Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 5 - Sep. / Oct. of 2009
Vol. 42 nº 5 - Sep. / Oct. of 2009
|
ORIGINAL ARTICLE
|
|
Preterm labor diagnosis by sonographic measurement of the uterine cervical length |
|
|
Autho(rs): Carlos Eduardo Ferreira Novaes, Hilton Augusto Koch, Carlos Antônio Barbosa Montenegro, Jorge Fonte de Rezende Filho |
|
|
Keywords: Transvaginal ultrasonography, Preterm labor, Uterine cervical length, Preterm labor diagnosis |
|
|
Abstract:
IClinical Head of the 33ª Enfermaria (Maternidade) da Santa Casa da Misericórdia do Rio de Janeiro, Assistant Professor of Obstetrics, Universidade Gama Filho (UGF), Rio de Janeiro, RJ, Brazil
INTRODUCTION Preterm labor is the major cause of perinatal death, constituting a severe worldwide public health problem, inclusive in the United States where the incidence is around 10%(1). Additionally, preterm labor can be considered as a great social problem as this may represent the end of the dream of many families to have a healthy offspring. Also, one must consider the huge economic burden on the medical assistance, both at the public and private levels, as a result of frequently long, and consequently expensive hospitalization periods that may still end up in a great frustration with the death of the neonate. Additionally, it is important to note that in many cases, despite the high financial expenditure besides the personal and professional dedication, preterm labor may negatively affect the quality of life and psychosocial development of the children(2). Considering the magnitude of the theme, it is clear that it is necessary to minimize the negative consequences involved in preterm labor. Many conditions may lead to preterm labor, as follows: intrauterine infection, twin gestation, polyhydramnios, placental failure, uterine malformations, hemorrhagic syndromes, smoking, urinary infection, among others. However, despite the long range of causes, preventive measures against preterm labor have shown to be ineffective, since oral tocolysis has already proved to have no therapeutic value and, if effective, intravenous tocolysis only should be utilized with the objective of ensuring a correct and accurate administration of corticoids to accelerate the fetal lung maturation(3). Recent studies have been focused on determining the appropriate timing of corticoid administration, considering that the expected benefits to the fetus can be observed only 48 hours after administration, and that such benefits cease in seven days at maximum. It is known that no effect is observed with later and/or repeated administration of corticoid to the pregnant mother, as previously thought. This argument corroborates the power of corticoid administration, but can be utilized only one time(1). So, it is urgent to determine the predictive factor of preterm labor. Some studies try to find the correct value for uterine cervix length for predicting this accident. However, a consensus about this matter is still to be achieved in the worldwide medical literature(3–6) that, on the contrary, demonstrates disagreement between values reported be several studies. The most relevant among these studies is the one developed by Kagan et al.(7), who have demonstrated the high incidence of preterm birth in patients whose sonographic findings had demonstrated significant shortening of the uterine cervix. Additionally, Kagan et al. demonstrate that, in patients with a single gestation, with symptoms corresponding to preterm labor threat and uterine cervical length < 15 mm, the labor occurs within a seven-day period; and that, in patients with uterine cervical length > 15 mm, the delivery occurs after this period. These data represent an attempt to predict the ideal moment to accelerate the fetal lung maturation(1,2) and the correct introduction of intravenous tocolysis for this purpose. The present study evaluates a substantial series of preterm labor threats with the objective of collaborating in the development of a nationwide casuistics as a contribution to determine an effective predictive factor of preterm labor in the Brazilian population, utilizing an easy-to-perform, low-cost imaging method that is widely adopted in the daily obstetric practice: transvaginal ultrasonography(8–12).
