Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 4 - July / Aug. of 2009
Vol. 42 nº 4 - July / Aug. of 2009
|
ORIGINAL ARTICLE
|
|
Percutaneous ethanol sclerotherapy of renal cysts: treatment outcomes and literature review |
|
|
Autho(rs): Giuseppe D'Ippolito, Lucas Rios Torres, Alessandra Caivano Rodrigues Ribeiro, Arcílio de Jesus Roque, Valdemar Ortiz, Sergio Ajzen |
|
|
Keywords: Kidney diseases, Sclerotherapy, Ethanol |
|
|
Abstract:
IProfessor at Department of Diagnostic Imaging - Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/ EPM)
INTRODUCTION Renal cysts are the most common benign lesions in the adult kidney(1). Generally, these lesions are asymptomatic, being incidentally found in elderly patients. Treatment starts being considered as these lesions are associated with flank pain, hypertension, hematuria, infection and collecting system obstruction(1,2). Percutaneous ethanol sclerotherapy is a minimally invasive procedure, and is currently considered as one of the main options for the management of symptomatic renal cysts(1,2). Along the last two decades, a great number of authors have published reports on their experiments with percutaneous treatment of symptomatic renal cysts with different strategies and not always coincidental results(1-21). The objective of this study is to present the practical results from percutaneous ethanol sclerotherapy of renal cysts in a group of ten symptomatic patients submitted to this treatment in the authors' Institution.
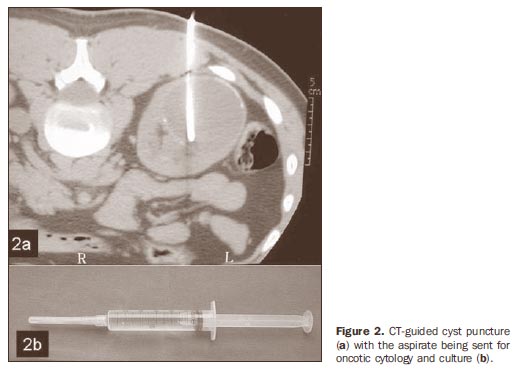
MATERIALS AND METHODS In the period between 2005 and 2007, ten patients (eight men and two women), with a total of ten renal cysts, were submitted to percutaneous sclerotherapy with 95% ethanol. The patients' ages ranged from 22 to 78 years (mean, 55 years). In all of the cases, the indication for the procedure was ipsilateral lumbar pain refractory to other treatments. At least one sonographic examination was performed for each patient to evaluate the number, internal content and walls of cysts. Also, the patients were submitted to contrast-enhanced computed tomography (CT) for evaluation of the relationship between cyst and collecting system (Figure 1). All the lesions were classified as simple cysts (Bosniak category I)(22). The cysts volume ranged between 20 and 1300 ml (mean, 200 ml). Seven patients presented parapyelic cysts, and three, cortical cysts. All the parapyelic cysts caused some degree of dilatation of the pyelocalyceal system by extrinsic compression (Figure 1). Ultrasonography-guided and CT-guided procedures were performed, respectively in two and eight cases. The percutaneous procedure comprised six steps, as follows: 1. Determination of the presence of connection between the cyst and the collecting system by intravenous contrast injection (through CT) and calculation of the cyst volume either by US or CT (Figure 1). 2. Cyst puncture, with the aspirate being sent for oncotic cytology and culture (Figure 2).
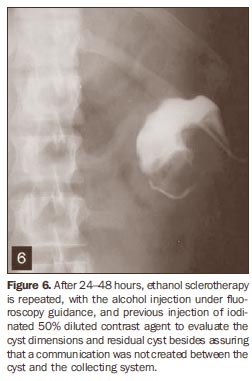
3. Contrast agent injection into the cyst to confirm the connection between the lesion and the colleting system (Figure 3). 4. Percutaneous drain insertion for complete drainage of the cyst content, with measurement of the total aspirate volume (Figure 4). 5. Injection of 95% sterile ethanol into the cyst, corresponding to 25% to 40% of the aspirate volume, up to a maximum volume of 250 ml (Figure 5). 6. Holding definitely the ethanol within the cyst or aspirating it, repeating the procedure within 24 and 48 hours, with a percutaneous 6F or 8.5F drainage catheter (Figures 5 and 6).
Steps 2, 3, 4 and 5 were performed under general anesthesia. The procedures repetition was performed under radioscopic guidance and did not require analgesia or sedation. Changes in decubitus (supine position, left lateral, right lateral and ventral decubitus) were carried out every five minutes. After 20 minutes the injected ethanol was aspirated. More than one procedure was performed for all the patients (on average, two procedures per patient), with a percutaneous 6F or 8.5F drainage catheter that remained in position after the first aspiration. Complete success corresponded to total cyst regression observed at the followup assessments (minimum six months)(1-3). Statistical data analysis was not performed because of the small number of cases, not allowing the calculation of statistical significance.
