INTRODUCTION
The core function of the uterine cervix in pregnancy and in normal delivery is well established. The cervix functions as a valve responsible for ensuring the retention of the fetus in uterus up to the end of the pregnancy. At delivery, it undergoes changes allowing the safe transit of the conceptus(1). Preterm delivery, defined as a delivery occurring before the 37th gestational week is the most relevant problem associated with neonatal mortality and morbidity in the developed world(2). A logical strategy to prevent preterm delivery starts with the identification of patients at risk. As the cervical length shortening is a normal component of human parturition, many investigators have assessed the value of ultrasonography in the measurement of cervical length during pregnancy, and it has been reported that this is one of the parameters with closest correlation with the risk for preterm delivery(3). Although a consensus on the normal cervical length over the different gestational weeks is still to be reached, there is ample evidence that a short cervical length is associated with a higher prevalence of preterm delivery(4). The representative risk threshold is also controversial, with several studies suggesting measurements between 15 and 35 mm. Such lack of consensus has been attributed to differences among studied populations: low or high risk for preterm delivery, gestational age at the moment of the studies, investigation design (longitudinal or cross sectional) and patients’ parity(5–9).
The reasons for pursuing the development of a chart on cervical lengths are the existence of different reports in the literature on changes of the uterine cervix along the gestational period and the fact that the uterine cervix length may differ in different populations. In the clinical practice, the early detection of abnormalities in the cervical length is important, thus the need to accurately define the normal cervical length for each gestational week. The present study is aimed at evaluating the uterine cervix length in a population of healthy pregnant women, between the 20th and 34th weeks of gestation, with the purpose of constructing a normality curve for this gestational period.
MATERIALS AND METHODS
A cross sectional study including 145 healthy pregnant women under prenatal follow-up, between the 20th and 34th gestational weeks.
The gestational age was determined by means of the last menstruation date and ultrasonography performed before the 20th week. Differences of up to 8% between biometric parameters and the last menstruation date, confirmed the last menstruation date as the parameter to estimate gestational age. Otherwise biometric parameters were utilized. In order to establish normal values, the authors waited for the pregnancies outcome, and only the women who had term delivery (> 37 weeks) were included in the final analysis.
The sample included both primigravidae and women with a previous history of pregnancy. The patients were initially submitted to anamnesis for evaluation of inclusion and exclusion criteria. Inclusion criteria were the following: pregnancy with a single live fetus, gestational age between the 20th and 34th weeks, and absence of maternal or fetal diseases. Exclusion criteria were the following: previous surgical interventions (cervical conization) in the uterine cervix, cerclage, fetal malformations, low-lying placenta, amniorrhexis changes in the amniotic fluid index, and fetal death. Additionally, the presence of labor, vaginal bleeding, or symptoms of vulvovaginitis at the time of the examination were also considered as exclusion criteria. Rest, tocolysis and steroids were utilized as clinically appropriate, but, because of the medicamentous intervention, the patients were excluded from the study. Patients presenting early delivery and those from whom delivery data could not be obtained were also excluded. Patients who met inclusion criteria, regardless of age, received explanations on the study and were invited to participate in the study. Those who agreed in participating in the present study signed a term of free and informed consent. In case of patients under legal age, consent was also requested from parents or caregivers.
The measurements of uterine cervix length were standardized and performed by a single observer trained and qualified in compliance with the principles established by Fundação de Medicina Fetal – FMF Brazil (Fetal Medicine Foundation), according to the Certificate of Competency in Cervical Assessment, by means of transvaginal ultrasonography with a 4.0 to 9.0 MHz transducer connected to a Voluson 730 Expert unit (GE Healthcare; Buckinghamshire, England) or Sonoace 9900 unit (Medison; Gyeonggi-do, South Korea). After emptying the bladder, the patients were placed in lithotomy position and the probe was gently placed into the anterior vaginal fornix in order to acquire a full sagittal view of the cervix, including the external and internal orifices, and the cervical canal, while avoiding exerting inappropriate pressure on the cervix, which could erroneously elongate it. The probe was then slowly moved backward until the image became blurred, and then enough pressure to restore a clear image was applied. The image was then magnified so that a clear visualization of the cervix and internal and external orifices was obtained. The distance between the internal and external orifices along the endocervical canal was then measured in millimeters. Care was taken so that, on the sagittal view, the distances from the surface of anterior and posterior labia to the cervical canal were the same. The sonolucent cervical mucosa was used as a guide for the true position of the internal orifice, thus avoiding confusion with the lower uterine segment (Figure 1). Funneling was considered as being present whenever the internal orifice was U- or V-shaped with > 5 mm in width.
