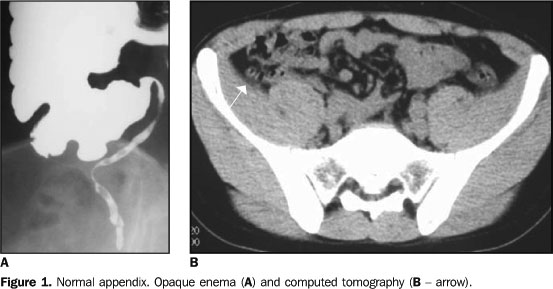
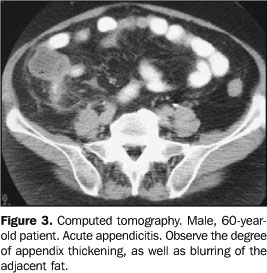
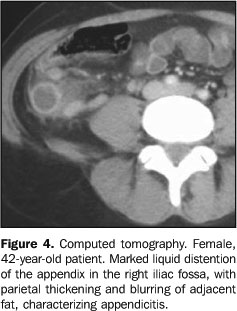
TOMOGRAPHIC FINDINGS Thick appendix – Appendiceal distention is the first tomographic sign, but its identification depends on the degree of distention, amount of surrounding fat, and technical quality of the study (slice thickness). The normal appendix is visualized in 67%–100% of asymptomatic adults submitted to CT(1) with thin slices (Figure 1). An appendix is considered as thick when > 8 mm in transverse (Figure 3). Usually, the appendix contents is liquid (Figure 4). The distention rarely exceeds 15–20 mm, since perforation generally occurs first. Higher values suggest the possibility of mucoceles or neoplasm. In patients with paucity of peritoneal fat, rectal contrast may facilitate its identification(5,9).
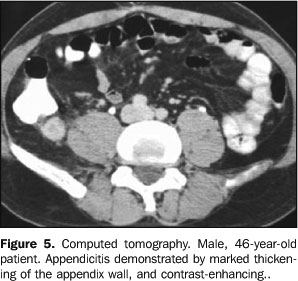
Appendix wall thickening – The normal appendiceal wall is 1–2 mm-thick. In the inflammatory process, mural thickening is present, and if intravenous contrast agent is utilized(1), we will observe the contrast uptake on the inflammed appendix walls (Figure 5).
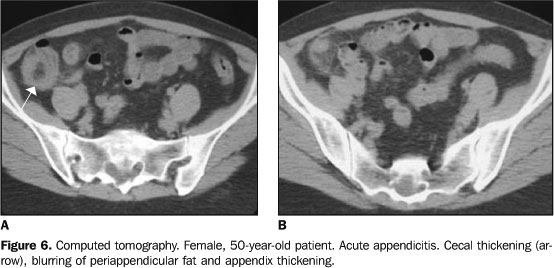
Blurring of the adjacent fat – The normal fat surrounding the appendix is homogeneous. In appendicitis, there is a blurring of this fat (Figure 3), a very frequent and significant sign found in 98% of cases(1). Cecal thickening – Also, the presence of some degree of inflammatory process is frequent in the adjacent loops(10), especially in the cecum (Figure 6).
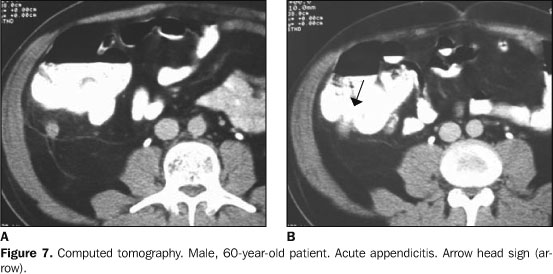
Arrow-head sign – Characterized by an arrow-head shape, as a result of edema in the base of the appendix(11), on rectal contrast-enhanced studies (Figure 7).
