Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 6 - Nov. / Dec. of 2009
Vol. 42 nº 6 - Nov. / Dec. of 2009
|
CASE REPORT
|
|
Magnetic resonance imaging findings of intracranial gossypiboma: a case report and literature review |
|
|
Autho(rs): Michele Carneiro Brito Martins, Raquel Portugal Guimarães Amaral, Celi Santos Andrade, Leandro Tavares Lucato, Claudia da Costa Leite |
|
|
Keywords: Magnetic resonance imaging, Brain, Granuloma, Gossypiboma |
|
|
Abstract:
IMD, Radiologist, Trainee at Unit of Magnetic Resonance Imaging of Instituto de Radiologia do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InRad/HC-FMUSP), São Paulo, SP, Brazil
INTRODUCTION Several terms are utilized in the medical literature to describe an inflammatory process related to the presence of a foreign body(1). The term "gossypiboma" is utilized to describe a mass composed of a cotton matrix surrounded by an inflammatory/granulomatous reaction(1). The term gossypiboma originates from the Latin work gossypium (meaning cotton) and from the Kiswahili (a Tanzanian language) word boma (meaning place of concealment)(2). Other terms utilized are: textiloma, originated from the Latin textile (woven fabric) and associated with the suffix oma (that means tumor or edema); gauzoma (from surgical gauze); and muslinoma (from muslin, a woven cotton fabric)(1). Because of radiodense filaments present inside some materials, they can be readily visualized by means of conventional radiology and computed tomography (CT). However the image patterns at magnetic resonance imaging (MRI) are not completely known yet. Sometimes, small fragments of surgical material may not include radiodense filaments, making the direct identification by x-ray imaging methods more difficult. MRI represents an extremely useful tool in these cases(3,4). Also, there are bioresorbable materials that can develop inflammatory reactions and that are not radiodense. Depending on the clinical history of a patient, an exuberant inflammatory reaction may be confused with innumerable diseases such as recurrent tumors, radionecrosis, abscesses, hematomas, resoluting infarction, primary tumors or metastases(1). Aiming at avoiding wrong diagnoses, it is important to be familiarized with the appearance of an intracranial gossypiboma on MRI images. In the present report, the authors describe the magnetic resonance imaging patter of intracranial gossypiboma, which is relatively rare as compared with gossypibomas found following intra-abdominal and orthopedic surgeries(5). The objective of the present report is to warn of this diagnostic possibility and review the literature about the terminology and materials utilized during intraoperative procedures.
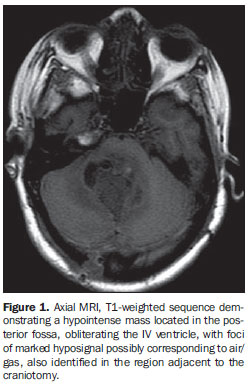
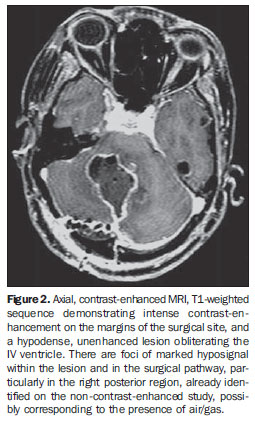
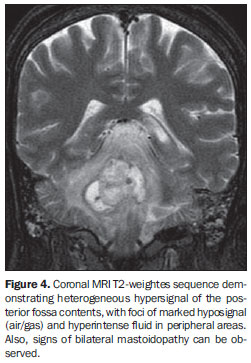
CASE REPORT Female, 33-year-old patient who had been diagnosed with supratentorial racemose intraparenchymal neurocysticercosis in the posterior fossa, affecting the IV ventricle, for six years. The patient was submitted to four surgeries along the last two years, the last one twenty days ago, in the posterior fossa. In the late postoperative period, the patient progressed with fever, decrease in the conscience level, and purulent secretion through the surgical wound. A CT was performed, demonstrating an expansile mass in the posterior fossa with intense enhancement after contrast administration. MRI demonstrated a hypointense mass in the posterior fossa on T1-weighted sequence, obliterating the IV ventricle, with foci of marked hyposignal compatible with the presence of air/gas. These foci were also present in the surgical pathway in the right posterolateral region (Figure 1). After contrast administration, enhancement was observed in the lesion margins and meninges adjacent to the craniotomy (Figure 2). On the contrast-enhanced sagittal T1-weighted image, one could identify the continuity of the lesion with the surgical pathway, extending towards the right posterolateral region of the posterior fossa, as well as the foci of marked hyposignal (air/gas) (Figure 3). On the coronal T2-weighted image, the lesion presented heterogeneous hypersignal with foci of marked hyposignal inside and peripheral areas filled with fluid (Figure 4). On T2-weighted and FLAIR sequences, hypersignal was observed in the adjacent cerebellar parenchyma as well as in the pons, mesencephalon, and cerebellar peduncles. The diffusion sequence demonstrated restricted diffusion of water molecules at some points of the lesion.
