Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 6 - Nov. / Dec. of 2009
Vol. 42 nº 6 - Nov. / Dec. of 2009
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Marcelo Souto Nacif, Karen Amaral do Vabo, Telmo Pimentel do Vabo, Ronaldo Maselli de Pinheiro Gouvêa, Ricardo Ebecken, Alair Augusto Sarmet Moreira Damas dos Santos |
|
|
IProfessor at Centro Universitário Serra dos Órgãos (Unifeso), Teresópolis, RJ, in charge of the Unit of Cardiac MRI at Hospital de Clínicas de Niterói (HCN), Niterói, RJ, Brazil
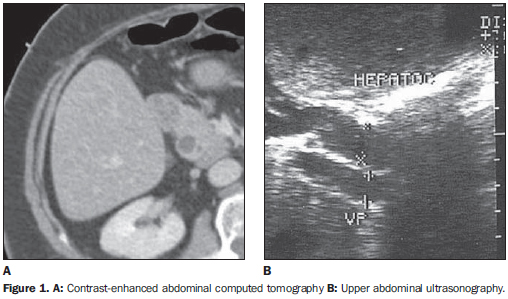
Female, 66 year-old patient complaining of stomach pain. On January 27, 2007, the patient presented a sudden, dull ache in the epigastric region, with no irradiation or trigger factor that improved with the use of symptomatic medication. The patient remained asymptomatic for approximately one month, when the epigastric pain returned upon ingestion of fatty food, but now with higher intensity, demanding emergency treatment. She denied vomiting, choluria, acholia or fever. Investigation on an out-patient basis was indicated for the suspicion of hepatitis, and the patient was submitted to abdominal ultrasonography and computed tomography. One week later, the patient presented a new episode of epigastric pain followed by vomiting, choluria and acholia, and on February 28, 2007 she was admitted to Hospital de Clínicas de Niterói, RJ, Brazil. During her hospital stay, the patient reported improvement of the algic symptomatology with null diet and underwent magnetic resonance cholangiography. The only relevant fact in the patient's previous history was a cholecystectomy ten years ago. At clinical examination, the only finding was jaundice (2+/4+). Laboratory tests demonstrated cholestasis indicators with high levels of bilirubin (remarkably direct bilirubin), TGO and TGP, as well as alkaline phophatase and gamma-GT. Also, CA- 19-9 serum levels were high. Serum amylase and lipase levels were normal. Images description Figure 1. A: Contrast-enhanced abdominal computed tomography B: Upper abdominal ultrasonography. The sonographic image (impaired by the excessive presence of intestinal gas) and the CT image demonstrate dilatation of the extrahepatic biliary tract. No abnormality is observed in the pancreatic duct and head.
Figure 2. A, B, C, D: Upper abdominal magnetic resonance cholangiography. A polypoid mass is observed in the major papilla of the duodenum, in association with choledocal dilatation with poorly faceted calculi. On the reconstructed image, distal interruption of the irregular lumen, neither abrupt nor filiform, is observed. Diagnosis: Adenoma in the hepatopancreatic ampulla.
