Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 41 nº 4 - July / Aug. of 2008
Vol. 41 nº 4 - July / Aug. of 2008
|
ORIGINAL ARTICLE
|
|
Post-operative evaluation of endovascularly treated abdominal aortic aneurysms by multidetector computed tomography angiography |
|
|
Autho(rs): Fabiana Barroso Thomaz, Gaudencio Espinosa Lopez, Edson Marchiori, Fabio Vargas Magalhães, Isabela Ferreira de Magalhães, Iugiro Roberto Kuroki, Mônica Ferreira Caramalho, Romeu Côrtes Domingues |
|
|
Keywords: Aortic aneurysm, Endovascular repair, Postoperative complications, Tomography, Radiology |
|
|
Abstract:
ISpecialist Title by Colégio Brasileiro de Radiologia e Diagnóstico por Imagem (CBR), MDs, Radiologists at the Unit of Computed Tomography of Clínica de Diagnóstico Por Imagem (CDPI), Rio de Janeiro, RJ, Brazil
INTRODUCTION In the recent years, the therapeutic approach to aortic aneurysms has undergone deep changes in previously established therapy concepts. Great and continuous developments in endovascular surgery have not only expanded the options for interventional treatment but also have led to a rediscussion of surgical indications. For many years, open surgery remained as the sole option for treating aortic aneurysms. In 1969, Dotter(1) introduced the concept of endoluminal management of aortic aneurysms. Many studies approaching different types of prostheses were developed with animal models. In 1990, Parodi et al.(2) performed for the first time an endoluminal repair of abdominal aortic aneurysms. Currently, endovascular prostheses represent an alternative approach to open surgery for patients with thoracic or abdominal aortic aneurysms, depending on their morphology and general clinical conditions of the patient. Multidetector computed tomography angiography is a useful tool in the assessment of endovascularly treated patients by following-up the aneurysm size, endograft morphology and positioning, and detecting possible complications such as endoleak, graft migration, thrombosis, graft angulation, occlusion, dissection, hematomas, and pseudoaneurysm at the site of arteriotomy. The present study is aimed at the postoperative evaluation of endovascularly treated abdominal aortic aneurysms by multidetector computed tomography angiography, identifying and characterizing the main complications associated with the procedure.
MATERIALS AND METHODS Angiotomographic studies of 166 patients were retrospectively evaluated. The sample included 137 men and 29 women with ages ranging between 47 and 89 years (mean, 73 years) with endovascularly treated abdominal aortic aneurysms at Clínica de Diagnóstico Por Imagem (CDPI), Rio de Janeiro, RJ, Brazil, in the period between June 2005 and August 2006. The first postoperative follow-up was performed at about the 30th postoperative day. Studies were performed in multidetector Brilliance, 64-channel tomograph (Philips; Eindhoven, The Netherlands), adopting the following parameters: collimation, 0.625 mm; pitch, 0.6–1; mAs, 300–400; kV, 120. In all of the cases, a nonionic iodinated contrast agent (350 mg/ml concentration) was injected via peripheral venous access by infusion pump at a rate of 4 –5 ml/s and a variable amount of 70–100 ml. Contrast delay was managed through bolus tracking and contrast agent volume was calculated by multiplying the sum of the spiral acquisition time with a post-threshold delay of 150 UH in the abdominal aorta by the flow rate. Immediately after contrast agent administration, a saline solution was injected to aid in the contrast medium column progression, with the volume similarly calculated by multiplying the same flow rate by the time required to reach the right atrium (12–15 seconds). Aiming at evaluating the first postoperative follow-up, a noncontrast-enhanced phase focused on a segment limited to the endograft, 0.625 collimation and pitch 0.6–1. In some cases, a delayed phase was added immediately after the end of the contrast-enhanced phase. Axial images were underwent post-processing in workstations (Extended Brilliance Workspace), utilizing multiplanar reconstruction (MPR), volume rendering technique (VRT) and, occasionally, maximum intensity projection (MIP). The minimal morphometric study included the measurement of the aorta diameter at the proximal fixation ring and the maximum aneurysmal diameters. Other measurements were eventually performed in the presence of complications. The images were independently analyzed by two radiologists, with the final results being reached by consensus. The presence of the following findings was considered: endoleak, angulation, thrombosis, endograft migration, access vessel dissection or collections at the inguinal access site.