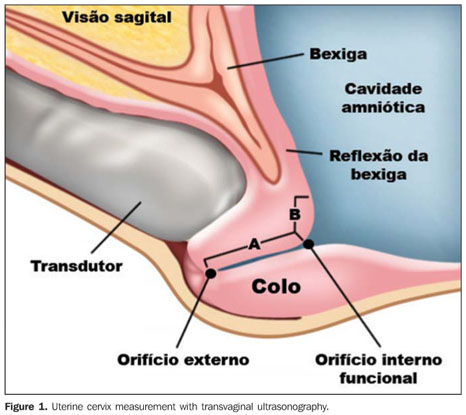
MATERIALS AND METHODS Upon approval by the Committee for Ethics in Research, a longitudinal, prospective study evaluated, by means of transvaginal ultrasonography, the uterine cervical length in all the patients with clinical signs of preterm labor threat assisted in the authors' institution from October/2008 to February/2009. Uterine cervical length was evaluated in 72 patients with preterm labor threat with the objective of establishing a direct correlation between the measurements and the occurrence of labors within a seven-day period. Preterm labor threat was characterized in cases where clinical signs presented between the 22nd and 37th gestational weeks, with poor visualization of 80% or more of the uterine cervix at ultrasonography, besides a minimum 2 cm-dilatation and presence of uterine contractions twice every ten minutes, with a minimum duration of 40 seconds(1). Exclusion criteria were the following: patients with therapeutic preterm labor induction, dead fetus, premature amniorrhexis, chorioamnionitis, uterine malformations, cervical diseases, fetal malformations, twin gestation, previous history of preterm labor and hemorrhagic syndromes(6–8). A term of free and informed consent was signed by the patients who underwent transvaginal ultrasonography with empty bladder (after spontaneous micturition immediately before the examination) with a Hitachi EUB 525 (Hitachi; Tokyo, Japan) unit with a 6.0 MHz transducer. After introduction of the transducer through the vaginal tract and identification of the external and internal orifices without compression on the cervix, the endocervical canal was defined as a hyperechogenic line between these orifices(6). The measurement of the uterine cervical length was performed on a sagittal view, on the monitor screen, at mean 50% magnification, by drawing a straight line between the external and internal orifices(6,13–15) (Figures 1 and 2). On average, the examination time was of seven minutes. Three measurements were performed, and the lowest among the three values was selected(4,5). All the examinations were performed by a single sonographist with ten-year practical experience. The data were recorded on an appropriate individual dossier and later submitted to statistical analysis for obtention of negative and predictive values, besides the determination of specificity and sensitivity of the method. The ROC curve was not utilized for certifying a new minimum uterine cervical length related to spontaneous birth within seven days, since the authors' proposal was to compare the values found by the present study with the cutoff value reported by Kagan et al.(7) for preterm labors. The authors of the present study are currently developing a more extensive casuistics whose data will be submitted to the ROC curve for determining their own cutoff value. A schematic representation of the study is shown on Figure 3.
RESULTS Seventy-two patients were included in the study protocol (Table 1). Their age range was between 14 and 41 years (mean, 27.5 years). The ethnic composition of the sample was the following: 70% of the patients were white, 25% black, and 5% of other races. As regards parity, 47.2% of the patients were primiparae, 25%, secundiparae, and 25.7% had had more than two gestations. The mean gestational age at the onset of clinical signs of preterm labor threat and at the time of the examinations was 28.9 weeks. The greatest uterine cervical length observed was 45 mm, and the smallest was 0.8 mm.
In the present study, 20 patients (27.7%) presented a cervix with < 15 mm in length, and 52 (72.2%) > 15 mm. Among the 20 patients with cervix < 15 mm, 19 (95%) progressed to labor in up to seven days. Most of the patients (98.7%) in the group with cervix > 15 mm progressed to labor after the seven-day period. Only three patients (4.1%) had not the expected behavior: in two cases (2.7%) with uterine cervical length > 15 mm (40 and 27 mm) the labors occurred within the seven-day period, and in the other case, where the uterine cervical length was < 15 mm (13 mm), the labor did not occur within the sevenday period, but still it was a preterm labor (35 weeks). Statistical validity analysis of the method demonstrated 90.5% sensitivity and 98% specificity. Positive predictive value was 95% and negative predictive value was 96%. The measurement of uterine cervical length by transvaginal ultrasonography was uneventful in all of the patients included in the present study. The examination was extremely well tolerated by all the pregnant women, even in the setting of clinical signs compatible with a threat of preterm labor. The therapeutics was not impaired, since all the patients were followed-up on an inpatient basis and submitted to treatment with uterolytic agents and corticoid to accelerate the fetal lung maturation, as routinely done nowadays in the majority of obstetric centers.
DISCUSSION The most extensive investigation on the present theme has been developed by Tsoi et al.(16), who have utilized ultrasonography to measure the uterine cervical length in 510 women with preterm labor threat. Labor occurred within 48 hours in 4.15% of cases, and before the 35th week in 14.9%. The logistic regression analysis has demonstrated the uterine cervical length as a sole independent predictive factor for labor within 48 hours. For labor within seven days, the independent predictive factors were uterine cervical length and vaginal bleeding. In the group of women whose labor did not occur within seven days, the incidence of labor before the 35th week was of 7.1%. The authors have concluded that in women with preterm labor threat, the sonographic measurement of the uterine cervical length allowed the differentiation between true and false labor. Additionally, Tsoi et al. have reported that in three studies about this same theme, involving 532 women with 24-36 gestational weeks and preterm labor threat, the labor have occurred within seven days in 49% of cases with uterine cervical length < 15 mm, and in only 1.2% of cases with uterine cervical length > 15 mm(16). The careful observation of the present casuistics clearly demonstrates that, in the case where the labor did not occur within seven days, even with uterine cervical length < 15 mm, it occurred in the preterm period corresponding to 35 gestational weeks. The case where the uterine cervical length was > 15 mm and the labor occurred within the sevenday period corroborates the argument that upon continuation and worsening of symptoms the examination should be repeated on a daily basis for assessing the shortening of the uterine cervix and ensuring a correct administration of corticoids. The measurement of uterine cervical length by transvaginal ultrasonography was uneventful in all of the patients included in the present study. The examination was extremely well tolerated by all the pregnant women even in the setting of clinical signs compatible with preterm labor threat. The therapeutics was not impaired, since all the patients were followed-up on an inpatient basis and submitted to treatment with uterolytic agents and corticoids to accelerate the fetal lung maturation as routinely done nowadays in the majority of obstetric centers.