In association with the patient's clinical history, these findings strongly suggested the possibility of an inflammatory/granulomatous process with a mass in the surgical site probably corresponding to the presence of a foreign body (gossypiboma). The diagnostic hypothesis was postoperatively confirmed, with the finding of a fragment of surgical gauze involved by an inflammatory/granulomatous process. Therefore, the term gauzoma would be more appropriate than gossypiboma, considering that the latter is a more generic term.
DISCUSSION A wide variety of hemostatic agents may be utilized to avoid hemorrhages both during and after a surgical procedure. Resorbable and nonsesorbable materials may be utilized. As an example, the following nonresorbable materials can be mentioned: cotton gauze (causing gauzoma), rayon-based synthetic materials or muslin pieces (causing muslinoma). On the other hand, the most frequently utilized resorbable materials are the following: gelatin foam (Gelfoam®), oxidized cellulose (Surgicel®, Oxycel®) and microfibrillar collagen (Avitene®)(1), that may be left in place to avoid repetitive hemorrhages. Also, synthetic materials may be used as a dura mater substitute for repairing dural defects (Silastic®), besides copolymer chemotherapy wafers (Gliadel® wafers), several types of agents utilized for embolization of highly vascular tumors (Gelfoan® and Avitene®), and trisacryl gelatin microspheres and polyvinyl alcohol particles (embospheres)(1). Eventually, nonresorbable materials may be inadvertently left behind in the surgical field. All of such materials may elicit an inflammatory reaction(1). Nonresorbable materials may elicit two types of reaction(6). An exudative reaction leads to the development of an abscess with or without secondary bacterial infection. The inflammatory process may occur at the first day, and the granulomatous reaction, after one week. If the material is infected, an abscess and, consequently, a cutaneous draining fistula develop(3,7). On the other hand, resorbable agents elicit a physiological inflammatory process up to complete material reabsorption. In most of cases this process is asymptomatic. In the past, the inflammatory reaction involving hemostatic materials was named textiloma. However, this term should be utilized only for designating organic materials(5,7). An association of cotton based and synthetic materials has been widely utilized, so the term textiloma was replaced by "gossypiboma"(6,8). Additionally, the term textiloma is widely associated with general surgeries whose iatrogenically left material has implied medical/legal litigation. However, some authors support the use of the term textiloma considering its historical precedence in relation to gossypiboma(1). Asymptomatic presentations are accidentally found months or years after the surgery(9). In the present case, the patient presented symptoms at 20 days postoperatively. The exudative type of mass with a bacterial inflammatory process produces earlier symptoms than the fibrotic type(10). Gossypibomas present a variety of radiological patterns depending on the time the foreign body has remained in the surgical site, type of material utilized, and anatomic location. The MRI signal intensity depends on the quantity of fluid and protein present in the lesion. Studies have reported that MRI demonstrates a well circumscribed mass with hyposignal on T1-weighted images and hypersignal on T2-weighted images(3,7). A capsule with marked hyposignal is observed on T1- and T2-weighted images. However, other studies report the presence of strips of hyposignal on T2-weighted images compatible with gauze fibers, the typical and classic image of a gossypiboma(11,12). In the present case, neither a capsule nor strips with hyposignal similar to fibers were observed on T2-weighted images, corroborating the theory that gossypibomas presentation is really inconstant. On the diffusion sequence, there was restriction of water molecules in some foci, corresponding to high protein contents within the lesion, a characteristic that has been already described in the literature. The incidence of postoperatively found foreign bodies is of 0.01% to 0.001%. Among these cases, 80% are gossypibomas, 75% of them identified after intra-abdominal or pelvic surgery(3,7). However, such incidence is underestimated, considering the cases not reported because of medical/legal implications.