Appendicolith – Appendicolith does not necessarily indicate inflammation in the organ, since this finding is observed in asymptomatic adults without appendiceal distention. However, this finding gains high significance in the presence of other findings. After appendix perforation, the appendicolith may migrate to other sites in the abdominal cavity(1), resulting in formation of distant abscess, including during the post-operatory period (Figure 8). Inflammatory mass – In the case of an intense inflammatory process after appendiceal perforation, large, ill-define inflammatory masses may be observed in the right iliac fossa, determined by the blockage of the adjacent intestinal loops and omentum (Figure 9). In some cases, the appendix may be totally destructed by infection, so its identification is unfeasible(2). Free intraperitoneal fluid – The appendix perforation results in spillage of pus into the abdominal cavity, with possible bacterial peritonitis(1) (Figure 10). Extraluminal air – It may be found within a collection or free inside the cavity (pneumoperitoneum) as a result of appendiceal perforation (Figure 11). Pneumoperitoneum pneumoperitoneum is less frequent, and, if present, is small(1).
COMPLICATIONS Complications occur as a result from delayed diagnosis and appendix perforation(1,2), disseminating the infectious process into the peritoneal cavity. Main complications are the following: Abscess – A frequent complication, occurring in the appendix or in other sites inside the abdominal cavity, characterized by fluid collection, marginal enhancement after intravenous contrast administration, and many times blocked by adjacent intestinal loops (Figure 12). Venous thrombosis – Severe complication resulting from infectious process dissemination to the portal system. Also, hepatic abscesses may be observed. Intestinal obstruction – Initially, the blockage determined by the intestinal loops determines a regional ileum, however, as the disease progresses, obstruction may occur as a result from inflammatory process and ischemia (Figure 13). Sepsis – Extremely severe complication detectable by clinical diagnosis, resulting from intracavitary abscesses or diffuse peritonitis, with consequent systemic dissemination of the infectious process and high mortality. Ureteral obstruction – The inflammatory process may determine ureteral obstruction at right (Figure 14).
DIFFERENTIAL DIAGNOSIS Main differential diagnoses are(2,4,6): diverticulitis, epiploic appendagitis, typhilitis, omental infarct, Crohn's disease, colitis, acute cholelythiasis/cholecystitis, ureteral calculus/pyelonephritis, pelvic inflammatory disease/ovarian cyst, mesenteric lymphadenopathy, neoplasm.
REFERENCES 1. Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology 2000;215:337–348. [ ] 2. Gore RM, Miller FH, Pereles FS, Yaghmai V, Berlin JW. Helical CT in the evaluation of the acute abdomen. AJR Am J Roentgenol 2000;174: 901–913. [ ] 3. Sivit CJ, Applegate KE, Berlin SC, et al. Evaluation of suspected appendicitis in children and young adults: helical CT. Radiology 2000;216: 430–433. [ ] 4. Paulson EK, Harris JP, Jaffe TA, Haugan PA, Nelson RC. Acute appendicitis: added diagnostic value of coronal reformations from isotropic voxels at multi-detector row CT. Radiology 2005; 235:879–885. [ ] 5. Mullins ME, Kircher MF, Ryann DP, et al. Evaluation of suspected appendicitis in children using limited helical CT and colonic contrast material. AJR Am J Roentgenol 2001;176:37–41. [ ] 6. Lane MJ, Katz DS, Ross BA, Clautice-Engle TL, Mindelzun RE, Jeffrey RB Jr. Unenhanced helical CT for suspected acute appendicitis. AJR Am J Roentgenol 1997;168:405–409. [ ] 7. Freire Filho EO, Jesus PEM, D'Ippolito G, Szejnfeld J. Tomografia computadorizada sem contraste intravenoso no abdome agudo: quando e por que usar. Radiol Bras 2006;39:51–62. [ ] 8. Menezes MR, Kay FU. Tomografia computadorizada multidetectores não-contrastada na avaliação do abdome agudo: um novo paradigma no pronto-socorro? Radiol Bras 2006;39(2):IV–V. [ ] 9. Kamel IR, Goldberg SN, Keogan MT, Rosen MP, Raptopoulos V. Right lower quadrant pain and suspected appendicitis: nonfocused appendiceal CT – review of 100 cases. Radiology 2000;217: 159–163. [ ] 10. Rao PM, Wittenberg J, McDowell RK, Rhea JT, Novelline RA. Appendicitis: use of arrowhead sign for diagnosis at CT. Radiology 1997;202: 363–366. [ ]
Received May 12, 2006.
* Study developed at Clínicas da Imagem, Multimagem, São Camilo and São Mateus, and Hospital e Maternidade Jardim América, Goiânia, GO, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554