Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 40 nº 2 - Mar. / Apr. of 2007
Vol. 40 nº 2 - Mar. / Apr. of 2007
|
ORIGINAL ARTICLE
|
|
Parosteal osteosarcoma: conventional radiology findings |
|
|
Autho(rs): Francisco Nanci Neto, Edson Marchiori, Alberto Domingues Vianna, Ierecê Lins Aymoré, Ana Luiza Brito de Almeida, Klaus L. Irion, Felipe Birchal Collares |
|
|
Keywords: Parosteal osteosarcoma, Bone radiology |
|
|
Abstract:
Francisco Nanci NetoI; Edson MarchioriII; Alberto Domingues ViannaIII; Ierecê Lins AymoréIV; Ana Luiza Brito de AlmeidaV; Klaus L. IrionVI; Felipe Birchal CollaresVII IMD, Radiologist at Clínica de Diagnóstico por Imagem – CDPI, Rio de Janeiro, RJ, Brazil
INTRODUCTION Osteosarcoma is a tumor arising from the osteogenic matrix,and is the most frequent primary malignant tumor of bone inyoungsters(1). It may be localized inside or onthe surface of the bone; and in this case it may occur in thecortical bone (intracortical), in adjacent soft tissues(extra-osseous), or in the periosteum(juxtacortical)(2). Juxtacortical osteosarcomas are rare (8%–10% of allosteosarcomas)(1) and can be classified into:parosteal, periosteal and high-grade surfacetypes(3,4). These types are characterizedaccording their origin, respectively from the external periosteallayer, internal periosteal layer, or from any site of theperiosteum, but histologically identical to the conventionalosteosarcoma(2). On its turn, parostealosteosarcomas can be subdivided into conventional anddedifferentiated(1,5,6). Parosteal osteosarcoma is the most common subtype ofjuxtacortical osteosarcomas, accounting for 75% of them, with abetter prognosis(7). The incidence is highestin the third and fourth decades of life(8–10)most frequently affecting women(7,9–12). Itsmost frequent presentation is a mildly painfulmass(7,13,14) in the posterior distal region ofthe femur(12,15,16). Occasionally, areas ofdedifferentiation for a high grade sarcoma may arise inside apre-existent low-grade lesion, both at the tumor presentation(synchronic), and after one or more recurrences (metachronic), inthis case with worse prognosis(7,11,16–19). Generally, histological findings associated with conventionalx-ray are distinctive, allowing differentiation between parostealosteosarcoma and other surface osteosarcomas as well as otherlesions with which they are frequently confused. Prognosis andmanagement are determined by the extent and histological grade ofthe tumor(20). The objective of the present study was to analyze the mostsignificant clinical findings of parosteal osteosarcoma, and todescribe the most frequent findings on conventionalradiology.
MATERIALS AND METHODS A retrospective study was performed including 26 cases ofpatients (nine males, 16 females, one unspecified) diagnosed withparosteal osteosarcoma from the archives of Clube do Osso (BoneClub), in Rio de Janeiro, RJ, Brazil, gathering up radiologicaland anatomopathological documentation of more than 6,000 cases ofbone diseases. The patients came from several public and privatehospitals and clinics, in the period between 1960 and 1995, withhistopathological confirmation of parosteal osteosarcoma. The patients' dossiers were reviewed for collection of datasuch as sex, signs and symptoms, as well as symptoms duration atthe moment of the diagnosis. Plain films of the 26 patients were evaluated, and thefollowing main aspects of the lesion were defined: localizationin relation to the affected bone and preferential region; shape;margins; interface with the adjacent cortex, mineralizationpattern and presence of medullary invasion, radiolucent line andperiosteal reaction.
