Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 42 nº 3 - May / June of 2009
Vol. 42 nº 3 - May / June of 2009
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Renato Tavares Daher, Renato da Silva Faria, Rubia Kelly Mendes Moreira, Ricardo Tavares Daher |
|
|
Renato Tavares DaherI; Renato da Silva FariaII; Rubia Kelly Mendes MoreiraIII; Ricardo Tavares DaherIV
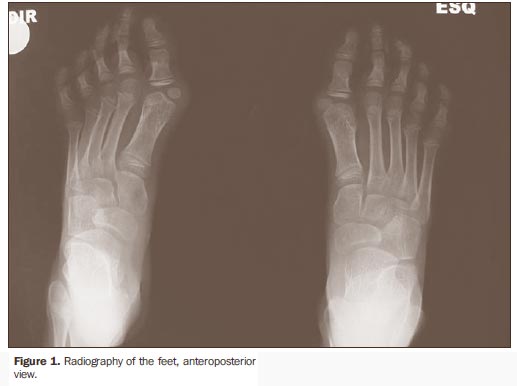
A female, seven-year-old, caucasian patient with pain and increased volume in the right gluteal region, besides limited rotation of the coxofemoral joint at the same side for four months. Additionally, the patient presented bilateral hallux valgus deformity and history of a tumor in the posterior cervical region with no previous trauma, and with motion limitation for five years. Images description Figure 1. Radiography of the feet, anteroposterior view, demonstrating bilateral hallux valgus deformity and shortening of the hallux.
Figure 2. Multidetector computed tomography, axial section and coronal and sagittal reformatting, demonstrating right-sided calcification in the gluteus maximus muscle. Diagnosis: Fibrodysplasia ossificans progressiva.
COMMENTS Fibrodysplasia ossificans progressiva is a condition resulting from autosomal dominant inheritance with variable expression(1)and primary involvement of the conjunctive tissue(2). This disease is characterized by congenital malformation of the hallux and progressive heterotopic calcifications(3), causing deformities and lifelong disability. This is a rare condition whose physiopathogenesis consists of a slow and progressive fibroblastic proliferation, with subsequent ossification and calcification of the conjunctive tissue(2). Fibrodysplasia ossificans progressiva, also known as myositis ossificans progressive or Münchmeyer'syndrome(1), was first reported by Guy Patin describing a "woman who turned into wood"(4). With a prevalence of 0.61 case per million inhabitants(5) and about 700 cases identified in worldwide up to 2008(6), this disease affects all ethnic groups, and is more prevalent in men than in women at a ratio of 4:1(5). Preferentially, children and young adults are affected, on average at the 3.6 years of age(7). It is associated with congenital bone malformations, with bilateral hallux valgus deformity and shortening of the hallux being the most significant findings for raising diagnostic suspicion (reported in 79% to 100% of patients)(3,7). Hand malformations, such as shortening of the first metacarpal bones and brachymesophalangia with clinodactyly of the fifth finger, also may be associated(7), but, in the present case these alterations were not observed. The natural course of the disease is characterized by remissions and exacerbation episodes precipitated by local trauma (vaccinations, anesthetic infiltrations, surgeries)(2,4,7) and infections by the influenza virus(8). Typically, patients present a localized soft-tissue swelling associated with pain and low-grade fever. Along time the soft-tissue masses coalesce, fibrose and calcify, forming "bony bridges" in weeks(2). Typically, heterotopic osteogenesis occurs simultaneously in more than one anatomic region, affecting muscles, fasciae, ligaments, tendons and articular capsules(2). Smooth and cardiac musculatures are not involved(9). It is a disabling disease, with craniocaudal progression and from axial to appendicular bones, primarily affecting the vertebral spine, shoulders, hips and peripheral joints(4). Main radiographic findings include soft-tissues swelling, ectopic ossification, hallux valgus deformity, microdactyly, clinodactyly, monophalanx, scoliosis and subluxation(10). Bone scintigraphy can detect areas with ectopic calcification before radiography can do it, and also may be utilized for determining the disease extent. The application of computed tomography and magnetic resonance imaging is still to be established, but these methods seem to be promising tools in the staging the disease, as well as for detecting new foci undetectable by radiography(2). The histopathology of this disease varies with the lesion progression time, and alteration can be observed only in the affected areas. This focal and evolutive behavior justifies the normal results of the biopsy performed in a non-affected area early in the course of the disease. Generally, precocious lesions present lymphocyte infiltration, macrophages and fibroblasts, later extending to conjunctive tissues with central ossification where osteoblasts, osteocytes and osteoclasts can be observed(7). The diagnosis must be reached in the neonatal period and should be based on clinical and imaging criteria, considering the invasive procedures (surgical resection, biopsy) accelerate the disease progression(4). Differential diagnoses are limited, since the patient's phenotype, clinical history and radiographic findings practically define the diagnosis of fibrodysplasia ossificans progressive. However, other causes for ectopic ossification deserve to be mentioned, such as Albright's hereditary dystrophy, pseudomalignant heterotopic ossification, progressive osseous heterodysplasia and osteosarcoma(3,7). Up to the present, no effective therapy is available. The disease management is conservative, and based on the primum non nocere principle, avoiding every and all condition which could potentially unleash ectopic ossification(7). The prognosis is poor and, generally the death occurs because of respiratory failure and cor pulmonale as a result of thoracic restriction(4).
REFERENCES 1. Palhares DB, Leme LM. Miosite ossificante progressiva: uma perspectiva no controle da doença. J Pediatr. 2001;77:431-4. [ ] 2. Kransdorf MJ, Meis JM. From the archives of the AFIP. Extraskeletal osseous and cartilaginous tumors of the extremities. Radiographics. 1993; 13:853-84. [ ] 3. Kaplan FS, Xu M, Glaser DL, et al. Early diagnosis of fibrodysplasia ossificans progressiva. Pediatrics. 2008;121:1295-300. [ ] 4. Sferco A, Naser C, Robledo H, et al. Fibrodisplasia osificante progresiva: pautas para su reconocimiento. Arch Argent Pediatr. 2001;99:249-52. [ ] 5. Connor JM, Skirton H, Lunt PW. A three generation family with fibrodysplasia ossificans progressiva. J Med Genet. 1993;30:687-9. [ ] 6. Kaplan FS, Pignolo RJ, Shore EM, et al. The seventeenth annual report of the fibrodysplasia ossificans progressiva (FOP) collaborative project. FOP Connection. 2008;21:1-18. [ ] 7. Araújo Jr CR, Carvalho TN, Costa MAB, et al. Fibrodisplasia ossificante progressiva: relato de caso e achados radiográficos. Radiol Bras. 2005; 38:69-73. [ ] 8. Scarlett RF, Rocke DM, Kantanie S, et al. Influenza-like viral illnesses and flare-ups of fibrodysplasia ossificans progressiva. Clin Orthop Relat Res. 2004;(423):275-9. [ ] 9. Ramírez AR, Cock PR. Fibrodisplasia osificante progresiva: reporte de un caso. Rev Colomb Ortop Traumatol. 2002;16:27-30. [ ] 10. Norman A. Escoliose e anomalias com acometimento geral do esqueleto. In: Greenspan A, editor. Radiologia ortopédica. 2ª ed. Rio de Janeiro: Guanabara Koogan; 1996. p. 920-4. [ ]
Study developed at Centro de Reabilitação e Readaptação Dr. Henrique Santillo (CRER), Goiânia, GO, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554