Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 3 - May / June of 2007
Vol. 40 nº 3 - May / June of 2007
|
ORIGINAL ARTICLE
|
|
Utilization of splenic impedance indices in the evaluation of portal hypertension |
|
|
Autho(rs): Daniel Dutra Cançado, Antonio Carlos Pires Carvalho, Célia Maria Coelho Resende |
|
|
Keywords: Impedance indices, Splenic artery, Portal hypertension, Radiology |
|
|
Abstract:
IMaster in Medicine (Radiology) by Faculty of Medicine, Universidade Federal do Rio de Janeiro (UFRJ), Rio de Janeiro, RJ, Brazil
INTRODUCTION The development of dynamic imaging methods, with higher definition and detail of parenchymal and vascular structures, has allowed a sensitive improvement in the evaluation of patients with hepatic diseases and its complications. Ultrasonography (US), in experienced hands, has shown to be a high-quality imaging method with a well-defined role in the evaluation of the liver, identifying from early cirrhotic alterations to the presence of masses and other findings which may suggest the presence of hepatocarcinoma or other lesions associated with hepatic parenchymal disease. Maybe, the major impact of US is observed in the analysis of the portal circulation, especially after the introduction of the Doppler technology(1). In the eighties, with the introduction and development of the technique of transjugular intrahepatic portosystemic shunt, the Doppler method emerged as an useful toll for following up patients who have been submitted to this procedure(2,3), as well as those who have undergone liver transplant(4). More recent studies start evaluating the usefulness of magnetic resonance imaging in the evaluation of the portal system, hepatic parenchyma and other solid viscera(5,6). Portal hypertension is an important condition found in cirrhotic patients, occurring principally because of an increase in the vascular resistance to the portal blood flow. Consequences of portal hypertension include ascites formation, hepatic encephalopathy and esophageal varices, the latest ones at risk of bleeding, implying a significant increase in mortality in this group of patients(7). US and echo-color Doppler have shown to be effective methods for the diagnosis of portal hypertension, allowing detection of the decrease in the flow velocity as well as the increase in diameter of the portal vein, two characteristics of portal hypertension(8,9). Most recently, increase in splenic and hepatic arteries impedance indices has also been observed in the setting of portal hypertension(10–12). Some studies have shown that splenic impedance indices presented a good correlation with the measure of the portal vascular resistance (one of the determining factors of portal hypertension), and also is one of the main predictors of the presence of esophageal varices at endoscopy(10,12). The present study was aimed at analyzing splenic impedance indices — resistance index (RI) and pulsatility index (PI) — in patients with chronic liver disease (cirrhotic patients, and those with chronic hepatitis without cirrhosis), and evaluating their efficacy to detect the presence of esophageal varices at digestive endoscopy.
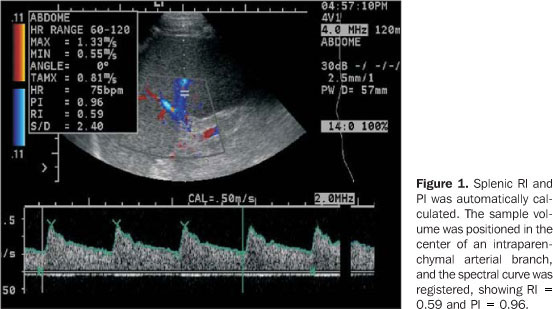
MATERIALS AND METHODS In the period between August/2003 and August/2005, a prospective study was performed in the Hospital Universitário Clementino Fraga Filho da Universidade Federal do Rio de Janeiro, with 63 patients, 42 of them with hepatic cirrhosis (25 men and 17 women; mean age = 49.7 ± 14.8 years), and 21 with chronic hepatitis (12 men and nine women; mean age 51.4 ± 8.8 years). The diagnosis of cirrhosis was based on hepatic biopsy results or, in their absence, on clinical-laboratory evaluation or detection of esophageal varices at endoscopy. The diagnosis of chronic hepatitis was based on hepatic biopsy results. Fifteen subjects (eight men and seven women) with no evidence of hepatic, renal or heart diseases, were considered as a control group, with mean age of 43.6 ± 15.3 years. Exclusion criteria were: patients submitted to previous treatment for varices with elastic ligature or sclerotherapy, as well as patients with conditions affecting the portal hemodynamics, such as hepatocellular carcinoma, portal vein thrombosis, or hepatofugal portal flow. The 42 cirrhotic patients were submitted to endoscopy for the relief of esophageal varices. During a period ranging between one and four weeks after endoscopy, the patients were submitted to echo-color Doppler US after a minimum 8-hour fasting period. Patients affected by chronic hepatitis and patients of the control group also were evaluated by US. The US systems utilized in the present study were an Acuson Aspen and a Sonoline G50 (Siemens®), with multifrequency 3.5 MHz convex transducers. All the procedures were performed by the authors D.D.C. and/or C.M.C.R., both without knowing the endoscopies results. The transducer was positioned on the left intercostal space, and the image of the splenic parenchyma was amplified to allow a better evaluation of the splenic artery branches by echo-color Doppler. The sample volume was placed inside de intraparenchymal arterial branches, during the breath-holding, and the spectral analysis of the blood flow was registered. Splenic PI and RI were calculated by the software included in the equipment, considering the average of the values obtained from at least three similar spectral curves (Figure 1).