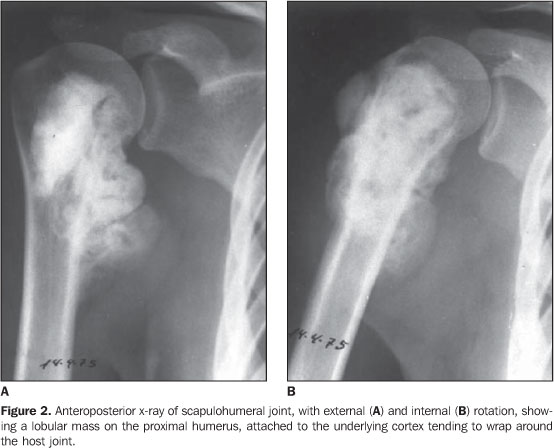
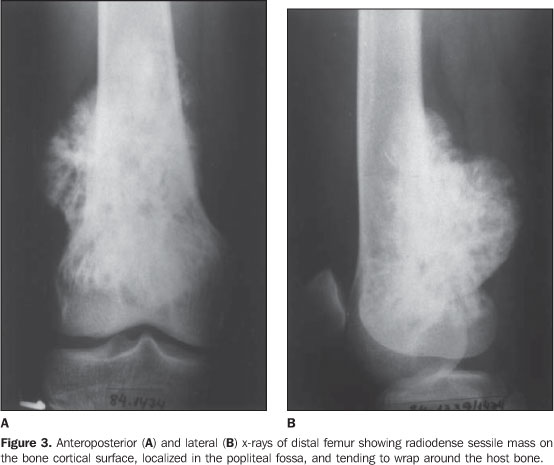
RESULTS a) Clinical considerations The mean age of the patients was approximately 23.6 years, theoldest patient with 47 years and the youngest with six years ofage. The peak of incidence occurred in the second and thirddecades of life, with 17 patients (65.4%) in this age range. As regards the sex of the patients, 16 were female (61.5%),nine male (34.6%), and in one case this information wasunavailable. Therefore, women were preferentially affected with amale-to-female ratio of 1:2. Information on signs and symptoms were available for 23 cases.The most frequent clinical finding was increase in local volumeof the tumor which was visible or palpable in 18 patients(78.3%); in seven patients, the tumor was painless. Pain in theaffected site was the second most frequent clinical finding,present in 16 (69.6%) patients; five of these latest presentedonly pain. Also, limitation of the adjacent joint movementamplitude was observed in four cases (17.4%) and report of aprevious trauma in five cases (21.7%). The duration of symptoms until the moment of the diagnosis wasquite variable. Of the 19 patients whose information wereavailable, 11 presented symptoms for one to twelve months, sevenfor one to five years, and one patient had symptoms for more thanfive years. No patient presented symptoms for less than onemonth. b) Radiological findings The evaluation of all the 26 patients was based onconventional radiology findings. As regards the skeletal tumor location, the most frequent sitewas the distal femur in 16 cases (61.5%), 11 of these cases(68.7%) with involvement of the distal posterior femoral region(popliteal fossa). The second most frequent site was the proximal tibia, withfour cases (15.4%), followed by the middle femur with two cases(7.7%), one of them in the femoral amputation stump, and theproximal humerus, also with two cases (7.7%). The two remainingtumors originated respectively from the distal fibula andproximal femur (7.7%). Therefore, all the tumors occurred in theappendicular skeleton, and 20 patients (76.9%) presented a tumoraround the knee. Twenty-four tumors (92.3%) involved the metaphysis: 11 weremetaphyseal and diaphyseal, five affected only the metaphysis,six affected all the regions, and two were metaphyseal andepiphyseal. The two remaining tumors were exclusivelyepiphyseal. The typical radiographic finding present in all of the caseswas an ovoid or spherical mass, with bone density and in closejuxtaposition to the bone surface. In 13 (50%) cases the tumors were seen as lobular masses (Figures 1 and 2), with irregular margins in ten cases (38.5%) e smooth margins in three cases (11.5%).
The majority of tumors (88.5%) appeared as a mass attached tothe underlying cortical bone, and the smallest ones presentedwith smaller areas of cortical adhesion, but as the tumor grewthey also increased. Because of overlapping between tumor andhost bone, the adherence areas could not be evaluated in threecases (11.5%). The small lesions were eccentric and, as the tumor increased, tending to wrap around the host bone (Figures 2 and 3). This has occurred in 20 cases (76.9%). This trend to wrap around the bone led to the radiolucent line obliteration; also, because of structures overlapping, the identification of possible medullary invasion, besides the previously mentioned cortical adhesion by means of conventional x-ray became difficult.
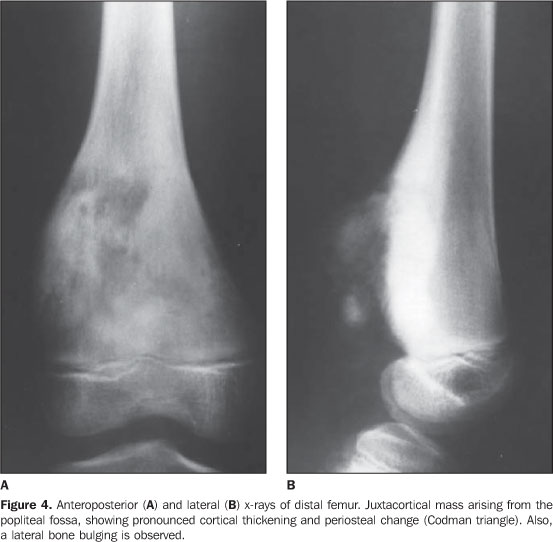
In 24 patients (92.3%) there was reactive sclerosis of the adjacent cortex, resulting in cortical thickening (Figure 4).
