Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 2 - Mar. / Apr. of 2007
Vol. 40 nº 2 - Mar. / Apr. of 2007
|
ORIGINAL ARTICLE
|
|
Computed tomography findings in patients less than 20 years old with lymphoma |
|
|
Autho(rs): Adriana Moreira Viana Borba, Alexandra Maria Vieira Monteiro, Cláudio Marcio Amaral de Oliveira Lima, Érica Barreiros Ribeiro, Stella Beatriz Gonçalves de Lucena, Luis Flávio Skinner |
|
|
Keywords: Lymphoma, Computed tomography |
|
|
Abstract:
IPost-graduation Student in Radiology at Escola Médica da Pontifícia Universidade Católica do Rio de Janeiro (PUCRJ), Rio de Janeiro, RJ, Brazil
INTRODUCTION The term lymphomas refer to malignant neoplasms of specificcells in the lymphatic system (T-cells, B-cells andhistiocytes)(1,2). They are subdivided into twogroups, Hodgkin's lymphomas (HL) and non- Hodgkin's lymphoma(NHL)(1). NHL is more frequent in the childhood thanHL, and is the third most common neoplasm after leukemia andcentral nervous system tumors in children less than 16 years ofage. HL represents about 5% of all cancers in infants andchildren(3). NHL is prevalent in children less than 16 years of age, whileHL most frequently affects children with more than five years ofage and is rare under this age. The incidence is higher in malesat a 3:1 ratio for NHL, and 2:1 for HL(3). Clinical characteristics, radiological findings, histologicalpatterns, therapy and prognosis of pediatric Hodgkin's diseaseare similar to those of Hodgkin's disease inadults(3). Generally, HL is characterized by theorderly spread of the disease from a lymph node group toanother(4); so frequently the involvement of uppermediastinal lymph nodes (both prevascular and paratracheal) isobserved in about 98% of patients with intrathoracic disease.Approximately one third of these patients present unilateral orbilateral hilar lymphadenopathy(5). Thymic involvementis observed in up to 70% of patients with mediastinal Hodgkin'sdisease, generally associated with an increase of lymph nodes inother sites of the mediastinum(5). In the childhood, the majority of NHL is extranodal, incontrast to both the NHL in the adult and Hodgkin's disease atany age range. In the childhood, the most frequent primary siteis the abdomen, particularly the ileocecal region, followed bythe mediastinum (approximately 25%)(3). Imaging methods, particularly computed tomography, areinvaluable tools for evaluating the disease extent, planning thetreatment and analyzing the subsequent response to thetherapy(6). The aim of the present study was to describe general findingsof computed tomography according their histological subtype inless-than-20-year-old patients with diagnosis of lymphoma.
MATERIALS AND METHODS Retrospective study of digital files of the ComputedTomography Unit in Centro Universitário de Controle doCâncer at Hospital Universitário Pedro Ernesto –Universidade do Estado do Rio de Janeiro, Rio de Janeiro, RJ,Brazil, during the period between March 2003 and July 2005. Inthis period 1,356 computed tomography studies were performed inpatients with less than 20 years of age. Of these patients, 22were diagnosed with lymphoma - 12 of them HL, and 10 NHL. Inclusion criteria were: age under 20, and diagnostic andhistopathological confirmation of lymphoma type. Two patientswere excluded due the absence of histological categorization(follow-up in another hospital unit). The equipment utilized was a GE HiSpeed helical model, with aprotocol including base of the neck, chest, abdomen andpelvis. All of the studies were reviewed by two investigators, andonly those where there was a consensus were taken intoconsideration. Of a total of 22 cases, 12 were HL, and 10 NHL. Sixteenpatients were men and six women, with ages ranging between threeand 20 years (mean age 11.5). In the HL group was in the agerange between six and 20 years, and the NHL, between three and 20years. In the HL group, eight patients were male and four, female. Inorder of frequency, the following histological subtypes werefound: mixed cellularity (41.6%), nodular sclerosis (33.3%),lymphocytic predominance (16.6%), and lymphocytic depletion(8.5%). In the NHL group, eight were men, and two were women.Predominant histological subtypes were: diffuse large B celllymphomas (40%); Burkitt's lymphomas (40%), followed byT-lymphoblastic lymphomas (10%) and small-cell lymphomas(10%). Of a total of 22 patients, 14 (63%) underwent examination forthe first time, and eight (36%) for follow-up. No patientspresented with coexistent infection. One patient died during thestudy period.