The t-Student and Fisher-Snedecor tests in Anova variance analysis and Bonferroni's test were utilized for statistical analysis with significance level p £ 0.05.
RESULTS The most frequent etiology of cirrhosis was by hepatitis C virus infection, found in 25 patients (60%). The other causes included cryptogenic cirrhosis in seven patients (17%), hepatitis B virus infection in three (7%), autoimmune hepatitis in one (2%), cholestatic disease in two (5%), alcohol abuse in one (2%), alcohol abuse + hepatitis C virus in two (5%), and alcohol abuse + hepatitis B virus in one patient (2%). The 21 patients with chronic hepatitis presented C virus infection. As regards the Child-Pugh score, 19 patients were class A (44%), 15 class B (36%), four class C (10%), and four patients (10%) could not be scored because of data absence. As regards the presence of esophageal varices, 31 patients (74%) presented with varices at endoscopy, and 11 patients (26%) had a normal endoscopy. Data regarding impedance indices are shown in Table 1. Mean splenic RI and PI were higher in cirrhotic patients (RI = 0.63 ± 0.08; PI = 1.02 ± 0.22) in comparison with those with chronic hepatitis (RI = 0.58 ± 0.06; PI = 0.89 ± 0.15), and the healthy subjects (RI = 0.57 ± 0.04; PI = 0.87 ± 0.11), with a significant difference between cirrhotic patients and those with chronic hepatitis, and between cirrhotic patients and healthy subjects.
Cirrhotic patients without esophageal varices presented higher indices (RI = 0.67 ± 0.07; PI = 1.10 ± 0.21) as compared with cirrhotic patients with esophageal varices (RI = 0.62 ± 0.08; PI = 0.99 ± 0.22), However, this difference was not significant. The cirrhotic group (n = 42) was subdivided into cirrhotic without (n = 25) and with (n = 17) collateral circulation evidenced at US, in order to evaluate possible hemodynamic alterations in the splenic territory in patients who developed collateral circulation. The indices were higher in the cirrhotic patients without evidence of collateral circulation (RI = 0.65 ± 0.07; PI = 1.06 ± 0.22) as compared with cirrhotic with collateral circulation (RI = 0.60 ± 0.08 and PI = 0.97 ± 0.21), with a significant difference only for RI.
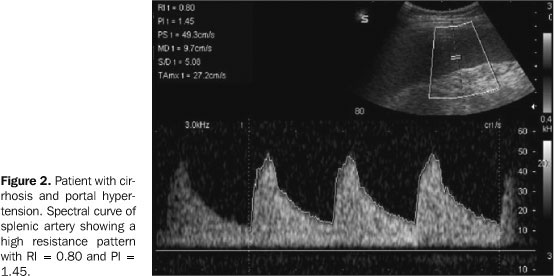
DISCUSSION Gray scale US and, most recently, echo-color Doppler have played a relevant role in the evaluation of portal hypertension(8,9,13–15). It is a relatively low-cost method besides being noninvasive and widely available. However, the evaluation of portal hypertension severity by US, as well as its value as a predictor of esophageal varices still remains controversial in the literature(8,16–19). Recently, the hemodynamic evaluation of the splenic artery has been performed with echocolor Doppler, demonstrating a direct relation between splenic impedance indices and portal vascular resistance(10–12,20). The splenic arterial and capillary beds are related to the peripheral territory of the portal system, reflecting the system hemodynamic changes. A possible explanation for this sensitivity of impedance indices to the portal hemodynamics would be the peculiar splenic venous circulation. The spleen presents a venous circulation different from any other organ, characterized by the presence of the red pulp. In case of portal hypertension, there is an accumulation of red cells in the sinusoids and dilated pulp cords. The splenic arterial hemodynamics may be changed by the venous congestion, causing a decrease in the arterial diastolic velocity and a consequent increase in the impedance indices(10,11) (Figure 2).