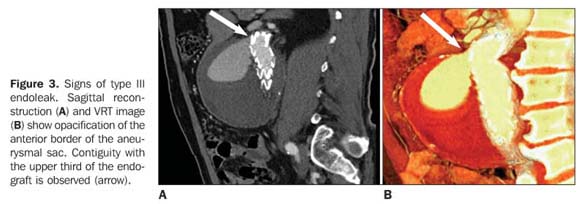
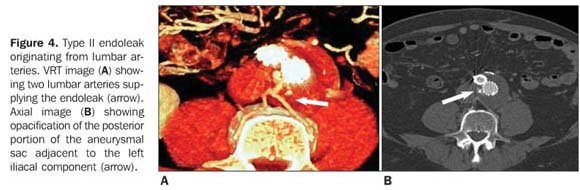
RESULTS Among the 166 cases, 93 patients did not present any complication, and 73 presented the following findings: endoleak (n = 37), thrombosis (n = 29), angulation (n = 17) (Figure 1), presence of collection at the puncture site (n = 10), graft migration (n = 7), access vessels dissection (n = 7) and occlusion (n = 6). Also, a case of aortoduodenal fistula was found. Endoleak was the most frequently found complication (n = 37), distributed as follows: six type I (Figure 2), 30 type II, and one type III (Figure 3). Two of these 37 patients with endoleaks presented with more than one type (types I and II); four patients presented an increase in the aneurysmal diameter ranging between 3mm and 19 mm. A supplying vessel was identified in ten of the patients (33%) with type II endoleak (Figure 4).
The second most frequent complication was the presence of laminar thrombus lining the internal circumference of the endograft in 29 patients of the present series (17.47%). These cases were characterized by a laminar thrombus in the endograft body, with no significant luminal reduction (Figure 5). In six cases thrombosis was found in one of the iliac branches of the endograft with vascular lumen occlusion.
The third most frequent complication was graft angulation (Figure 5), observed in 17 cases (10.24% of the total sample), six of them with inferior migration of the proximal ring. In four cases, the authors could analyze the preoperative morphometric studies, observing two types of proximal neck predisposing to complications: a short proximal neck with about 90° angulation to the left in the first patient, and a conical neck with laminar thrombus in the second one, besides juxtarenal bilobular aneurysm in the other two patients.
DISCUSSION The management of abdominal aortic aneurysms by endovascular graft implantation has increasingly been utilized as an effective alternative to conventional open surgery, reducing considerably the morbimortality(3). The most relevant determining factor in the success of endovascular procedures is aneurysmal dimensions stabilization or regression achieved by complete blood flow exclusion in the aneurysmal sac. Computed tomography angiography is considered as the method of choice in the postoperative follow-up of patients submitted to endovascular management of abdominal aortic aneurysms, considering the highest sensitivity of this imaging technique in the detection of possible complications, besides being a rapid, safe and non-invasive method(4). With the introduction of multidetector computed tomography, other resources were added to the advantages of angiotomography, enabling extremely short acquisition times, minimizing motion artifacts, optimizing the utilization of contrast agents, and allowing the acquisition of thicker slices resulting in axial images and three-dimensional and multiplanar reconstruction with a higher quality(5). The postoperative follow-up is focused particularly on measurements of the aneurysm and proximal fixation ring, the stent-graft positioning and morphology, the contrast medium column, and the presence of extraluminal opacification (endoleak). Our study evaluated 166 patients submitted to endovascular treatment by different surgical teams, and procedure-related complications were observed in 73 patients. The presence of endoleak, defined as the persistence of blood flow into the aneurysm sac but outside the endoluminal graft, was the most frequent complication, present in 35patients – a result compatible with those reported in the literature. The incidence of endoleaks is estimated between 2.4% and 45.5% of endovascularly repaired infra-renal abdominal aortic aneurysms. Other study reports a prevalence of approximately 10% in the current practice, and 44% in cases where the previous technique was adopted(6). At computed tomography angiography, the type of endoleak is suggested by the configuration and location of the endoleak in relation to the endograft and to the aneurysm(7). Five different types of endoleaks are described, including blood flow into the aneurysm sac around the proximal or distal graft attachment sites (type I), retrograde flow from patent collateral vessels (type II), graft defect or rupture (type III), graft fabric porosity (type IV) and endotension, where the aneurysmal sac size increases and goes undetected at imaging studies (type V). In the study developed by Sicard & Rubin(8) with 450 patients, two (0.44%) presented endotension, requiring open surgery for the graft removal and subsequent conventional repair. During the surgery, increased intra-aneurysmal pressure and high pulsatility were observed. Type II endoleak is the most frequently found in the postoperative period. In the present study 41% of patients presented with this complication. In the studies developed by Tolia et al.(9) and Görich et al.