Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 5 - Sep. / Oct. of 2009
Vol. 42 nº 5 - Sep. / Oct. of 2009
|
ORIGINAL ARTICLE
|
|
Evaluation of fetal cervical lymphangioma by magnetic resonance imaging and correlation with sonographic findings |
|
|
Autho(rs): Erika da Gloria Antunes, Heron Werner Junior, Pedro Augusto Daltro, Leise Rodrigues, Bruno Amim, Fernando Guerra, Romeu Côrtes Domingues, Emerson Leandro Gasparetto |
|
|
Keywords: Fetus, Lymphangioma, Cystic hygroma, Ultrasonography, Fetal magnetic resonance imaging |
|
|
Abstract:
IMD, Radiologist at Clínica de Diagnóstico Por Imagem (CDPI), Trainee at Multi-Imagem, Rio de Janeiro, RJ, Brazil
INTRODUCTION Lymphangiomas are congenital malformations of lymphatic vessels and constitute approximately 5% to 6% of all benign lesions in the childhood and adolescence(1,2),, occurring most frequently in the head, neck or axilla, although they may occur anywhere in the developing lymphatic system. No racial or sex predominance is reported, and the entity is subdivided into four histological types, cystic hygroma being the most frequently found(1,2). Although these lesions tend to involve and, sometimes, invade adjacent structures, they do not present malignant potential(1). In cases of isolated presentation, lymphangiomas have a good prognosis and most of times should be surgically resected. However, in cases of prenatal detection, it is important to perform a fetal karyotyping considering that lymphatic dysplasias are associated with chromosomal abnormalities(3). In such cases the prognosis is more reserved, so the prenatal diagnosis of lymphangiomas becomes extremely important, allowing a more appropriate counseling and treatment . Ultrasonography (US) is the method of choice for fetal evaluation because of its low cost, real-time capability and non-invasiveness, besides being easy to perform(4–7). Most of times, lymphangiomas are diagnosed at the second and third trimesters of gestation, and identified as multiseptated, thin-walled cystic masses in the fetal head and neck region(8). Magnetic resonance imaging (MRI) has been utilized as a valuable complementary method to US in the diagnosis of fetal malformations. The developments in the techniques of this imaging modality have revolutionized the assessment of pregnant women and fetuses, with increasingly rapid sequences and reduction of fetal motion artifacts(9). The examination can be performed without sedation and provides an excellent resolution of the fetal anatomy(4). In cases of lymphangiomas, the method determines more accurately the lesion extent and its relationship with the adjacent structures, allowing a more appropriate surgical planning. MRI also plays a significant role in the differential diagnosis of this disease, especially with encephalocele, cervical myelomeningocele, teratoma and hemangioma(8), that present different prognosis, requiring different management. The objective of the present study is to report three cases of cervical lymphangiomas in fetuses evaluated by routine US, and correlating the findings with alterations observed at fetal MRI.
MATERIALS AND METHODS The present study evaluated three pregnant women referred by Instituto Fernandes Figueira, Rio de Janeiro, after the finding of fetal cervical cystic mass at obstetric US. The patients were 20 years old (patient 1), 29 years old (patient 2) and 34 years old (patient 3), with mean age of 27 years, and underwent MRI one week after US with, respectively 24, 35 and 33 gestational weeks (mean 30.6 weeks). Subsequently, a new US study was performed for comparative purposes. The three patients were previously informed about the procedure and signed a term of free and informed consent. A 1.5 T Magnetom Avanto MRI unit (Siemens Medical Systems; Erlangen, Germany) was utilized, with the patients in dorsal or left lateral decubitus, feet first entry, and with a surface coil placed on their abdomen. The total examination time was, on average, 20 minutes, with acquisition of T1-weighted sequences (repetition time [TR], 201 ms; echo time [TE], 4.72 ms; field of view (FOV), 250–400 mm; matrix, 256 × 90–256) and T2-weighted HASTE (half-Fourier acquired single shot turbo spin echo) sequences (TR, 1000 ms; TE, 85–87 ms; FOV, 250–380 mm; matrix, 256 × 112–256) in the axial, coronal and sagittal planes of the fetuses with 3.0–7.0 mm-thick slices. The subsequent sonographic studies were performed immediately after the MRI studies, with Logic 500 and Voluson 730 US units (General Electric; Wisconsin, USA) with 3.5 MHz, 5.0 MHz and volumetric (3D and 4D) transducers. The MRI images were independently analyzed by the radiologist who performed the comparative US study and by a second radiologist, both with experience in fetal medicine, to evaluate the lesions site, size and extent, seeking a consensus on the establishment of a correlation between the findings of the two imaging methods utilized. The three patients had a Cesarean section between their 37th and 38th gestational weeks, and underwent postnatal follow-up. The newborns (two girls and one boy) were submitted to surgery right after the birth, except for one of them who was evaluated by MRI after one week of life to restudy the lesion extent, confirming the pre-natal findings. The three newborns were successfully submitted to surgery and had the diagnosis confirmed by means of histopathological evaluation.