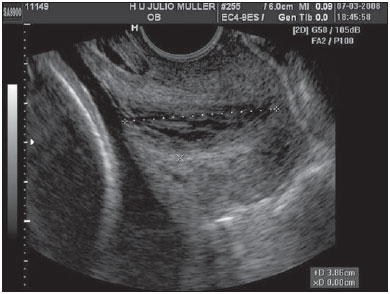
Figure 1. Measurement of uterine cervix.
Data on the pregnancies outcome were later obtained from the assisting physicians or from the patients themselves, by phone. The results are presented on a chart and table. Variables with normal distribution were expressed as mean and standard deviation. The Student’s t test was utilized for means comparison. The possible association between body mass index (BMI) and cervical length was evaluated by analysis of variance. The association between uterine cervical length and gestational age was assessed by means of linear regression. The significance of r was analyzed by means of the Student’s t test. The 5th, 50th and 95th percentiles for each gestational age were calculated and demonstrated on a chart (Figure 2). Results with alpha error up to 5% were considered as being statistically significant.
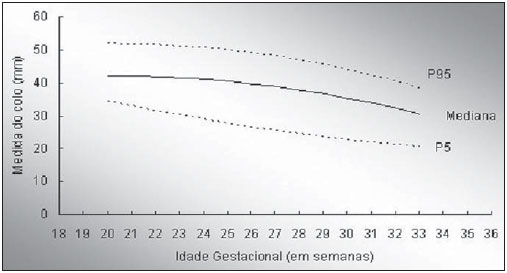
Figure 2. Median representation, 5th and 95th percentiles of uterine cervix length as a function of gestational age. Cervical measurements (50th percentile) = 13.42 – 0.07 Χ GA Χ GA + 2.83 Χ GA. Cervical measurement (5th percentile) = 81.55 + 0.04 Χ GA Χ GA – 3.16 Χ GA. Cervical measurement (95th percentile) = 19.30 – 0.08 Χ GA Χ GA + 3.22 Χ GA.
Measurements of uterine cervix length were performed in 200 pregnant women. After exclusion of those cases with unknown outcomes, preterm delivery or medicamentous intervention to prevent it (use of progesterone or tocolytics), 145 patients remained in the study. Of those 145 patients, 84 (57.9%) came from a private clinic (Fetalcare) and 61 (42.1%) came from the public health system (Hospital Universitário Júlio Müller). One hundred and thirty one pregnant patients (90.3%) lived in the Great Cuiabá region (including the Cuiabá and Várzea Grande cities) and only 14 (9.7%) lived in other Mato Grosso upstate cities. One hundred and one patients (69.6%) were born in the Mid-Western region, 14 (9.7%) were born in the Southeastern region, and 7 (4.8%) were born in the Northern region of the country. The mean age of the patients was 27.8 ± 5.6 years (median, 27 years). As regards ethnicity, 74 patients (51.0%) were white, 62 (42.8%) were mulattos and nine (6.2%) were black, notwithstanding the difficulties in distinguishing ethnicities in Brazil. One hundred and thirty six patients (93.8%) reported a stable relationship with the child’s father, although not necessarily sharing the same roof, while nine patients did not have stable partners. Forty nine patients (33.8%) did not have a remunerated activity as they were either housewives or students. As regards schooling, 24 (16.5%) patients had not completed high school, therefore having not obtained a professionalizing education, 79 (54.5%) had completed high school and 42 (29.0%) were undergoing or had completed university courses.
