IMaster in Radiology, MD, Radiologist at Medimagem, Niterói, RJ, and Labs D'Or Laboratório e Imagem, Rio de Janeiro, RJ, Brazil
IIPhD, Associate Professor, Department of Radiology - Universidade Estadual do Rio de Janeiro (UERJ), Niterói, RJ, MD, Radiologist, Instituto Nacional de Câncer (INCA), Rio de Janeiro, RJ, Brazil
Mailing address
INTRODUCTION
Sinusopathy is a common clinical problem that, sometimes, does not present an adequate response to medicamentous therapy. Computed tomography (CT) is the method of choice for evaluating these cases, particularly in the setting of a probable surgical intervention(1). Endoscopic surgery has been increasingly utilized, requiring a meticulous assessment and a detailed description of both nasal and paranasal cavities structures(2). Considering that the main objective of this type of surgery is to reopen the natural ways of drainage of paranasal cavities, it is very important that the radiologist is aware of the ostiomeatal complex variants, describing them in a comprehensible way for the otorhinolaryngologist(3-8).
The present study was aimed at evaluating the frequency and types of anatomical variants of the ostiomeatal complex.
MATERIALS AND METHODS
CT studies of 200 patients evaluated for clinical suspicion of sinusopathy were analyzed. The sample included 111 women and 89 men in the age range between eight and 87 years (mean age = 39 years) and with no previous history of surgery. Images were acquired in three different types of tomographs: Twin Elscint (Marconi; Haifa, Israel), Light Speed (GE Healthcare; Wisconsin, USA) and Somatom AR-Star (Siemens; Erlangen, Germany).
The protocol consisted of coronal and axial slices, respectively, perpendicular and parallel to the palate, with 2-3 mm in thickness. For patients who could not tolerate the prone position (hyperextended neck) required for coronal images acquisition, helical acquisition was performed with 2-3 mm collimation and computer-generated reconstructed coronal views.
In all of the cases, bone algorithm was utilized for documentation, and soft tissues window was utilized in some selected cases.
RESULTS
One or more anatomical variants (Graphic 1) were identified in 167 of the 200 cases evaluated (83.5%). The majority of patients presented with up to two anatomical variants (38% with one; 27% with two variants).
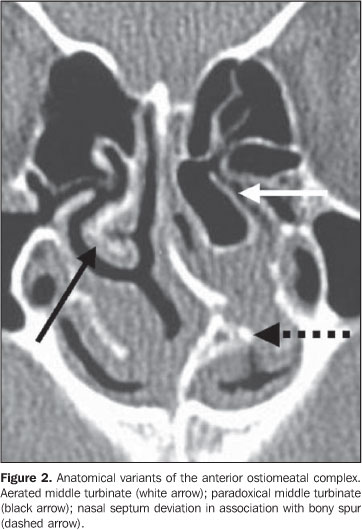
The frequency of anatomical variants of the ostiomeatal complex is shown on Graphic 2. Most of these anatomical variants involved the middle turbinate (84%) and the nasal septum (34%) (Figure 2), including: unilateral middle turbinate pneumatization in 39 cases (23%), bilateral pneumatization in 19 cases (11%), unilateral paradoxical middle turbinate curvature in 34 cases (20%) and bilateral paradoxical middle turbinate curvature in 24 cases (14%).
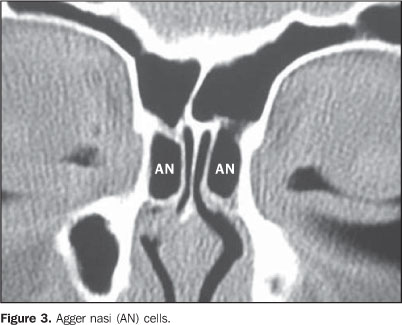
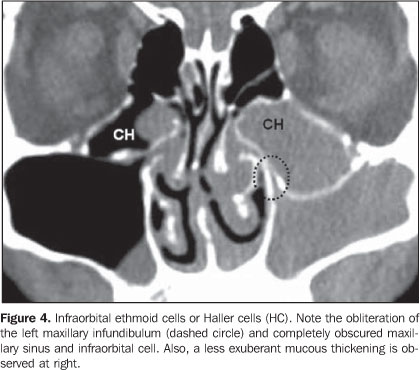
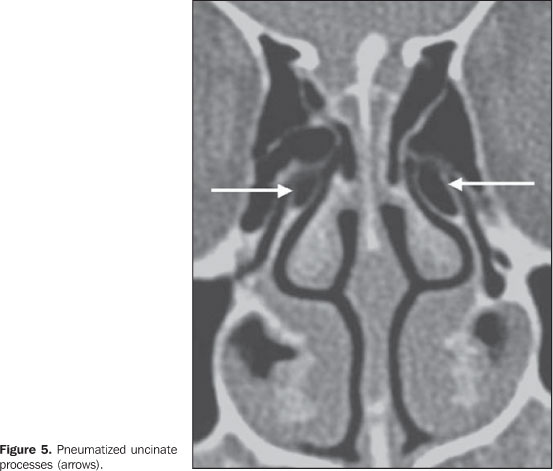
Other pneumatized structures were: agger nasi cells (Figure 3) in 27 cases (16%), unilateral or bilateral pneumatization of the uncinate process in 26 cases (16%) (Figure 5), and infraorbital (Haller) cells in 16 cases (10%) (Figure 4).