A radiolucent line between the tumor and the adjacent cortex,except in the area of the tumor attachment to the cortex, wasobserved in 13 cases (50%). The classical pattern of tumor mineralization — a denser mineralization on the base than in the periphery of the tumor (Figures 1, 2 e 3) — was found in 42.3% of cases. Other mineralization patterns found were: amorphous pattern (23.1%), uniform pattern (23.1%) and lobulated pattern (11.5%). Periosteal reaction was present in four cases (15.4%) with formation of a Codman's triangle (Figure 4) in two, and periosteal thickening with calcification (Figure 5) in one case.
Finally, it is important to note that although there is noreport on follow-up for the majority of patients, three casescorresponded to local recidivation.
DISCUSSION Osteogenic sarcomas (osteosarcomas) are the most frequentmalignant bone tumors in children and young adults, constitutingabout 15% of primary bone tumors(21). Othermost common bone sarcomas are chondrosarcoma and Ewing'ssarcoma(22–24). In the present study, the mean age of the patients wasapproximately 23.6 years, with peak of incidence in the secondand third decades of life. This finding was a little differentfrom the majority of published studies, where the peak ofincidence occurs ten years latter, in the third and fourthdecades of life(2,4,9,11,20,25,26). Schajowiczet al.(4), have studied 64 cases with 81% ofthe patients with more than 20 years of age, while Jelinek etal.(27) have reported a mean age of 31 years (n= 60). Okada et al.(13), who have presented thelargest casuistic in the literature, with 226 cases, reported amean age of 28 years, similarly to Temple etal.(9), with 38 patients (mean age = 28.9years), Johnson et al.(25), with 33 patients(mean age = 33 years), and Cassone et al.(26),with 29 patients (mean age = 25.3 years). As regards the patient's sex, women were preferentiallyaffected — 61.5% women (n = 16), 34.6% men (n = 9) and onepatient whose sex was not reported —, with a 2:3 men/womenratio. This higher female prevalence is in agreement with severalauthors(2,4,7,9,12,13), with a similar 2:3men/women ratio reported by Okada et al.(13) (n= 226). Regarding signs and symptoms, in the present casuistic, themost frequent clinical findings were increase in local volume ofthe tumor in 18 patients (78.3%), local pain in 16 (69.6%). Also,limitation of the adjacent joint movement amplitude was observedin four cases (17.4%), and report of previous trauma in fivecases (21.7%) These clinical findings are similar to thosedescribed by several other studies(2–4,7, 13,14,26). Okada et al.(13) havereported the following symptoms as the most frequently found:localized edema in 54% of patients (n = 102), and pain in 35% (n= 66); the following signs have been observed: a mass in 86% ofpatients (n = 81), and limitation of the adjacent joint movementamplitude in 33% of cases (n = 31). There was a history ofprevious trauma in only 19 cases (8.4%). According to Schajowiczet al.(4), a trauma just attracts attention toalready existing lesions, rather than causing them to appear. In the present study, all the tumors were situated in longtubular bones, the popliteal fossa being the most frequent site(40% of cases). This finding is in agreement with all the otherseries(1,7,12,14,20,25–27). Also, 76% of thelesions involved bones around the knee, a rate similar to thosereported by Resnick et al.(3) and Spina etal.(1) (70%), and Johnson etal.(25) and Cassone etal.(26) (72%). The preference of the tumor for a specific site in the boneaffected was a remarkable characteristic of parostealosteosarcoma. The metaphysis was affected by 92.3% of tumors, and7.7% were restricted to the diaphysis. These percentages are inagreement with the expected ratios; Partovi etal.(16) have reported 90% of lesions involvingthe metaphysis, and 10% involving only the diaphysis, while Okadaet al.(13) have found respectively 91% and 9%.Both the present study and other studies in the literature, havefound no tumor restricted to the epiphyseal region. Temple et al.