Patients’ stature ranged between 1.47 m and 1.80 m, while reported weight before pregnancy ranged between 39 kg and 127 kg. As regards pregestational BMI, 10 (6.9%) were underweight, with BMI values up to 18.4. The total number of patients with normal BMI (between 18.5 and 24.9) was 102 (70.3%), while 33 patients (22.8%) were overweight or obese (BMI above 25.0). With respect to obstetric history, 59 patients were primigravidae, while 45 (31.0%) were secundigravidae, and 41 (28.3%) had had two or more previous pregnancies. Thirty-four patients (23.4%) had previously presented miscarriage, and of those 28 (19.3%) had undergone curettage. Preterm delivery was recorded in the history of six (4.1%) patients. Only five (3.4%) patients were smokers and 10 were alcoholic, although their alcohol intake has not been quantified.
The distribution of patients assessed at each week of the study is shown on Table 1. Cervical funneling was observed in seven patients (4.8%). Uterine cervix length at each gestational week is also shown on Table 1. It is observed that the uterine cervix length gradually decreases as the gestational age progresses, with a negative linear relationship between the two variables, with
R = –0.351 and
R2 = 0.123. The regression curve y = 58.56 – 0.79x, with y corresponding to cervical length and x to gestational age, is significant (
p < 0.001) and demonstrates a mean cervical shortening of 0.8 mm at each gestational week in the period between the 20th and the 34th weeks. While in the group of patients with no history of preterm delivery the cervix length was 38.1 ± 8.6 mm, in those with previous history of preterm delivery the cervix length was 35.5 ± 8.0 mm (
p = 0.473). In the group with no previous history of miscarriage the uterine cervix length was 37.7 ± 8.2 mm, while in the group with a previous history of at least one miscarriage event the length was 37.9 ± 9.1 mm (
p = 0.937). In the seven cases (4.8%) with funneling, the cervix length was 27.7 ± 5.6 mm, as compared with 38.3 ± 8.2 mm in the group without funneling (
p = 0.001). The nulliparous patients, including those with a previous history of miscarriage (71 patients; 49.0%) presented a mean uterine cervix length of 38.1 ± 8.4 mm, while the patients with at least one previous delivery (74 patients; 51.0%) presented a mean uterine cervix length of 37.4 ± 8.4 mm (
p = 0.606). As regards pregestational BMI, calculated with basis on weight reported by the patients themselves, those who were underweight presented a mean uterine cervix length of 37.9 ± 9.7 mm, while in those with a normal BMI the mean was 37.3 ± 7.9 mm, and in those overweight or obese the mean value was 39.1 ± 9.4 mm (
p = 0.565).
With a view on providing a reference chart, the interpolation of the 5th, 50th and 95th percentiles was made (Figure 2). The curve obtained by means of the square polynomial model demonstrates that at the 20th gestational week, the 5th, 50th and 95th percentiles were, respectively, 34 mm, 42 mm and 52 mm, and at the 33rd week they were, respectively, 21 mm, 31 mm and 38 mm.
DISCUSSION
Many studies involving measurements of uterine cervix length in healthy pregnant women at certain gestational ages have been developed. However only few charts with measurements along the gestational period are found to be utilized in the clinical practice(10–12). The measurement of uterine cervix length, as a predictive method, is superior as compared with other screening methods (funneling, cervical volume or absence of glandular tissue around the endocervical canal) based on ultrasonography(4,8,13) in the evaluation of the possibility or risk for preterm delivery in low-risk populations. A small number of publications are focused on the uterine cervix study during the gestational period by means of magnetic resonance imaging. The comparison between the two imaging methods in the evaluation of cervical biometry did not present any statistical difference. Such finding reinforces the utilization of ultrasonography for such purpose considering the low cost and wide availability of this method(14).
The population of the State of Mato Grosso originates from several Brazilian states, so the present study comprises a sample of patients originating from the five Brazilian geographic regions, including a low-risk population with singleton pregnancies in which screening tests for preterm delivery present a low sensitivity and low positive predictive value. In fact, the prevalence of preterm delivery in this population is low, making screening protocols inaccurate. Even so, it is believed that the measurement of uterine cervix length may be utilized as a valuable method to evaluate the risk for preterm delivery(15). Thus, the establishment of the normal values is instrumental in the comparison of lengths and, consequently, in the detection of abnormalities as early as possible.