According to Bolognesi et al.(11), patients with more severe portal hypertension — those with portal vein thrombosis or hepatofugal portal flow — presented the highest impedance indices, and therefore these indices were considered as an indicative of the condition. In another study performed by Bolognesi et al.(10), the utilization of a formula for estimating the portal pressure — with the splenic PI and the measure of the portal flow — demonstrated a significant correlation with the direct measurement of the portal pressure and a good accuracy in the prediction of mild (< 16 mmHg) or severe (> 16 mmHg) portal hypertension. In the present study, the impedance indices were increased in cirrhotic patients (RI = 0.63 ± 0.08; PI = 1.02 ± 0.22) as compared with patients with chronic hepatitis (RI = 0.58 ± 0.06; PI = 0.89 ± 0.15) and healthy subjects (RI = 0.57 ± 0.04; PI = 0.87 ± 0.11). These results are similar to those reported by Bolognesi et al.(11), evaluating 167 cirrhotic patients (RI = 0.64 ± 0.08 and PI = 1.03 ± 0.24 in cirrhotic patients, and RI = 0.51 ± 0.05 and PI = 0.72 ± 0.11 in healthy subjects), and by Piscaglia et al.(20), who have found RI = 0.63 ± 0.07 in cirrhotic patients, RI = 0.53 ± 0.05 in patients with chronic hepatitis, and RI = 0.55 ± 0.05 in healthy subjects, in a study with 124 patients with chronic hepatopathy. Indices in patients with chronic hepatitis were near those observed in healthy subjects, probably because of the absence, at that moment, of a significant vascular resistance, like the one occurring in patients with an already established cirrhosis. The utilization of impedance indices for patients with chronic hepatitis may contribute for a better follow-up of the chronic hepatopathy progress, and the suspicion of cirrhosis should be raised in case of increase in these indices. The group of cirrhotic patients without esophageal varices presented higher indices (RI = 0.67 ± 0.07; PI = 1.10 ± 0.21) as compared with the group of cirrhotic patients with esophageal varices (RI = 0.62 ± 0.08; PI = 0.99 ± 0.22), however, this result had no statistical significance in the present study. In truth, these results diverge from those reported in the literature where cirrhotic patients with esophageal varices tended to present higher impedance indices(11,12). Piscaglia et al.(12) also have observed that RI between 0.61 and 0.63 presented higher accuracy for prediction of esophageal varices (respectively 75% and 76%). The present study demonstrated that, in cirrhotic patients without evidence of collateral circulation at US, impedance indices were higher (RI = 0.65 ± 0.07; PI = 1.06 ± 0.22) as compared with cirrhotic patients with collateral circulation (RI = 0.60 ± 0.08 and PI = 0.97 ± 0.21), the RI being the parameter with statistical significance. Parametric alterations of echo-color Doppler, such as the measurement of the portal vein and portal flow velocity in the presence of umbilical vein recanalization, have already been reported, such alterations underestimating the presence of portal hypertension(21). This occurred because the recanalized umbilical vein represented a portosystemic shunt, tending, as a result, to normalize the portal vein velocity. However, the effect of collateral circulation on splenic impedance indices had not yet been reported in the literature. It is known that, in patients submitted to liver transplant and surgical correction of portal hypertension, there is a decrease in these indices caused by the reduction of the portal vascular resistance(11,22,23). Likewise, there is some speculation if the presence of collateral circulation also would contribute for the effect of portal system decompression, diverting the portal flow to the systemic circulation, and, as a result, causing a decrease in the indices (Figure 3). The present study presents some limitation such as the absence of an expressive casuistic, which may have impaired the evaluation of indices as indicators of esophageal varices. Another possible limiting factor is the lack of homogeneity in the sample of cirrhotic patients, since it has included patients with more advanced grades of hepatic dysfunction (Child-Pugh B and C classes), besides an array of causes of hepatic cirrhosis. It is still to be known if the physiopathological and hemodynamic mechanisms of portal hypertension are the same among the several etiologies. Even considering the mentioned limitations, splenic impedance indices seem to be useful for evaluation of patients with chronic liver disease, and present increased in patients with cirrhosis. New studies are necessary to evaluate the collateral circulation effects on these indices, as well as their efficacy as indicators of esophageal varices.