(10) endoleaks were found respectively in 19% and 24% of cases. The meaning of type II endoleak is still under discussion, considering that this type of endoleak tends to present a benign and self-limited behavior(11). Despite of the fact of aneurysmal rupture secondary to type II endoleak being rare, increased aneurysmal pressure has been reported. Also, in the study developed by Sicard & Rubin(8), five (1.1%) of the 450 postoperative cases presented type II endoleaks progressing with increase in the volume of the aneurysmal sac and managed by means of embolization of afferent vessels. In the present study, only four (14%) of the 30 patients with type II endoleak presented increased aneurysmal sac. The second most frequent complication was the presence of a laminar thrombus lining the internal circumference of the endograft, observed in 29 patients included in the present study (17.47%) and in 3% to 19% of patients in the study developed by Tolia et al.(9). Thrombi are visualized as non-contrast-enhanced intraluminal round, or semi-lunar areas, with prognosis ranging from spontaneous resolution to complete graft thrombosis. The third most frequent complication was graft angulation, observed in 17 cases (10.24% of the total sample), six of them with inferior migration of the proximal ring. It is known that the evaluation of the proximal aneurysmal neck plays an essential role in the preoperative morphometric study. Endovascular procedures should by avoided in the following circumstances: proximal neck with > 26 mm in diameter and/or larger than the distal neck, distance of less than 15 mm between the lower renal artery and the aneurysm (short neck), proximal neck tortuosity (angle > 60°) and presence of extensive calcification and/or thrombus(8). In the above mentioned study developed by Tolia et al.(9), angulation and migration have been observed in 18% of cases. When voluminous aneurysms decrease in diameter after endograft deployment, a decrease in the aneurysmal length also occurs and may cause graft kinking. So, a distal graft migration may occur with dilatation of the aortic fixation ring, predisposing to the formation of type I endoleak (7). Access vessel dissection was found in seven cases (3.61% of patients), and may be related to tortuosity or parietal calcification of the iliac artery. These features may predispose to complications during the surgical procedures, requiring excessive strength to advance the release device causing intimal injury(4). Several authors have demonstrated that computed tomography angiography is the most sensitive imaging method for evaluating the outcomes of endovascular management of abdominal aortic aneurysms as well as for long term follow-up. Additionally, this method is rapid, safe and non-invasive. In summary, endoleak was the most prevalent complication in the present study, the type II being the most frequently found. The findings of the present study are quantitatively and qualitatively similar to the ones described in the literature(8–10).
REFERENCES 1. Dotter CT. Transluminally-placed coilspring endarterial tube grafts. Long-term patency in canine popliteal artery. Invest Radiol. 1969;4:329–32. [ ] 2. Parodi JC, Palmaz JC, Barone HD. Transfemoral intraluminal graft implantation for abdominal aortic aneurysms. Ann Vasc Surg. 1991;5:491–9. [ ] 3. Rydberg J, Kopecky KK, Lalka SG, et al. Stent grafting of abdominal aortic aneurysms: pre- and postoperative evaluation with multislice helical CT. J Comput Assist Tomogr. 2001;25:580–6. [ ] 4. Tillich M, Bell RE, Paik DS, et al. Iliac arterial injuries after endovascular repair of abdominal aortic aneurysms: correlation with iliac curvature and diameter. Radiology. 2001;219:129–36. [ ] 5. Hong C, Pilgram TK, Zhu F, et al. Coronary artery calcification: effect of size of field of view on multi-detector row CT measurements. Radiology. 2004;233:281–5. [ ] 6. Cademartiri F, Nieman K, van der Lugt A, et al. Intravenous contrast material administration at 16-detector row helical CT coronary angiography: test bolus versus bolus-tracking technique. Radiology. 2004;233:817–23. [ ] 7. Mita T, Arita T, Matsunaga N, et al. Complications of endovascular repair for thoracic and abdominal aortic aneurysm: an imaging spectrum. Radiographics. 2000;20:1263–78. [ ] 8. Sicard GA, Rubin BG. Endoluminal graft repair for abdominal aortic aneurysms. Adv Surg. 2003; 37:301–25. [ ] 9. Tolia AJ, Landis R, Lamparello P, et al. Type II endoleaks after endovascular repair of abdominal aortic aneurysms: natural history. Radiology. 2005;235:683–6. [ ] 10. Görich J, Rilinger N, Sokiranski R, et al. Leakages after endovascular repair of aortic aneurysms: classification based on findings at CT, angiography, and radiography. Radiology. 1999; 213:767–72. [ ] 11. Espinosa G, Ribeiro M, Riguetti C, et al. Six-year experience with talent stent-graft repair of abdominal aortic aneurysms. J Endovasc Ther. 2005;12:35–45. [ ] Received August 28, 2007. Accepted after revision October 23, 2007. * Study developed at Clínica de Diagnóstico Por Imagem (CDPI), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554