(9), with a 38-patientcasuistic, have radiographically described all the lesions asdensely mineralized and in close juxtaposition to the bonesurface. These features we also observed in all the cases in thepresent study. Okada et al.(13), evaluating 226 patients,demonstrated that the most frequently found external edge oftumors was the lobulated one (60%), followed by irregular edges(17%) and smooth edges (16%). In the present study, similarresults were found, the lobulated edge being the most frequentlyfound (50%), irregular (38.5%), and smooth (11,5%), lessfrequently found. These results are in agreement with otherstudies in the literature(1,4,11,15,27),generally describing these tumors with lobulated or irregularmargins. Twenty-three of the 26 tumors (88.5%) were attached to thebone cortex; and in three of them (11.5%) the adhesion could notbe evaluated because of overlapping between the lesion and thehost bone. Okada et al.(13) have reported 70%of tumors attachment to the underlying bone cortex, and in 24% oftumors this attachment could not be evaluated due the same abovementioned reasons. In 76% of cases, the tumor involved the bone as its sizeincreased, likewise in several otherstudies(3,11,15,20,27). Hudson et al.(28) and Pérez etal.(11) have reported an irregular thickeningof the adjacent cortex, which was also observed in 92.3% ofpatients in the present study. Okada etal.(13), with 226 patients, have reportedcortical thickening in only 29% of cases. In the present study, intramedullary extension of the tumorcould not be found. In their study, Okada etal.(13) mentioned that the medullaryinvolvement was more clearly seen on computed tomography ormagnetic resonance imaging, evidenced in 37 (22%) patientsevaluated in transverse sections. In the present casuistic, a radiolucent line between the tumorand the adjacent bone was observed in 13 cases (50%), with atendency to obliteration in tumors involving the bone. This facthas been reported by severalauthors(3,11,15,20,27); Okada etal.(13) have observed this radiolucent line in58% of 226 lesions, with difficulty in identifying it byconventional radiology in the remaining lesions because ofstructures (tumor and adjacent bone) overlapping. Some authors(2,3,18) have described aclassical lesion mineralization pattern, denser on the base thanin the periphery; in the present study this pattern was found in42.3% of cases (n = 11). Also, an amorphous pattern ofmineralization was found in 23.1% of patients, a uniform patternin 23.1%, and a lobulated pattern in 11.5%. Okada etal.(13) have observed this classical pattern ofmineralization in a still lower percentage, only 15%. The periosteal reaction, absent in the majority of casesaccording to some authors(2,11,26), wasobserved in only four cases in the present study (15.4%). Asimilarly low rate was reported by Okada etal.(13), with only 6% of tumors presentingperiosteal reaction. In summary, the main findings of conventional radiology in allof the cases were a densely mineralized lesion in closejuxtaposition to a bone surface, with the adjacent cortexirregularly thickened, besides areas of cortical attachment andirregular and lobulated margins. Also, a radiolucent line betweenthe tumor and the adjacent bone was typically evidenced, besidesa denser mineralization pattern on the base than in theperiphery, and a mild periosteal reaction.