Among the variants of the uncinate process insertion which were found in 10 cases, seven (3.5%) presented the uncinate process inserted into the middle turbinate, two (1%) into the ethmoid cribriform plate, and one (0.5%) into the middle orbital wall.
Other less frequent variants found were: aberrant ethmoidal bulla in eight cases (5%), hypoplastic middle turbinate in 14 cases (8%), paradoxical inferior turbinate, medial deviation of the uncinate process, hypoplastic maxillary sinus, and nasal septum spur without associated deviation in two cases each (1%), and only one case (0.6%) with each of the following variants: bilateral paradoxical inferior turbinate, spiral-shaped middle turbinate, pneumatized superior turbinate, hypoplastic middle turbinate attached to the uncinate process, enlarged inferior turbinate, double maxillary infundibulum, choanal atresia, uncinate process attached to the infraorbital ethmoid cell, accessory middle turbinate and duplicate middle turbinate.
DISCUSSION
The ostiomeatal complex is differently defined by several authors.
Scribano et al.(9) have defined the ostiomeatal complex as a complex including the maxillary sinus ostium, ethmoid infundibulum and middle meatus; in other words, as the final site of drainage from the frontal and maxillary sinuses and anterior ethmoidal cells.
Casiano(10) has defined the ostiomeatal complex as the ethmoid bulla, uncinate process and adjacent spaces and ostia draining the anterior sinuses (anterior ethmoid sinus, frontal and maxillary sinuses).
Zinreich et al.(11) have defined the ostiomeatal complex as the group of bony structures and aerated channels into which the paranasal cavities drain, and have subdivided the complex into three parts. The first most anterior portion of the complex includes structures surrounding the frontal recess; the second one corresponds to the structures including the maxillary sinus and middle meatus; and the third and most posterior portion includes the structures surrounding the sphenoethmoidal recess. The ostiomeatal complex would be formed by the two first portions(11). Mafee et al.(12) and Mafee(13) have described the ostiomeatal complex similarly to the definition by Zinreich et al.(11).
Laine & Smoker(14) have defined the ostiomeatal complex as an aerated channel of the middle meatus representing the final common pathway for drainage of the maxillary and frontal sinuses and anterior ethmoid cells, delimited by the uncinate process, ethmoidal bulla and middle turbinate.
Shankar et al.(6) have defined ostiomeatal complex as a complex including the maxillary ostium, ethmoid infundibulum, hiatus semilunaris, middle meatus, frontal recess, ethmoid bulla and uncinate process.
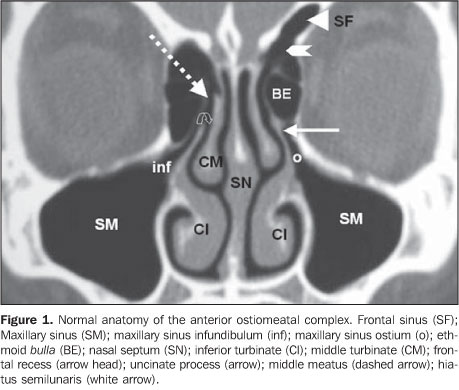
In the present study, the concept developed by Stammberger & Kennedy(7) was adopted, defining ostiomeatal complex as a functional unit of the anterior ethmoid complex representing the final common pathway for drainage and ventilation of the frontal, maxillary and anterior ethmoid cells. Any of these cells, clefts, ostia, recesses or cavities may be affected by a pathological process, thereby contributing to the symptoms and pathophysiology of sinusitis (Figure 1).