CONCLUSION The present study demonstrates that in most of cases preterm labor can be predicted, allowing a more appropriate indication of fetal lung maturation.
REFERENCES 1. Montenegro CAB, Rezende Filho J. Rezende – Obstetrícia fundamental. 11ª ed. Rio de Janeiro: Guanabara Koogan; 2008. [ ] 2. Leveno KJ, Cunningham FG, Gant NF, et al. Manual de obstetrícia de Williams. 21ª ed. Porto Alegre: Artmed; 2005. [ ] 3. Gibson JL, Macara LM, Owen P, et al. Prediction of preterm delivery in twin pregnancy: a prospective, observational study of cervical length and fetal fibronectin testing. Ultrasound Obstet Gynecol. 2004;23:561–6. [ ] 4. Oliveira TA, Carvalho CMP, Souza E, et al. Avaliação do risco de parto prematuro: teste da fibronectina fetal e medida do colo uterino. Rev Bras Ginecol Obstet. 2000;22:633–9. [ ] 5. Yamasaki AA, Bittar RE, Fonseca ESB, et al. Prevenção do parto prematuro: emprego do toque vaginal e da ultra-sonografia transvaginal. Rev Bras Ginecol Obstet. 1998;20:350–6. [ ] 6. Brandão RS, Pires CR, Souza E, et al. Avaliação biométrica do colo uterino durante a gestação por meio da ultra-sonografia transvaginal e ressonância magnética. Radiol Bras. 2008;41:235–9. [ ] 7. Kagan KO, To M, Tsoi E, et al. Preterm birth: the value of sonographic measurement of cervical length. BJOG. 2006;113 Suppl 3:52–6. [ ] 8. Guzman ER, Ananth CV. Cervical length and spontaneous prematurity: laying the foundation for future interventional randomized trials for the short cervix. Ultrasound Obstet Gynecol. 2001;18:195–9. [ ] 9. Brandão RS, Murta CGV, Moron AF, et al. Ultra-sonografia tridimensional do colo uterino na gestação: perspectivas. Radiol Bras. 2006;39:305–8. [ ] 10. Carbonne B. Is it possible to improve diagnostic and prognostic criteria of preterm labour? Eur J Obstet Gynecol Reprod Biol. 2004:15:117 Suppl 1:S6–9. [ ] 11. Fuchs I, Tsoi E, Henrich W, et al. Sonographic measurement of cervical length in twin pregnancies in threatened preterm labor. Ultrasound Obstet Gynecol. 2004;23:42–5. [ ] 12. Berghella V, Berghella M. Cervical length assessment by ultrasound. Acta Obstet Gynecol Scand. 2005;84:543–4. [ ] 13. Pires CR, Moron AF, Mattar R, et al. Estudo comparativo entre marcadores ultra-sonográficos morfológicos preditores de parto pré-termo: sinal do afunilamento do colo e ausência do eco glandular endocervical. Radiol Bras. 2005;38:17–24. [ ] 14. Carr BD, Smith K, Parsons L, et al. Ultrasonography for cervical length measurement: agreement between transvaginal and translabial techniques. Obstet Gynecol. 2000;96:554–8. [ ] 15. Ferreira AC, Mauad Filho F, Nicolau LG, et al. Ultra-sonografia tridimensional em ginecologia: malformações uterinas. Radiol Bras. 2007;40:131–6. [ ] 16. Tsoi E, Fuchs IB, Rane S, et al. Sonographic measurement of cervical length in threatened preterm labor in singleton pregnancies with intact membranes. Ultrasound Obstet Gynecol. 2005;25:353–6. [ ] Received April 1st, 2009. Accepted after revision June 29, 2009. * Study developed at Santa Casa da Misericórdia do Rio de Janeiro – 33ª Enfermaria (Maternidade), Rio de Janeiro, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554