CONCLUSION All the classes of hemostatic agents may elicit inflammatory processes (gossypibomas), but such processes may mimic high-grade gliomas, radionecrosis, abscesses or other types of recurrent tumors. Therefore it is necessary to be alert to this diagnostic possibility(1). The identification and correct imaging evaluation are extremely important to define the surgical approach to this entity, provided it is correctly diagnosed.
REFERENCES 1. Ribalta T, McCutcheon IE, Neto AG, et al. Textiloma (gossypiboma) mimicking recurrent intracranial tumor. Arch Pathol Lab Med. 2004; 128:749-58. [ ] 2. Rajput A, Loud PA, Gibbs JF, et al. Diagnostic challenges in patients with tumors: case 1. Gossypiboma (foreign body) manifesting 30 years after laparotomy. J Clin Oncol. 2003;21:3700-1. [ ] 3. Kopka L, Fischer U, Gross AJ, et al. CT of retained surgical sponges (textilomas): pitfalls in detection and evaluation. J Comput Assist Tomogr. 1996;20:919-23. [ ] 4. Van Goethem JW, Parizel PM, Perdieus D, et al. MR and CT imaging of paraspinal textiloma (gossypiboma). J Comput Assist Tomogr. 1991; 15:1000-3. [ ] 5. De Marco JK, McDermott MW, Dillon WP, et al. MR appearance of postoperative foreign body granuloma: case report with pathologic confirmation. AJNR Am J Neuroradiol. 1991;12:190-2. [ ] 6. Olnick HM, Weens HS, Rogers JV Jr. Radiological diagnosis of retained surgical sponges. JAMA. 1955;159:1525-7. [ ] 7. Yamato M, Ido K, Izutsu M, et al. CT and ultrasound findings of surgically retained sponges and towels. J Comput Assist Tomogr. 1987;11:1003-6. [ ] 8. Williams RG, Bragg DG, Nelson JA. Gossypiboma: the problem of the retained surgical sponge. Radiology. 1978;129:323-6. [ ] 9. Kim HS, Chung TS, Suh SH, et al. MR imaging findings of paravertebral gossypiboma. AJNR Am J Neuroradiol. 2007;28:709-13. [ ] 10. Kominami M, Fujikawa A, Tamura T, et al. Retained surgical sponge in the thigh: report of the third known case in the limb. Radiat Med. 2003; 21:220-2. [ ] 11. Lo CP, Hsu CC, Chang TH. Gossypiboma of the leg: MR imaging characteristics - a case report. Korean J Radiol. 2003;4:191-3. [ ] 12. Nassar I, Mahi M, Semlali S, et al. Textilome intracranien. A propos dun cas. J Neuroradiol. 2004;31:148-9. [ ] Received January 23, 2008. * Study developed at Unit of Magnetic Resonance Imaging of Instituto de Radiologia do Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (InRad/HC-FMUSP), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554