RESULTS Among the computed tomography findings, we observed that mediastinal lymphadenopathy was the most frequent finding (59%), predominating in the HL group (75%), followed by hepatosplenomegaly (50%), cervical and retroperitoneal lymphadenopathy (27.3%) (Tables 1 and 2).
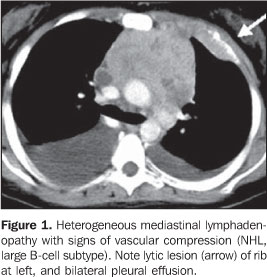
As regards the presence of lymphadenopathy (Table 1) a high predominance in the HL group compared with the NHL group. In the majority of cases, the lymph node mass presented homogeneous contrast enhancement, with the exception of two cases: one in the HL group, and another in the NHL group (Figure 1). No calcified lymph node was detected.
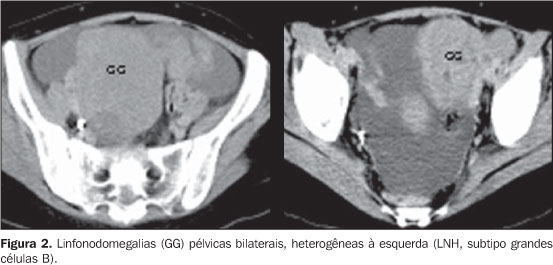
Cervical lymphadenopathies were predominantly bilateral, most frequently detected in the HL group, without the presence of necrosis and/or calcification. The other lymph node chains affected showed variable presentations, highlighting especially the pelvic ones in the most severe case (Figure 2).
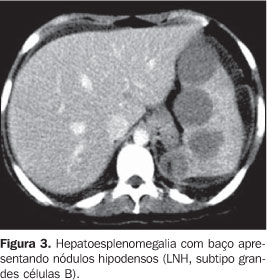
Extranodal findings were more frequent in the NHL group, as shown on Table 2. Lymphadenopathy was the most frequent one, and in one of these cases, the splenomegaly was heterogeneous (Figure 3). Hepatomegaly as an isolate finding was observed only in the HL group (n = 2).
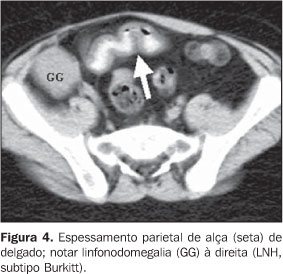
Small bowel parietal thickening (n = 4) was found in four patients, all of them in the NHL group, 50% of Burkitt subtype. This alteration was associated exclusively with hepatosplenomegaly in three of the four cases (75%), and was found as a single manifestation in only one case (Figure 4).
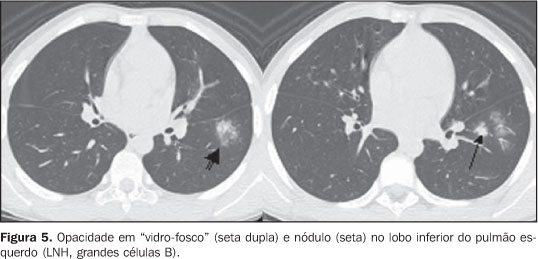
Pleural effusion (n = 3), pericardial effusion (n = 1), andascites (n = 1) were found only in the NHL group. Pulmonary involvement represented by nodule(s) (n = 2) was found only in the NHL group. Ground-glass opacities (n = 2) were equivalent in both groups (Figure 5). Associated infection was not found in any of the cases.
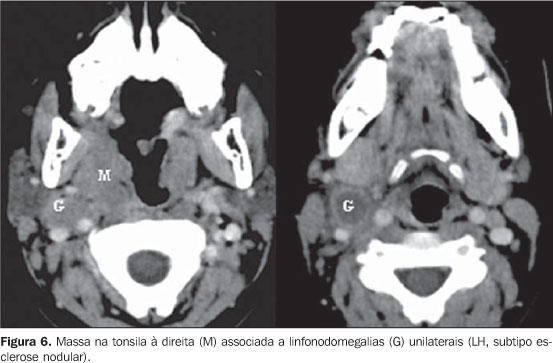
Only one unilateral mass was found in the tonsil, associated with cervical lymphadenopathy, in the HL group, nodular sclerosis subtype (Figure 6).