RESULTS All the procedures were performed with no technical difficulty. The length of the patients' hospital stay ranged between 24 and 72 hours, depending on the number of repetitions (one procedure performed every 24 hours). The procedure repetitions were performed under fluoroscopic guidance and their frequency was established as a function of the cysts size and radiographic aspect; cysts whose size remained unchanged after the first sclerotherapy procedure were immediately submitted to another procedure until a clear decrease in the remainder cyst volume was observed at radioscopy. A patient with a 1300 ml cyst, initially received a 250 ml 95% ethanol injection (about 20% of the cyst volume), with three repetitions along three consecutive days. No complication was observed. The procedure was well tolerated by all the patients. As far the reduction in the cysts dimensions is concerned, a complete success was achieved in seven patients, and partial success was achieved in three. The ten patients submitted to percutaneous sclerotherapy presented improvement in clinical symptoms.
DISCUSSION The main indications for treatment of simple renal cysts are the following: a) voluminous cysts causing hydronephrosis; b) refractory pain; c) hematuria; d) hypertension(1). Studies have demonstrated that a the simple drainage of a cyst leads to recurrence of symptoms in up to 80% of cases, therefore this is not considered as an effective therapeutic approach(3). On the other hand, US, CT, or fluoroscopy-guided percutaneous sclerotherapy have been successfully applied with a variety of substances such as pure ethyl alcohol(1) ethyl alcohol diluted with iopamidol(4), lipiodol/ acrylate(5), povidone iodine(6), acetic acid(7), hydrochloride minocycline(8) and tetracycline(9). The ethyl alcohol sclerosing action is due to the fact that after one to three minutes of contact with the ethanol, the cyst epithelial cells become fixed and nonviable. The cyst capsule is completely penetrated after 4-12 hours(3). Several treatment approaches have been proposed basically varying in relation to the number of sessions (single × multiple)(2,3, 10-12) and prolonged(13) or persistent retention(14) of the sclerosing agent with somewhat conflicting outcomes. The described six-step technique is proposed by several authors and was adopted in the present study(1,12-15). The reason for its choice is related to the good results initially achieved. The procedure may be performed either under US or CT guidance. Advantages of US are: low cost, wide availability and realtime capability. The CT advantages are related to the higher anatomic resolution of the method, allowing the evaluation of the communication between the cyst and the renal collecting system simultaneously with the sclerotherapy. Some authors perform the procedure under local(14) and other under general anesthesia arguing for the fact that this measure is better tolerated by the patient, considering that the injection of the alcohol into the cyst may be quite painful(11). Several authors have studied different technical approaches. Hanna & Dahniya have demonstrated that the frequency of symptoms recurrence is smaller with two consecutive sclerotherapy procedures instead of a single procedure(3), and similar results have been reported by Chung et al.(16). Seo et al. have compared results achieved with the utilization of 50% acetic acid and 99% ethyl alcohol in 58 patients, demonstrating better results with acetic acid after a single percutaneous sclerotherapy session(7). Other studies have suggested that a percutaneous suction drain is kept within the cyst for 24-48 hours, which supposedly would reduce the recurrence rate(11); in the authors' experience, this strategy can make the alcohol reinjection through the percutaneous drain more difficult, since the catheter may be obstructed by the aspirated debris. Most recently, a sclerosing treatment without ethanol aspiration was proposed, that is to say, that the sclerosing agent would be left within the cyst for an indeterminate period with results similar to the ones achieved with other more complex techniques, suggesting that this approach is quite practical and effective(14). In a more recent study, results from multiple ethanol sclerotherapy sessions were compared with those of single session OK-432 sclerotherapy. This substance is a blend of low virulence strains of group A streptococcus (Streptococcus pyogenes). According to this study, after one-year treatment, higher efficacy was observed with the utilization of OK-432(21). However, it is important to note that OK432 is not available in Brazil yet. The post-treatment follow-up is generally performed by means of serial US at the 1st, 3rd, 6th, 12 th and 24 th months after the procedure, or at shorter intervals in case of appearance of symptoms(12,14,17). As regards the procedure results, several authors consider that: a) a complete success corresponds to symptoms regression and cyst disappearance; b) partial success corresponds to symptoms regression and cyst persistence with < 50% of its original volume; c) treatment failure corresponds to symptoms persistence and cyst recurrence with > 50% of its original volume (Figure 7). In the literature, the complete success rate for sclerotherapy ranges between 70% and 90%(1,3,10-14,16,17), independently from the technique adopted, but with better results for smaller cysts(18,19). Complications resulting from the procedure rarely occur and generally are selflimited. Most frequent complications are fever, pain, hematuria and small perinephric hematomas(1,12,13,17,18). Contraindications for renal cysts sclerotherapy are those related to percutaneous procedures, such as severe coagulation disorders, communication between the cyst and the renal collection system, and lesions that do not meet the simple cysts criteria, with suspicion of infection or with presence of blood in the aspirate(4,17,20).