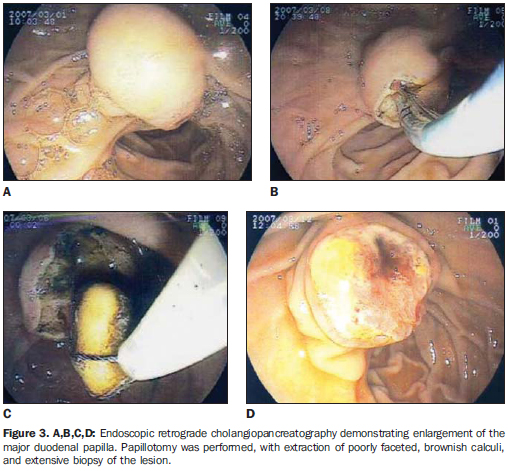
COMMENTS Adenomas are the most common tumors of the hepatopancreatic ampulla (0.04-0.12% of necropsies), being less frequently found than malignant lesions in this structure. Other benign tumors such as lipomas, hamartomas, fibromas and neurogenic tumors may be found in this region. Typically, these tumors do not present any sex predilection, and mean age of patients is about 60 years(1,2). These tumors may achieve 4 mm to 7 cm in size and, although extremely small tumors may be asymptomatic, 75% of patients are symptomatic at the moment of the diagnosis(1,3,4). The most frequent symptoms are the following: non-specific abdominal pain and jaundice (respectively 75% and 70%), besides digestive hemorrhage (50%). Laboratory tests demonstrate a cholestatic pattern of jaundice, with high levels of bilirubin - remarkably direct bilirubin -, gamma-GT and alkaline phosphatase. Intermittent episodes of pancreatitis are not infrequent and high CA 19-9 serum levels may be observed(5-7). Frequently, imaging findings demonstrate coexistence with biliary lithiasis, and a partial distal obstruction leading to a "double lumen" pattern (dilatation of the main biliary and pancreatic tract lumen), which has not been found in the present filling is observed as a single finding which is extremely non-specific in this region, and, also, the utilization of intravenous contrast media (either gadolinium or iodine) is quite controversial in the differentiation between malignant and benign tumors of this region(4,8). Considering that adenomas, particularly the villous ones, present a high malignization rate, a radical therapy must be considered for these patients (6,8). In summary, the imaging findings of the present case demonstrate a picture of dilatation of extrahepatic biliary ducts, with preserved main pancreatic ducts. Other finding is defective filling of the choledocal lumen compatible with the presence of poorly faceted and probably cholesterol-rich calculi (which cannot be seen at computed tomography). Additionally, a regular, "polypoid" mass is observed in the area of the hepatopancreatic ampulla leading to defective duodenal lumen filling, and determining a poorly regular transition with the choledocal lumen (neither abrupt nor filiform). Such mass measures approximately 3 cm, representing an argument against a non-neoplastic disease of this structure such as odditis (up to 1.5 cm) frequently secondary to calculi impaction. Thus, the suspicion of neoplastic lesion was raised, notwithstanding the finding of "primary" calculi (generally cholesterol-rich and moulded by the choledocal lumen) be poorly expected in periampullary malignant diseases which generally present a bad prognosis and extremely short survival. It is important to remember that residual calculi are generally faceted and usually cause complications within up to three years following cholecystectomy. The patient was submitted to endoscopic retrograde cholangiopancreatography with biopsy and excision of the lesion (Figure 3).
Final considerations As demonstrated in the present case, diagnostic suspicion may be raised even before histopathological examination by means of noninvasive methods in association with clinical and laboratory data in the search of a complete semiology of periampullary lesions, facilitating the therapeutic guidance. Adenoma in the hepatopancreatic ampulla must be considered by the radiologist in the differential diagnosis of lesions in this region.
REFERENCES 1. Buck JL, Elsayed AM. Ampullary tumors: radio-logic-pathologic correlation. Radiographics. 1993; 13:193-212. [ ] 2. Guibaud L, Bret PM, Reinhold C, et al. Bile duct obstruction and choledocholithiasis: diagnosis with MR cholangiography. Radiology. 1995;197:109-15. [ ] 3. Kim MJ, Mitchell DG, Ito K, et al. Biliary dilatation: differentiation of benign from malignant causes - value of adding conventional MR imaging to MR cholangiopancreatography. Radiology. 2000;214:173-81. [ ] 4. Asbach P, Klessen C, Kroencke TJ, et al. Magnetic resonance cholangiopancreatography using a free-breathing T2-weighted turbo spin-echo sequence with navigator-triggered prospective acquisition correction. Magn Reson Imaging. 2005; 23:939-45. [ ] 5. Schindera ST, Merkle EM. MR cholangiopancreatography: 1.5T versus 3T. Magn Reson Imaging Clin N Am. 2007;15:355-64. [ ] 6. Morita S, Suzuki K, Machida H, et al. Prospective trial of a navigator setting under left hepatic lobe on magnetic resonance cholangiopancreatography using a free-breathing prospective acquisition correction technique. Magn Reson Imaging. 2008;26:841-6. [ ] 7. Kim JH, Kim MJ, Chung JJ, et al. Differential diagnosis of periampullary carcinomas at MR imaging. Radiographics. 2002;22:1335-52. [ ] 8. Sugita R, Furuta A, Ito K, et al. Periampullary tumors: high-spatial-resolution MR imaging and histopathologic findings in ampullary region specimens. Radiology. 2004;231:767-74. [ ] Study developed at the Imaging Center of Hospital de Clínicas de Niterói (HCN) and at Department of Radiology - Universidade Federal Fluminense (UFF), Niterói, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554