Bone lesions, in the most severe case of NHL group (large B cell subtype) were multiple and mixed (lytic and blastic aspect) (Figure 7).
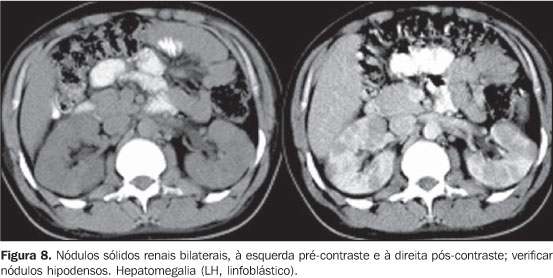
There was one case of renal involvement characterized by multiple and bilateral solid nodules (Figure 8) in the HL subtype.
DISCUSSION The utilization of imaging methods for diagnosis, follow-upand healing management of patients with lymphoma has increasinglyassumed an essential role in the management of this disease.According to the Ann Arbor System, the staging itself justifiesthe use of imaging methods, since it is based on a systematizedanalysis of the disease extent(4,6). Computed tomography, due the fast images acquisition incomparison with magnetic resonance imaging, allows a rapid andcomprehensive staging, which is essential for definition of theclinical oncological treatment. Reports in the literaturedescribe, for example, changes in the planning of up to 10% ofcases, based on data from computed tomography(6), aswell as the identification of non-suspect sites of intrathoracicdiseases or the elucidation of questionable radiologicalabnormalities which eventually might change therapeuticdecisions(5). As regards the frequency of general imaging findings, our dataare consistent with the literature reviewed(3,7). The pattern of thoracic involvement in patients with lymphomais variable, and, at the moment of the diagnosis this involvementis more frequent in HL than in NHL, with presence in up to 11.6%of cases of HL. In these patients, the pulmonary involvement isassociated with the presence of the disease in hilar ormediastinal lymph node chains. In cases with unilateral hilaradenopathy, parenchymal involvement, when present, occurs in theipsilateral lung8,9). The pulmonary disease, withoutlymph node involvement is more frequent in recurrent lymphomas.Pulmonary involvement is frequently asymptomatic and symptoms,when present, are usually non-specific(8,10). Onecharacteristic of HL in the lung is the dissemination along thelymphatic route(10) and, in the mediastinum, thedissemination contiguously from a lymph node group to the next,with initial presentation in about 65%–80% of patients withabnormal chest x-ray(5,10). In otherstudies(5) reporting a 98% frequency in patients withintrathoracic disease, we have observed a prevalence ofmediastinal lymphadenopathy in relation to other sites, in the HLgroup, inclusive. We have not identified calcifications which rarely are seenbefore the therapy, even in cases of follow-up; but areas withnecrosis were detected in both subtypes(7).Differently from carcinomas, lymphoma masses are more likely todisplace adjacent structures than invade them(5), justas the cases of vascular compression observed in the presentstudy. Approximately one third of patients with thoracic diseasepresent unilateral or bilateral hilarlymphadenopathy(5), a finding observed in only onecase in our study. Contrarily to HL, NHL tends to manifest as a single, bulkylymph node mass, and not as individually increased lymph nodes.According to our results, in the chest, other sites are usuallyinvolved, such as pulmonary parenchyma, pleura andpericardium(2,10). In patients with mediastinal HL and NHL mediastinal, asecondary pulmonary involvement usually is seen later with theprogress of the disease. Only 12% of patients with HL and 4% ofthose with NHL present pulmonary involvement as a primarymanifestation of the disease. The most frequent patterns observedon computed tomography studies are parenchymal consolidation,nodules or masses, and lymphatic dissemination. Among thesepatterns, nodules are the most frequent ones (50% to 90% ofcases), and can be solitary or, most frequently, multiple. Cavitation is rare (< 10%), but may occur, especially inthe HL subtype. Another aspect described is the presence ofground-glass halo surrounding a nodule (halo sign) or isolatedly,due to alveolar septa infiltration by neoplastic cells, withpreserved alveolar spaces(10). In the presentstudy, only one case of nodule presented this pattern, and, whenin association with ground-glass opacity, there was a randomdistribution. The protocol for chest examination must include the base ofthe neck as a routine, to discard head & neckinvolvement(5,7,11). Cervical lymphadenopathieswere the second main finding in general frequency order,predominating in the HL group. Lymphoma is the second mostfrequent malignant neoplasm in the neck, besides being the mostcommon extralaryngeal malignant neoplasm. NHL is one of