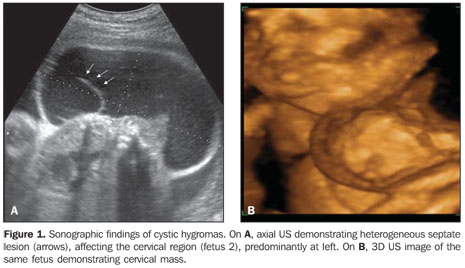
RESULTS All the lesions under suspicion of being cervical lymphangiomas at obstetric US were confirmed by MRI that, similarly to the previous and comparative US studies, evaluated the lesions site, size and content. All the lesions were located in the posterior cervical region, two of them at left (fetuses 1 and 3), and one at right (fetus 2). The lesions dimensions (lateral × transverse × anteroposterior) were 6.0 × 2.5 × 4.0 cm, 4.5 × 2.5 × 6.5 cm, and 11.0 × 2.0 × 5.0 cm, respectively in the fetuses 1, 2 and 3. As regards the lesions content, US demonstrated predominantly cystic lesions with thin septations inside (fetuses 2 and 3), and one was heterogeneous (fetus 1) (Figure 1). At MRI, two lesions presented hypointense signal on T1-weighted sequence and hyperintense on T2-weighted sequence, with hypointense thin septations inside on both sequences (fetuses 2 and 3), and one was heterogeneous, with a predominantly hyperintense signal on the T2-weighted sequence (fetus 1) (Figure 2).
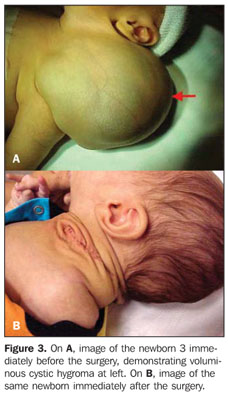
Additionally, MRI demonstrated involvement of the auricula in the case of fetus 2, and intrathoracic extension of the lesion towards the upper mediastinum in the case of fetus 1, which had not been demonstrated at US. By request of the assisting physician, the fetus 3 was submitted to a second MRI study after one week of life (Figure 2D). No other structure was involved by the lesion as compared with the prenatal MRI and obstetric US. In the three cases, airways involvement and associated chromosomal abnormalities were not observed, which has allowed a safe surgical planning and a good prognosis. All the three lesions were successfully resected without any impairment to the future life of the neonates (Figure 3).
DISCUSSION Fetal tumors, although uncommon, constitute unique circumstances in the management of pregnant patients, representing significant medical and ethical dilemmas(1). The knowledge on the specific types of tumors and respective biological characteristics is necessary for an appropriate counseling and management of these patients(1). Lymphangiomas are congenital malformations of the lymphatic system caused by a failure in the drainage from the primordial lymphatic sac(1,3). This failure leads to an enlargement of lymphatic channels, this theory being the one most commonly accepted, that of cystic hygroma. There are other theories regarding lymphangiomas, but the authors have opted for considering that of cystic hygromas, since this is the entity approached by the present study. There are four histological types of lymphangiomas: cystic hygroma, cavernous lymphangioma, capillary lymphangioma or lymphangioma simplex and vasculolymphatic malformation. All these types are formed by lymphatic channels with endothelial lining separated by a conjunctive tissue stroma(1). Frequently a combination of these four histological types may be found in a single lesion, and the difference among them is based merely on the size of lymphatic spaces and on their composition(1). Cystic hygroma is the most common type o lymphangioma and consists of huge cystic dilatations of the lymphatic space, occurring in the posterior cervical space in 70% of cases, 63% at left(1–3). Only 5% of these lesions are located below the diaphragm(3). No sex predominance is reported, usually occurring in children less than two years of age(2). These lesions present an infiltrative nature, usually invading adjacent structures (1,2), extending from the posterior cervical triangle to the mouth floor and tongue in the majority of cases, presenting extension towards the upper mediastinum in 10% of cases(1). In most of cases, the condition is asymptomatic and the size of the lesions is variable(2). Their growth is slow, but these lesions may present a rapid increase in size in cases of hemorrhage or trauma(2). Large masses may cause airways compression resulting in death(1). Small to middle-sized lesions may regress along the gestation(10). A correct prenatal diagnosis is extremely important, considering that, although cystic hygromas may be isolated malformations(1), these lesions are frequently associated with other chromosomal abnormalities, such as Turner syndrome and Down syndrome(1,2,10), that should be immediately investigated in case of suspicious diagnosis(8). In cases of isolated presentation, lymphangiomas have a good prognosis and most of times should be surgically resected. US is the method of choice for screening fetal malformations(11). Most of times, cystic hygroma presents like a predominantly cystic, multilocular mass with septa of variable thickness(2), and rarely with some solid component(1). The most echogenic portion of the lesion correlates with groups of small and abnormal lymphatic channels(2). In the three cases evaluated in the present series, the lesions were cystic hygromas, two of them predominantly cystic with thin septations inside, and one heterogeneous. All of the lesions were located in the posterior cervical region, two of them at left and one at right, with mean size of 7.0 × 2.3 × 5.2 cm (lateral × transverse × anteroposterior). MRI has been recognized as a useful complementary method, especially in cases where US results are dubious or undetermined(5,7,11,12). The advantages inherent to this imaging method include higher accuracy in the evaluation of soft tissues because of the better tissue contrast resolution besides the multiplanar capability(11), playing a significant role in the evaluation of lesions extent, most of times providing a more comprehensive and better fetal evaluation when performed in the sagittal plane(9). MRI is a safe method in fetal evaluation after the first gestational trimester(6,13) and provides additional information on lesions extent, demonstrating the presence or not of invasion of adjacent structures(13–15), and allowing a more appropriate, safe and individualized surgical planning. The most frequently observed pattern of cystic hygromas is that of a mass with iso- or hypointense signal on T1-weighted sequences, depending on the protein content of the lymphatic fluid, and hyperintense on T2-weighted sequences(1,2). Fluids with high protein content present hyperintense signal on T1-weighted sequences(1). Fluid level may be observed in cases of hemorrhage within the lesion(1–3) . In two cases of the present study, the lesions were hypointense on T1-weighted sequences, and hyperintense on T2-weighted sequences, with thin septations inside. In the third case, the lesion was heterogeneous with predominant hyperintense signal on T2-weighted sequences. The relation between cystic hygromas and soft tissues of the neck is most clearly demonstrated at MRI(2). This fact was confirmed by the present cases where MRI was more accurate than US in the evaluation of the lesions extent, demonstrating the invasion of adjacent structures, with extension towards the pinna of the fetus in one case, and towards the upper mediastinum in another one.