REFERENCES 1. Machado MM, Rosa ACF, Barros N, et al. Estudo Doppler na hipertensão portal. Radiol Bras 2004; 37:35–39. [ ] 2. Marcelino ASZ, Oliveira IRS, Chammas MC, et al. Parâmetros dopplervelocimétricos na avaliação da perviedade da anastomose portossistêmica intra-hepática transjugular (TIPS). Radiol Bras 2005;38:53–59. [ ] 3. Kisilevzky NH. TIPS para o controle das complicações da hipertensão portal: eficácia, fatores prognósticos associados e variações técnicas. Radiol Bras 2006;39:385–395. [ ] 4. Costa-Silva L, Lima AS, Tavares Júnior WC, Rocha PRS. Evidências de hiperfluxo portal no pós-operatório de transplantes hepáticos. Radiol Bras 2005;38:261–264. [ ] 5. Caldana RP, Bezerra ASA, D'Ippolito G, Szejnfeld J. Estudo da circulação hepatomesentérica pela angiografia por ressonância magnética com gadolínio: comparação entre doses simples e dupla no estudo de pacientes esquistossomóticos. Radiol Bras 2006;39:243–251. [ ] 6. Bezerra ASA, D'Ippolito G, Caldana RP, Cecin AO, Szejnfeld J. Avaliação hepática e esplênica por ressonância magnética em pacientes portadores de esquistossomose mansônica crônica. Radiol Bras 2004;37:313–321. [ ] 7. Garcia-Tsao G. Portal hypertension. Curr Opin Gastroenterol 1997;13:263–270. [ ] 8. Haag K, Rössle M, Ochs A, et al. Correlation of duplex sonography findings and portal pressure in 375 patients with portal hypertension. AJR Am J Roentgenol 1999;172:631–635. [ ] 9. Kok T, van der Jagt E, Haagsma EB, Bijleveld CM, Jansen PL, Boeve WJ. The value of Doppler ultrasound in cirrhosis and portal hypertension. Scand J Gastroenterol Suppl 1999;230:82–88. [ ] 10. Bolognesi M, Sacerdoti D, Merkel C, Bombonato G, Gatta A. Noninvasive grading of the severity of portal hypertension in cirrhotic patients by echo-color-Doppler. Ultrasound Med Biol 2001; 27:901–907. [ ] 11. Bolognesi M, Sacerdoti D, Merkel C, et al. Splenic Doppler impedance indices: influence of different portal hemodynamic conditions. Hepatology 1996;23:1035–1040. [ ] 12. Piscaglia F, Donati G, Serra C, et al. Value of splanchnic Doppler ultrasound in the diagnosis of portal hypertension. Ultrasound Med Biol 2001;27:893–899. [ ] 13. Bolondi L, Gandolfi L, Arienti V, et al. Ultrasonography in the diagnosis of portal hypertension: diminished response of portal vessels to respiration. Radiology 1982;142:167–172. [ ] 14. Zironi G, Gaiani S, Fenyves D, Rigamonti A, Bolondi L, Barbara L. Value of measurement of mean portal flow velocity by Doppler flowmetry in the diagnosis of portal hypertension. J Hepatol 1992;16:298–303. [ ] 15. Iwao T, Toyonaga A, ho K, et al. Value of Doppler ultrasound parameters of portal vein and hepatic artery in the diagnosis of cirrhosis and portal hypertension. Am J Gastroenterol 1997;92: 1012–1017. [ ] 16. Kuo CH, Changchien CS, Tai DI, Chen JJ. Portal vein velocity by duplex Doppler ultrasound as an indication of the clinical severity of portal hypertension. Changgeng Med J 1995;18:217–223. [ ] 17. Merkel C, Sacerdoti D, Bolognesi M, Bombonato G, Gatta A. Doppler sonography and hepatic vein catheterization in portal hypertension: assessment of agreement in evaluating severity and response to treatment. J Hepatol 1998;28:622–630. [ ] 18. Schneider AW, Kalk JF, Klein CP. Hepatic arterial pulsatility index in cirrhosis: correlation with portal pressure. J Hepatol 1999;30:876–881. [ ] 19. Siringo S, Bolondi L, Gaiani S, et al. The relationship of endoscopy, portal Doppler ultrasound flowmetry, and clinical and biochemical tests in cirrhosis. J Hepatol 1994;20:11–18. [ ] 20. Piscaglia F, Donati G, Cecilioni L, et al. Influence of the spleen on portal hemodynamics: a non-invasive study with Doppler ultrasound in chronic liver disease and haematological disorders. Scand J Gastroenterol 2002;37:1220–1227. [ ] 21. Sacerdoti D, Bolognesi M, Bombonato G, Gatta A. Paraumbilical vein patency in cirrhosis: effects on hepatic hemodynamics evaluated by Doppler sonography. Hepatology 1995;22:1689–1694. [ ] 22. Piscaglia F, Zironi G, Gaiani S, et al. Systemic and splanchnic hemodynamic changes after liver transplantation for cirrhosis: a long-term prospective study. Hepatology 1999;30:58–64. [ ] 23. Soresi M, Bascone F, Magliarisi C, et al. Hemodynamic changes in splanchnic circulation after orthotopic liver transplantation in patients with liver cirrhosis. Abdom Imaging 2002;27:541–545. [ ]
Received January 20, 2006.
* Study developed at Hospital Universitário Clementino Fraga Filho, Universidade Federal do Rio de Janeiro (HUCFF-UFRJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554