Anatomical variants of the ostiomeatal complex were found in 83.5% of cases in the present casuistic, a rate within the frequency interval observed by other authors — Bolger et al.(3) have reported a frequency of 64.9%; Pérez-Piñas et al.(5), 67%; Tonai & Baba(15), 75%; and Earwaker(16), 93%.
The groups evaluated, as well as pediatric groups, ranged considerably in size and distribution (Graphic 1)(4). Kinsui et al. have compared symptomatic and asymptomatic groups(17), and other authors have evaluated patients with suspected or confirmed sinusopathy(5,9,15,16,18,19). Earwaker(16) has studied 800 individuals, and the majority of authors have studied groups ranging from 71 to 200 patients(3-5,7,15,19-21), similarly to the number of patients included in the present study (200 patients).
The authors have reported quite different frequencies of anatomical variants (Graphic 1). Maybe, these divergences could be explained either by populational differences, by the definition adopted for anatomical variants (Graphic 1), or by the methodology of analysis(3).
Nasal septum
Deviation of the nasal septum can be defined as any midline deviation(16,20) and may be cartilaginous, osteocartilaginous or osseous. Severe nasal septal deviation may result in compression of the inferior or middle turbinate, causing obstruction of the normal mucus flow and, consequently, secondary inflammation and infection(14,20).
Deviation of the nasal septum was found in 28.5% of cases in the present study (Figure 2). In other studies, this finding ranged from 14.1% to 80%: Dutra & Marchiori(4), 14.1%; Kinsui et al.(17), 23.3%; Arslan et al.(18), 36%; Earwaker(16), 44%; and Pérez-Piñas et al.(5), 80%.
Middle turbinate or middle concha
Concha bullosa is one of the most frequently found anatomical variants(22,23). The differences reported in the prevalence of middle turbinate pneumatization may have been influenced by the aeration degree, and lower rates suggest that only large turbinates may have been taken into consideration. This finding may have been influenced by the sensitivity of the analysis method. There may be inherent differences among macroscopic anatomical study, analysis of conventional radiographs, tomographic studies and techniques of microscopic dissection(3). For Pérez-Piñas et al.(5), the middle turbinate was aerated only in cases where both the vertical cribriform plate and inferior bulbar portion were pneumatized. The present study has adopted the definition by Zinreich et al.(23), who have considered any pneumatization degree as concha bullosa.
Middle turbinate aeration was found in 42.5% of patients in the present study (Figure 2). Other studies have found prevalence of 21%(19), 28%(15,20), 30%(18), 33%(17) and 35%(16), all of them ranging between 21% and 73%(5), excepting Dutra and Marchiori(4) whose study has included only pediatric patients (4%).
Typically, the curved portion of the middle turbinate points toward the nasal septum. In cases where the curvature unusually occurs toward the opposite side, they are called paradoxical turbinates(14,20). This variation can be observed either in superior, middle or inferior turbinates, although this is much more frequent in middle turbinates. Again, the prevalence reported by different authors may diverge because some of them, like the authors of the present study, consider any involved portion of the turbinate as paradoxical curvature, whereas others may consider this variation only in cases where the whole turbinate is unusually curved towards the opposite side.
In the present study, 58 patients were found with paradoxical middle turbinates (29%). Arslan et al.(18) have found this variant in 3% of cases, Bolger et al.(3) in 26,1%, Earwaker(16) in 43%, Pérez-Piñas et al.(5) in 73% and Tonai & Baba(15) in 28%.
Agger nasi
The agger nasi is the most superior remnant of the first ethmoturbinate, which persists as a mound or tuberosity immediately anterior and superior to the insertion of the middle turbinate(7,12). An agger nasi cell results when this area becomes pneumatized. Agger nasi cells present a close relationship with five different cranial bones: lacrimal bone, maxillary bone, ethmoid bone, frontal bone and nasal bone(3). Very small agger nasi cells may be missed during anatomical dissections but not at CT.
Zinreich et al.(23), based on their experience with CT of paranasal sinuses, nasal endoscopy and functional endoscopic surgery, have demonstrated that agger nasi cells are air cells under the frontal sinus extending anterosuperiorly toward the frontal recess, reaching the lacrimal fossa inferolaterally, and laterally adjacent to the nasal bones. Frequently, agger nasi is the antero-inferior border of the frontal recess(3,24), and agger nasi aeration may be implied in cases of chronic frontal sinusitis. In the present study, the Zinreich et al.(23) agger nasi concept was adopted.