REFERENCES 1. Spina V, Montanari N, Romagnoli R. Malignant tumors of the osteogenic matrix. Eur J Radiol 1998;27(Suppl 1):S98–109. [ ] 2. Kenan S, Abdelwahab IF, Klein MJ, Hermann G, Lewis MM. Lesions of juxtacortical origin (surface lesions of bone). Skeletal Radiol 1993;22: 337–357. [ ] 3. Resnick D. Diagnosis of bone and joint disorders. 3rd ed. Philadelphia: WB Saunders, 1996;3662–3697. [ ] 4. Schajowicz F. Neoplasias ósseas e lesões pseudotumorais. 2ª ed. Rio de Janeiro: Revinter, 2000;71–130. [ ] 5. Sheth DS, Yasko AW, Raymond AK, et al. Conventional and dedifferentiated parosteal osteosarcoma. Diagnosis, treatment, and outcome. Cancer 1996;78:2136–2145. [ ] 6. David A, Rios RA, Tarragô RP, et al. Indicação de ressecção radical em sarcoma parosteal. Rev Bras Ortop 1995;30:801–804. [ ] 7. Abdelwahab IF, Kenan S, Hermann G, Klein MJ. Dedifferentiated parosteal osteosarcoma of the radius. Skeletal Radiol 1997;26:242–245. [ ] 8. Lin J, Yao L, Mirra JM, Bahk WJ. Osteochondroma-like parosteal osteosarcoma: a report of six cases of a new entity. AJR Am J Roentgenol 1998; 170:1571–1577. [ ] 9. Temple HT, Scully SP, O'Keefe RJ, Katapurun S, Mankin HJ. Clinical outcome of 38 patients with juxtacortical osteosarcoma. Clin Orthop Relat Res 2000;(373):208–217. [ ] 10. Meohas W, Smith J, Aymoré IL, et al. Osteossarcoma parosteal de escápula. Rev Bras Ortop 2003;38:561–566. [ ] 11. Pérez MG, Peinador AM, Moya AB, et al. Osteosarcoma yuxtacortical. Rev Clín Esp 1990;187–189. [ ] 12. Picci P, Campanacci M, Bacci G, Capanna R, Ayala A. Medullary involvement in parosteal osteosarcoma. A case report. J Bone Joint Surg Am 1987;69:131–136. [ ] 13. Okada K, Frassica FJ, Sim FH, Beabout JW, Bond JR, Unni KK. Parosteal osteosarcoma. A clinicopathological study. J Bone Joint Surg Am 1994; 76:366–378. [ ] 14. Wines A, Bonar F, Lam P, McCarthy S, Stalley P. Telangiectatic dedifferentiation of a parosteal osteosarcoma. Skeletal Radiol 2000;29:597–600. [ ] 15. Edeiken J, Farrell C, Ackerman LV, Spjut HS. Parosteal sarcoma. Am J Roentgenol Radium Ther Nucl Med 1971;111:579–583. [ ] 16. Partovi S, Logan PM, Janzen DL, O'Connel JX, Connel DG. Low grade parosteal osteosarcoma of the ulna with dedifferentiation into high-grade osteosarcoma. Skeletal Radiol 1996;25:497–500. [ ] 17. Haeckel C, Ayala AG, Radig K, Raymond AK, Roessner A, Czerniak B. Protease expression in dedifferentiated parosteal osteosarcoma. Arch Pathol Lab Med 1999;123:213–221. [ ] 18. Shuhaibar H, Friedman L. Dedifferentiated parosteal osteosarcoma with high-grade osteoclast-rich osteogenic sarcoma at presentation. Skeletal Radiol 1998;27:574–577. [ ] 19. Bertoni F, Bacchini P, Staals EL, Davidovitz P. Dedifferentiated parosteal osteosarcoma: the experience of the Rizzoli Institute. Cancer 2005; 103:2373–2782. [ ] 20. Levine E, De Smet AA, Huntrakoon M. Juxtacortical osteosarcoma: a radiologic and histologic spectrum. Skeletal Radiol 1985;14:38–46. [ ] 21. Pinho MC, Lima GAF, Rodrigues MB. Osteossarcoma periosteal (Qual o seu diagnóstico?). Radiol Bras 2005;38(6):VII–IX. [ ] 22. Oliveira GA, Werlang HZ, Bergoli PM, Frechiani M, Oliveira F. Tomografia computadorizada na análise dos padrões de calcificação nos tumores ósseos da bacia em pediatria: nova abordagem. Radiol Bras 2006;39:413–418. [ ] 23. Gomes ACN, Silveira CRS, Paiva RGS, Aragão Jr AGM, Castro Jr JRC. Condrossarcoma em paciente com osteocondromatose múltipla: relato de caso e revisão da literatura. Radiol Bras 2006;39: 449–451. [ ] 24. Catalan J, Fonte AC, Lusa JRB, Oliveira AD, Melo ES, Gonçalves CM. Sarcoma de Ewing: aspectos clínicos e radiográficos de 226 casos. Radiol Bras 2005;38:333–336. [ ] 25. Johnson K, Davies AM, Evans N, Grimer RJ. Imaging recurrent parosteal osteosarcoma. Eur Radiol 2001;11:460–466. [ ] 26. Cassone AE, Camargo PO, Croci AT, Oliveira CRGMC. Osteossarcoma parosteal: avaliação clínica, radiográfica, anatomopatológica e fatores de prognóstico em 29 casos operados. Rev Bras Ortop 1998;33:867–875. [ ] 27. Jelinek JS, Murphey MD, Kransdorf MJ, Shmookler BM, Malawer MM, Hur RC. Parosteal osteosarcoma: value of MR imaging and CT in the prediction of histologic grade. Radiology 1996; 201:837–842. [ ] 28. Hudson TM, Springfield DS, Benjamin M, Bertoni F, Present DA. Computed tomography of parosteal osteosarcoma. AJR Am J Roentgenol 1985;144:961–965. [ ]
Received May 5, 2006.
* Study developed at Department of Radiology – Universidade Federal do Rio de Janeiro (UFRJ) and at Clube do Osso (Bone Club), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554