the mostfrequent malignant neoplasms in children. Neck lymphoma usuallyinvolves the adenoids as well as the lingual and pharyngealtonsils (Waldeyer's ring); the unilateral tonsillar increase inchildren is highly suspect for malignancy. Cervical lymph nodes,especially internal jugular and spinal accessory lymph nodeswhich generally also are involved. In imaging studies groups ofnon-necrotic lymph nodes are observed(5,11). Inthe case of tonsilar mass, we observed association with cervicallymphadenopathies, some of them with a hypodense nucleus. The greatest part of NHLs in the childhood is extranodal, incontrast to both the NHL in adults and Hodgkin´s disease atany age. The most frequent primary site of NHL in children is theabdomen; particularly the ileocecal region(3),literally in agreement, and according to our results,predominantly associated with hepatosplenomegaly. Common findings of computed tomography in all the types ofsmall bowel lymphoma are: intestinal wall thickening, sometimesnodular in a diffuse or focal distribution, and also distinctlymph node masses in the mesenteric folds of the involvedsegment; in some cases, the CT shows a single focal, frequentlycecal, colonic mass. The evaluation of the liver and spleen is an essential part ofthe computed tomography study. Although an organ enlargement isan indicator of its involvement, this is not a reliablediagnostic criterion, and the sensitivity for detection of focallesion in dubious cases of lymphomas is significantly increasedwith sequential CT slices obtained after contrast bolusinjection(12). Secondary splenic involvement isfrequent both in HL and NHL, and malignant splenic neoplasm isthe most common. It is estimated that at the moment of thediagnosis there is splenic involvement in one-fourth to one-thirdof patients with HL or NHL. In patients with NHL, the splenicinvolvement is associated with infiltration of paraaortic lymphnodes in approximately 70% of them. Homogeneous organenlargement, miliary nodules, multifocal lesions between 1 cm and10 cm, and solitary mass are some forms of presentation. In casesof necrosis in large lesions, an irregular, cystic pattern isobserved, and a case of a patient with fever associated withlymphoma mimicking splenic abscess is reported in theliterature(5). In the present study, multiple lesionsdid not present peripheral contrast enhancement, which inassociation with clinical data, characterized the diseasemanifestation. Most frequently, in NHL, the small bowel mesentery and omentumare involved by a tumor disseminated via the intraperitonealpathway. The four general patterns of computed tomography imagingare: rounded masses, cake-like masses, ill-defined masses, andstellate mesentery. Rounded masses are more frequent in NHL,basically due to the lymphadenopathy, and not to theintraperitoneal dissemination(5,13). The presence ofascites suggests this forma of dissemination. Bone lymphoma causes diffuse or focal osseous pain and usuallycorresponds to dissemination from any other primary site.Manifestations of systemic dissemination, such as anaplasticlymphoma of the skin, may occur in association with alterationsrelated to the local tumor(2,14). The case ofbone involvement identified in the present study was exactly theone with more extensive systemic manifestation (large B-cellNHL), where chest, abdomen and pelvis presented with extensivelesions. Generally, renal lymphoma is not clinically evident; most oftimes it is detected in the imaging evaluation or follow-up ofpatients with lymphoma. NHL is considerably more frequent thanHL, notwithstanding the similarity between imaging findings.Renal lymphoma is extremely rare, since normally lymphatic tissueis absent in the kidney. Renal involvement may occur by directcontiguous or hematogenic dissemination. In about 50% of cases,renal lymphoma is a recidivation in patients with previouslytreated lymphomas. Distinct, solid masses are frequent, andgenerally are homogeneous and isodense in relation to the renalparenchyma in pre-contrast images, although some times they maypresent slightly lower or higher densities. A significantly lowerhomogeneous enhancement (10 UH to 30 UH) than the renalparenchyma enhancement is typical after contrast injection.Necrosis or calcification frequently occurs after the therapy.Extension to the perirenal space occurs in 40% of patients withrenal lymphoma, and some times this is the only manifestation ofthe disease, possibly in the form of multiple distinct nodules inthe perirenal fat(5,12,15).