Agger nasi cells were found in 13.5% of patients in the present casuistic (Figure 3), but other authors have reported prevalence rates of 7%(20), 86%(15), 96%(16) and 98%(3).
Infraorbital ethmoid cells or Haller cells
Arslan et al.(18) and Meloni et al.(19) have defined infraorbital ethmoid cell or Haller cell as a pneumatized ethmoid cell between the orbit and the maxillary sinus. Zinreich et al.(8,23) have described infraorbital ethmoid cell or Haller cell as an ethmoid cell that is found below the ethmoid bulla, attached to the floor of the maxillary sinus, adjacent to the maxillary infundibulum, as part of the lateral wall of the infundibulum. Stammberger & Kennedy(7) and Bolger et al.(3) have added that these cells are found precisely in the region of the maxillary sinus ostia. It is postulated that infraorbital ethmoid cells might constitute an etiological factor in the recurrent maxillary sinusitis(8), but, according to Bolger et al.(3) they should be analyzed on a case-by-case basis, considering that other authors have not observed statistically significant differences between patients with and without inflammatory sinus disease. In the present study, the definition coined by Stammberger & Kennedy(7) and Bolger et al.(3) was adopted.
In the present study, infraorbital ethmoid cells were found in 8% of cases (Figure 4), but other authors have reported a wide variation in the prevalence rates such as 1%(4), 5.5%(20), 6%(18), 9%(17), 20%(5), 36%(15) and 45%(3).
The uncinate process
The most common anatomical variants of the uncinate process are represented by insertion into an unusual topography and pneumatization.
The uncinate process is a superior extension from the lateral wall of the nasal cavity and generally is inserted into the postero-medial portion of the agger nasi(11,16).
Uncinate process insertion into other structures may result in a blind-end obstruction. In cases where the uncinate process inserts onto the lamina papyracea, the maxillary sinus drainage may be impaired(16,25). In the present study, this anatomical variation was found in one case (0.5%). If the uncinate process attaches to the middle turbinate or cribriform plate, the frontal and homolateral maxillary sinuses drainage may be impaired, resulting in a mechanism of sinus mucus recirculation. In the present study, these variants were found, respectively, in seven cases (3.5%) and in two cases (1%). Earwaker(16), in a study of 800 cases, have described variants of the uncinate process in detail, classifying them in association with other variants of the ostiomeatal complex and subdividing them differently from the present study. Other authors included in Table 1 have not approached anatomical variants of the uncinate process.
Pneumatized uncinate process (or uncinate bulla) also has been associated with poor sinus ventilation(11,14), specifically of the anterior ethmoid, frontal recess and of the infundibulum region. A careful analysis of consecutive CT images suggest that the pneumatization of the uncinate process occurs because of agger nasi excavation in the most anterosuperior region of the uncinate process(3).
In the present study, pneumatization of the uncinate process was found in 13% of cases (Figure 5), whereas other authors report prevalence rates of 2.5%(3), 4%(18) and 9.1%(16).
CONCLUSION
Different and frequent anatomical variants may be found in the anterior ostiomeatal complex, and a single individual may present with different variants. In the present study, the most frequent variants were those involving the middle turbinates, particularly their pneumatization and paradoxical curvature, deviation of the nasal septum and pneumatized agger nasi cells, infraorbital ethmoid cells and uncinate process.