CONCLUSION In the present three-case series evaluating cervical lymphangiomas, the authors considered that MRI was complementary to US, with a similar role in the evaluation of the lesions site, size and content. However, MRI demonstrated to be superior in the correct and more accurate demonstration of lymphangiomas extent, allowing an appropriate and individualized surgical planning. After the analysis of the three cases of cystic hygromas by US and MRI, the authors have concluded that MRI plays a significant role as an ally of obstetric US in the evaluation of fetal lesions because of its higher accuracy in the determination of these tumors extent and adjacent structures invasion, allowing a better surgical planning and, therefore improving the quality of life of these patients.
REFERENCES 1. Woodward PJ, Sohaey R, Kennedy A, et al. A comprehensive review of fetal tumors with pathologic correlation. Radiographics. 2005;25:215–42. [ ] 2. Koeller KK, Alamo L, Adair CF, et al. Congenital cystic masses of the neck: radiologic-pathologic correlation. Radiographics. 1999;19:121–46. [ ] 3. Kaminopetros P, Jauniaux E, Kane P, et al. Prenatal diagnosis of an extensive fetal lymphangioma using ultrasonography, magnetic resonance imaging and cytology. Br J Radiol. 1997;70:750–3. [ ] 4. Levine D, Barnes PD, Edelman RR. Obstetric MR imaging. Radiology. 1999;211:609–17. [ ] 5. Coakley FV, Hricak H, Filly RA, et al. Complex fetal disorders: effect of MR imaging on management – preliminary clinical experience. Radiology. 1999;213:691–6. [ ] 6. Shinmoto H, Kashima K, Yuasa Y, et al. MR imaging of non-CNS fetal abnormalities: a pictorial essay. Radiographics. 2000;20:1227–43. [ ] 7. Weinreb JC, Lowe TW, Santos-Ramos R, et al. Magnetic resonance imaging in obstetric diagnosis. Radiology. 1985;154:157–61. [ ] 8. Hertzberg BS, Bowie JD, Carroll BS, et al. Normal sonographic appearance of the fetal neck late in the first trimester: the pseudomembrane. Radiology. 1989;171:427–9. [ ] 9. McCarthy SM, Filly RA, Stark DD, et al. Obstetrical magnetic resonance imaging: fetal anatomy. Radiology. 1985;154:427–32. [ ] 10. Sanders RC, Blakemore K. Lethal fetal anomalies: sonographic demonstration. Radiology. 1989;172:1–6. [ ] 11. Kubik-Huch RA, Huisman TAGM, Wisser J, et al. Ultrafast MR imaging of the fetus. AJR Am J Roentgenol. 2000;174:1599–606. [ ] 12. Tekşam M, Ozyer U, McKinney A, et al. MR imaging and ultrasound of fetal cervical cystic lymphangioma: utility in antepartum treatment planning. Diagn Interv Radiol. 2005;11:87–9. [ ] 13. Frates MC, Kumar AJ, Benson CB, et al. Fetal anomalies: comparison of MR imaging and US for diagnosis. Radiology. 2004;232:398–404. [ ] 14. Kathary N, Bulas DI, Newman KD, et al. MRI imaging of fetal neck masses with airway compromise: utility in delivery planning. Pediatr Radiol. 2001;31:727–31. [ ] 15. Ogura T, Hamada H, Obata-Yasuoka M, et al. Antepartum assessment of fetal cystic lymphangioma by magnetic resonance imaging. Gynecol Obstet Invest. 2002;53:237–9. [ ] Received November 3, 2008. Accepted after revision August 27, 2009. * Study developed at clinics Multi-Imagem and Clínica de Diagnóstico por Imagem (CDPI), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554