CONCLUSION Computed tomography is an invaluable tool for the diagnosis,staging and follow-up of lymphomas, with alert findings such aslymph node masses (especially the mediastinal ones),hepatosplenomegaly, unilateral tonsilar mass, and parietalthickening of intestinal loop.
REFERENCES 1. Johnston JM, Sakamoto K, Windle ML, Cripe TP, Gross S, Coppes MJ. Non-Hodgkin lymphoma. Acesso em: 10/6/2005. Disponível em: http://www.emedicine.com/ped/topic1343.htm [ ] 2. Juhl JH. Linfoma. In: Juhl JH, editor. Interpretação radiológica. 7ª ed. Rio de Janeiro: Guanabara Koogan, 2000;200–215. [ ] 3. Kirks DR, Griscon NT. Diagnóstico por imagem em pediatria e neonatologia. 3ª ed. São Paulo: Revinter, 2003. [ ] 4. Associação Brasileira de Linfoma e Leucemia – Abrale. Linfoma de Hodgkin. Acesso em: 15/6/2005. Disponível em: http://www.abrale.com.br [ ] 5. Glazer HS, Semenkovich JW, Gutierrez FR. Mediastino. In: Lee JKT, Sagel SS, Stanley RJ, Heiken JP, editores. Tomografia computadorizada do corpo em correlação com ressonância magnética. 3ª ed. Rio de Janeiro: Guanabara Koogan, 2001;263–268. [ ] 6. Bernard A, Murphy SB, Melvin S. Neoplasias e estruturas semelhantes a neoplasias. In: Behrman RE, Kliegman RM, Nelson WE, editores. Tratado de pediatria. 15ª ed. Rio de Janeiro: Guanabara Koogan, 2000;1977–1822. [ ] 7. Effmann EL. The mediastinum. In: Kuhn JP, Slovis TL, Haller JO, editors. Caffey's pediatric diagnostic imaging. 10th ed. Philadelphia: Mosby, 2004;1649–1690. [ ] 8. Guermazi A, Brice P, de Kerviler EE, et al. Extranodal Hodgkin disease: spectrum of disease. RadioGraphics 2001;21:161–179. [ ] 9. Fishman EK, Kuhlman JE, Jones RJ. CT of lymphoma: spectrum of disease. RadioGraphics 1991;11:647–669. [ ] 10. Marchiori E, Valiante PM, Gutierrez ALTM, Bodanese L, Souza Jr AS. Linfomas pulmonares: correlação da tomografia computadorizada de alta resolução com a anatomopatologia. Radiol Bras 2002;35:1–6. [ ] 11. Dunleavy KM, Waes CV, Kass E, Grill R. Lymphomas of the head and neck. [update 2004 Aug 19]. Acesso em: 10/6/2005. Disponível em: http://www.emedicine.com/ent/topic742.htm [ ] 12. Cohan RH, Baber ME, Cooper C, Moore JO, Dunnick NR. Retroperitoneal cavity. In: Wegener OH, editor. Whole body computed tomography. 2nd ed. Oxford: Blackwell Sci Publ, 1993;471–477. [ ] 13. Byun JH, Ha HK, Kim AY, et al. CT findings in peripheral T-cell lymphoma involving the gastrointestinal tract. Radiology 2003;227:59–67. [ ] 14. Mulligan ME. Lymphoma, bone. [update 2005 Jan 5]. Acesso em: 10/6/2005. Disponível em: http://www.emedicine.com/radio/topic819.htm [ ] 15. Shirkhoda A. Kidney, lymphoma. [update 2005 Jan 19]. Acesso em: 9/6/2005. Disponível em: http://www.emedicine.com/radio/topic373.htm [ ]
Received May 19, 2006.
* Study developed in the Computed Tomography Unit at Centro Universitário de Controle do Câncer do Hospital Universitário Pedro Ernesto (HUPE) da Universidade do Estado do Rio de Janeiro (UERJ), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554