REFERENCES
1. Melhem ER, Oliverio PJ, Benson ML, et al. Optimal CT evaluation for functional endoscopic sinus surgery. AJNR Am J Neuroradiol. 1996;17: 181-8. [ ]
2. Ludwick JJ, Taber KH, Manolidis S, et al. A computed tomographic guide to endoscopic sinus surgery: axial and coronal views. J Comput Assist Tomogr. 2002;26:317-22. [ ]
3. Bolger WE, Butzin CA, Parsons DS. Paranasal sinus bony anatomic variations and mucosal abnormalities: CT analysis for endoscopic sinus surgery. Laryngoscope. 1991;101(1 Pt 1):56-64 . [ ]
4. Dutra LD, Marchiori E. Tomografia computadorizada helicoidal dos seios paranasais na criança: avaliação das sinusopatias inflamatórias. Radiol Bras. 2002;35:161-9. [ ]
5.P érez-Piñas, Sabaté J, Carmona A, et al. Anatomical variations in the human paranasal sinus region studied by CT. J Anat. 2000;197:221-7. [ ]
6. Shankar L, Evans K, Hawke M, et al. An atlas of imaging of the paranasal sinuses. London: Martin Dunitz; 1994. [ ]
7. Stammberger HR, Kennedy DW. Paranasal sinuses: anatomic terminology and nomenclature. The Anatomic Terminology Group. Ann Otol Rhinol Laryngol Suppl. 1995;167:7-16. [ ]
8. Zinreich SJ, Kennedy DW, Rosenbaum AE, et al. Paranasal sinuses: CT imaging requirements for endoscopic surgery. Radiology. 1987;163:769-75. [ ]
9. Scribano E, Ascenti G, Loria G, et al. The role of the ostiomeatal unit anatomic variations in inflammatory disease of the maxillary sinuses. Eur J Radiol. 1997;24:172-4. [ ]
10. Casiano RR. Correlation of clinical examination with computer tomography in paranasal sinus disease. Am J Rhinol. 1997;11:193-6. [ ]
11. Zinreich SJ, Albayram S, Benson M, et al. The ostiomeatal complex and functional endoscopic surgery. In: Som PM, Curtin HD, editors. Head and neck imaging. 4th ed. St. Louis: Mosby; 2003. p. 149-74. [ ]
12. Mafee MF, Chow JM, Meyers R. Functional endoscopic sinus surgery: anatomy, CT screening, indications, and complications. AJR Am J Roentgenol. 1993;160:735-44. [ ]
13. Mafee MF. Preoperative imaging anatomy of nasal-ethmoid complex for functional endoscopic sinus surgery. Radiol Clin North Am. 1993;31:1-20. [ ]
14. Laine FJ, Smoker WR. The ostiomeatal unit and endoscopic surgery: anatomy, variations and imaging findings in inflammatory diseases. AJR Am J Roentgenol. 1992;159:849-57. [ ]
15. Tonai A, Baba S. Anatomic variations of the bone in sinonasal CT. Acta Otolaryngol Suppl. 1996; 525:9-13. [ ]
16. Earwaker J. Anatomic variants in sinonasal CT. Radiographics. 1993;13:381-415. [ ]
17. Kinsui MM, Guilherme A, Yamashita HK. Variações anatômicas e sinusopatias: estudo por tomografia computadorizada. Rev Bras Otorrinolaringol. 2002;68:645-52. [ ]
18. Arslan H, Aydinlioglu A, Bozkurt M, et al. Anatomic variations of the paranasal sinuses: CT examination for endoscopic sinus surgery. Auris Nasus Larynx. 1999;26:39-48. [ ]
19. Meloni F, Mini R, Rovasio S, et al. Anatomic variations of surgical importance in ethmoid labyrinth and sphenoid sinus. A study of radiological anatomy. Surg Radiol Anat. 1992;14:65-70. [ ]
20.Kayalioglu G, Oyar O, Govsa F. Nasal cavity and paranasal sinus bony variations: a computed tomographic study. Rhinology. 2000;38:108-13. [ ]
21. Ünlü HH, Akyar S, Caylan R, et al. Concha bullosa. J Otolaryngol. 1994;23:23-7. [ ]
22. Zinreich SJ, Mattox DE, Kennedy DW, et al. Concha bullosa: CT evaluation. J Comput Assist Tomogr. 1988;12:778-84. [ ]
23. Zinreich SJ, Kennedy DW, Gayler BW. Computed tomography of nasal cavity and paranasal sinuses: an evaluation of anatomy for endoscopic sinus surgery. Clear Images. 1988;1:2-10. [ ]
24. Daniels DL, Mafee MF, Smith MM, et al. The frontal sinus drainage pathway and related structures. AJNR Am J Neuroradiol. 2003;24:1618-27. [ ]
25. McLaughlin RB Jr, Rehl RM, Lanza DC. Clinically relevant frontal sinus anatomy and physiology. Otolaryngol Clin North Am. 2001;(34):1-22. [ ]
 Mailing address:
Mailing address:
Dra. Anna Patricia Riello
Avenida Visconde de Albuquerque, 1102/201
Leblon. Rio de Janeiro, RJ
Brazil, 22450-000
E-mail: anna.riello@gmail.com
Received July 13, 2006. Accepted after revision September 14, 2007
* Study developed at Labs D'Or Laboratório e Imagem, Rio de Janeiro, RJ, and Medimagem, Niterói, RJ, Brazil.