As regards prognosis, the definition of uterine cervix length by means of ultrasonography seems to be more efficient as a short-term predictor rather than a long-term one. Therefore, serial scans at every 10–14 days should be recommended to women with short uterine cervix or with shortening of the uterine cervix length. Novaes et al., in a study with pregnant women at risk for preterm delivery, have demonstrated that the single predictive factor independent from delivery within 48 hours was the uterine cervix length(16). In a previous study developed by other authors, one observed that a weekly shortening of 4.1 mm, measured between 15 and 24 weeks of gestation in high-risk patients had a significant correlation with incompetent cervix(9). In another study evaluating 183 pregnant women, one observed a weekly mean cervical shortening of 0.9 mm in patients between 16 and 23 weeks and 6 days; in those patients with spontaneous preterm delivery before 35 weeks, the mean cervical shortening was 2.5 mm per week(4).
The present study demonstrated a similar uterine cervix shortening, 0.8 mm per week, although assessing women at different gestational ages. Another observation in the study developed by Owen et al. was that the risk for preterm delivery before the 35th. Gestational week decreased by 24% to every additional 5 mm in the cervix length(4). Additionally, the authors observed that cervical shortening over several consecutive weeks indicate increased risk for preterm delivery. Even in women with uterine cervix above the 10th percentile, the risk for preterm delivery increased as the cervical length decreased. Such observation defies the understanding of what a “competent” or “incompetent” cervix is. In truth, the uterine cervix length is an indirect indicator of cervical competency, and should be seen as a continuous rather than a dichotomous variable(4,5). Cervical length measurement between the 10th and 14th gestational weeks has not shown to be a reliable preterm labor predictor(17).
The implementation of the utilization of ultrasonography in the determination of uterine cervix length requires the identification of the best period, the ideal method for the evaluation, determination of the ideal cutoff point and evidences that the intervention will reduce the preterm delivery index in women with a short uterine cervix. One should remember that different pathological and physiological processes lead to preterm delivery. Cervical incompetence is only one of the multiple and complex causes and the measurement of cervical length should never be an isolated action in the evaluation of the patient at risk for preterm delivery.
As the cervical ripening process in the primigravidae is different from that in multiparous women(12,18), the present study may be limited because of the heterogeneity in the patients’ obstetric history. However, results observed in the present study suggest that parity does not seem to be a variable that influences the uterine cervix dynamics. Likewise, no association was observed between previous history of miscarriage or differences in pregestational BMI and uterine cervix length. Screening for the presence of funneling does not seem to add benefits in the prediction of preterm delivery, since significant funneling is usually associated with uterine cervix shortening, therefore not being an independent predictor(19). A significant correlation between presence of funneling and cervical shortening was also observed. The present study was not aimed at identifying cervical incompetence, as such condition is usually detected at ultrasonography in the period between the 17th and 22nd gestational weeks(20,21), and the measurements of the uterine cervix length started at the 20th gestational week. In the reviewed literature, the current indications to start cervical length measurements before the 20th gestational week are previous history of preterm delivery or previous surgical intervention in the cervix(20), conditions established as exclusion criteria in the present study.
The data obtained in the present study may be useful in the identification of pregnant patients with short cervices and increased risk for preterm delivery.
CONCLUSION
In healthy pregnant women, the mean cervical length presents a statistically significant decrease in the period between the 20th and 34th weeks of gestation.
REFERENCES
1. Ludmir J, Sehdev HM. Anatomy and physiology of the uterine cervix. Clin Obstet Gynecol. 2000;43:433–9.
2. Lumley J. Defining the problem: the epidemiology of preterm birth. BJOG. 2003;110 Suppl 20:3–7.
3. Freitas-Júnior RAO, Mauad-Filho F, Duarte G, et al. Evolução do comprimento cervical uterino na gestação, avaliado pela ultra-sonografia transvaginal. Rev Bras Ginecol Obstet. 2003;25:115–21.
4. Owen J, Yost N, Berghella V, et al. Mid-trimester endovaginal sonography in women at high risk for spontaneous preterm birth. JAMA. 2001;286:1340–8.
5. Iams JD, Goldenberg RL, Meis PJ, et al. The length of the cervix and the risk of spontaneous premature delivery. National Institute of Child Health and Human Development Maternal Fetal Medicine Unit Network. N Engl J Med. 1996;334:567–72.