CONCLUSION Renal cysts management by means of percutaneous ethanol sclerotherapy is a safe, effective and minimally invasive method that is well tolerated by the patients, with satisfactory mid- and long-term results, and thus it should be considered as a feasible therapeutic approach for the management of simple renal cysts in symptomatic patients.
REFERENCES 1. Mohsen T, Gomha MA. Treatment of symptomatic simple renal cysts by percutaneous aspiration and ethanol sclerotherapy. BJU Int. 2005;96:1369-72. [ ] 2. Gasparini D, Sponza M, Valotto C, et al. Renal cysts: can percutaneous ethanol injections be considered an alternative to surgery? Urol Int. 2003;71:197-200. [ ] 3. Hanna RM, Dahniya MH. Aspiration and sclerotherapy of symptomatic simple renal cysts: value of two injections of a sclerosing agent. AJR Am J Roentgenol. 1996;167:781-3. [ ] 4. Yamamoto K, Sakaguchi H, Anai H, et al. Sclerotherapy for simple cysts with use of ethanolamine oleate: preliminary experience. Cardiovasc Intervent Radiol. 2005;28:751-5. [ ] 5. Kim SH, Moon MW, Lee HJ, et al. Renal cyst ablation with n-butyl cyanoacrylate and iodized oil in symptomatic patients with autosomal dominant polycystic kidney disease: preliminary report. Radiology. 2003;226:573-6. [ ] 6. Peyromaure M, Debré B, Flam TA. Sclerotherapy of a giant renal cyst with povidone-iodine. J Urol. 2002;168:2525. [ ] 7. Seo TS, Oh JH, Yoon Y, et al. Acetic acid as a sclerosing agent for renal cysts: comparison with ethanol in follow-up results. Cardiovasc Intervent Radiol. 2000;23:177-81. [ ] 8. Uemasu J, Fujihara M, Munemura C, et al. Cyst sclerotherapy with minocycline hydrochloride in patients with autosomal dominant polycystic kidney disease. Nephrol Dial Transplant. 1996;11: 843-6. [ ] 9. van der Ent CK, van Dalen A, Enterman JH. Antibiotic sclerotherapy for renal cysts. Rofo. 1989; 150:339-41. [ ] 10. Delakas D, Karyotis I, Loumbakis P, et al. Longterm results after percutaneous minimally invasive procedure treatment of symptomatic simple renal cysts. Int Urol Nephrol. 2001;32:321-6. [ ] 11. De Dominicis C, Ciccariello M, Peris F, et al. Percutaneous sclerotization of simple renal cysts with 95% ethanol followed by 24-48 h drainage with nephrostomy tube. Urol Int. 2001;66:18-21. [ ] 12. Akinci D, Akhan O, Ozmen M, et al. Long-term results of single-session percutaneous drainage and ethanol sclerotherapy in simple renal cysts. Eur J Radiol. 2005;54:298-302. [ ] 13. Lin YH, Pan HB, Liang HL, et al. Single-session alcohol-retention sclerotherapy for simple renal cysts: comparison of 2- and 4-hr retention techniques. AJR Am J Roentgenol. 2005;185:860-6. [ ] 14. Falci-Júnior R, Lucon AM, Cerri LM, et al. Treatment of simple renal cysts with single-session percutaneous ethanol sclerotherapy without drainage of the sclerosing agent. J Endourol. 2005;19:834-8. [ ] 15. Akinci D, Gumus B, Ozkan OS, et al. Single-session percutaneous ethanol sclerotherapy in simple renal cysts in children: long-term follow-up. Pediatr Radiol. 2005;35:155-8. [ ] 16. Chung BH, Kim JH, Hong CH, et al. Comparison of single and multiple sessions of percutaneous sclerotherapy for simple renal cyst. BJU Int. 2000;85:626-7. [ ] 17. Paananen I, Hellström P, Leinonen S, et al. Treatment of renal cysts with single-session percutaneous drainage and ethanol sclerotherapy: longterm outcome. Urology. 2001;57:30-3. [ ] 18. el-Diasty TA, Shokeir AA, Tawfeek HA, et al. Ethanol sclerotherapy for symptomatic simple renal cysts. J Endourol. 1995;9:273-6. [ ] 19. Agostini S, Dedola GL, Gabbrielli S, et al. Percutaneous treatment of simple renal cysts with sclerotherapy and extended drainage. Radiol Med. 2004;108:522-9. [ ] 20. Gelet A, Sanseverino R, Martin X, et al. Percutaneous treatment of benign renal cysts. Eur Urol. 1990;18:248-52. [ ] 21. Ham WS, Lee JH, Kim WT, et al. Comparison of multiple session 99% ethanol and single session OK-432 sclerotherapy for the treatment of simple renal cysts. J Urol. 2008;180:2552-6. [ ] 22. Bosniak MA. The current radiological approach to renal cysts. Radiology. 1986;158:1-10. [ ] Received February 26, 2009. * Study developed at Hospital São Luiz, and Department of Diagnostic Imaging - Universidade Federal de São Paulo/Escola Paulista de Medicina (Unifesp/EPM), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554