6. Hassan SS, Romero R, Berry SM, et al. Patients with an ultrasonographic cervical length < or =15 mm have nearly a 50% risk of early spontaneous preterm delivery. Am J Obstet Gynecol. 2000;182:1458–67.
7. Heath VCF, Southall TR, Souka APS, et al. Cervical length at 23 weeks of gestation: prediction of spontaneous preterm delivery. Ultrasound Obstet Gynecol. 1998;12:312–7.
8. To MS, Skentou C, Liao AW, et al. Cervical length and funneling at 23 weeks of gestation in the prediction of spontaneous early preterm delivery. Ultrasound Obstet Gynecol. 2001;18:200–3.
9. Guzman ER, Mellon C, Vintzileos AM, et al. Longitudinal assessment of endocervical canal length between 15 and 24 weeks’ gestation in women at risk for pregnancy loss or preterm birth. Obstet Gynecol. 1998;92:31–7.
10. Hoesli IM, Strutas D, Tercanli S, et al. Charts for cervical length in singleton pregnancy. Int J Gynaecol Obstet. 2003;82:161–5.
11. Salomon LJ, Diaz-Garcia C, Bernard JP, et al. Reference range for cervical length throughout pregnancy: non-parametric LMS-based model applied to a large sample. Ultrasound Obstet Gynecol. 2009;33:459–64.
12. Theron G, Schabort C, Norman K, et al. Centile charts of cervical length between 18 and 32 weeks of gestation. Int J Gynaecol Obstet. 2008;103:144–8.
13. Chao AS, Chao A, Hsieh PC. Ultrasound assessment of cervical length in pregnancy. Taiwan J Obstet Gynecol. 2008;47:291–5.
14. Brandão RS, Pires CR, Souza E, et al. Avaliação biométrica do colo uterino durante a gestação por meio da ultra-sonografia transvaginal e ressonância magnética. Radiol Bras. 2008;41:235–9.
15. Berghella V. Novel developments on cervical length screening and progesterone for preventing preterm birth. BJOG. 2009;116:182–7.
16. Novaes CEF, Koch HA, Montenegro CAB, et al. Diagnóstico do parto pré-termo pela medida ultrassonográfica do comprimento do colo uterino. Radiol Bras. 2009;42:295–8.
17. Ozdemir I, Demirci F, Yucel O, et al. Ultrasonographic cervical length measurement at 10-14 and 20-24 weeks gestation and the risk of preterm delivery. Eur J Obstet Gynecol Reprod Biol. 2007;130:176–9.
18. Grgic O, Matijevic R, Vasilj O. Qualitative glandular cervical score as a potential new sonomorphological parameter in screening for preterm delivery. Ultrasound Med Biol. 2006;32:333–8.
19. Pires CR, Moron AF, Mattar R, et al. Estudo comparativo entre marcadores ultra-sonográficos morfológicos preditores de parto pré-termo: sinal do afunilamento do colo e ausência do eco glandular endocervical. Radiol Bras. 2005;38:17–24.
20. Rozenberg P, Gillet A, Ville Y. Transvaginal sonographic examination of the cervix in asymptomatic pregnant women. Ultrasound Obstet Gynecol. 2002;19:302–11.
21. Yoshizato T, Obama H, Nojiri T, et al. Clinical significance of cervical length shortening before 31 weeks’ gestation assessed by longitudinal observation using transvaginal ultrasonography. J Obstet Gynaecol Res. 2008;34:805–11.
1. Master, Professor, Department of Gynecology and Obstetrics, Faculdade de Medicina da Universidade de Cuiabá (UNIC), Cuiabá, MT, Brazil.
2. PhDs, Associate Professors, Department of Gynecology and Obstetrics, Faculdade de Ciências Médicas da Universidade Federal de Mato Grosso (UFMT), Cuiabá, MT, Brazil.
Mailing Address:
Dra. Rejane Martins Ribeiro Itaborahy
Rua Corumbá, 538, sala 09, Baú
Cuiabá, MT, Brazil, 78008-400
E-mail: rejane_itaborahy@terra.com.br
Received September 25, 2010.
Accepted after revision October 21, 2010.
* Study developed at Faculdade de Ciências Médicas da Universidade Federal de Mato Grosso (UFMT), Cuiabá, MT, Brazil.
