Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 2 - Mar. / Apr. of 2010
Vol. 43 nº 2 - Mar. / Apr. of 2010
|
WHICH IS YOUR DIAGNOSIS?
|
|
|
|
|
Autho(rs): Marcelo Souto Nacif, Amarino Carvalho de Oliveira Junior, Ricardo Oliveira Falcão, Mauro Esteves de Oliveira, David A. Bluemke, Carlos Eduardo Rochitte |
|
|
IProfessor at Radiology Departament, Faculdade de Medicina da Universidade Federal Fluminense, Niterói, RJ, Brazil, Fellow of Radiology and Imaging Sciences, Clinical Center of National Institutes of Health (NIH), Bethesda, MD, USA
Female, 40-year-old, 1.67 m tall patient, weighing 71 kg, with cardiac frequency of 85 bpm, blood pressure 110 × 70 mmHg, reporting chest pain and dyspnea associated with an apparent ST segment elevation at anterior wall ECG. Enzymatic curve elevation was not observed. The patient's social history revealed a serious family argument in the afternoon with the onset of pain early in the evening. Echocardiogram demonstrated a left ventricular apical aneurysm, and coronary computed tomography angiogram was normal. The patient was referred to the Unit of Radiology and Diagnostic Imaging of Hospital Pró-Cardíaco for evaluation using cardiac magnetic resonance imaging. Images description Figure 1. Coronary CT angiogram. Coronary obstruction is not present.
Figure 2. ECG-gating acquisitions of cine-MRI at systole, long axis two-chamber view and short axis from the base to the left ventricular apex. Note the basal hyperkinesia with increase in the parietal thickness and the middle-apical hypocontractility of the left ventricle with ventricular ballooning during systole.
Figure 3. ECG-gating acquisitions of cine-MRI – systole and diastole – and delayed enhancement on long axis three-chamber view (left ventricle output). No evidence of myocardial delayed enhancement is present that would otherwise be present following myocardial infarction.
Diagnosis: Stress-induced cardiomyopathy (transient left ventricular apical ballooning, broken-heart syndrome or Takotsubo syndrome).
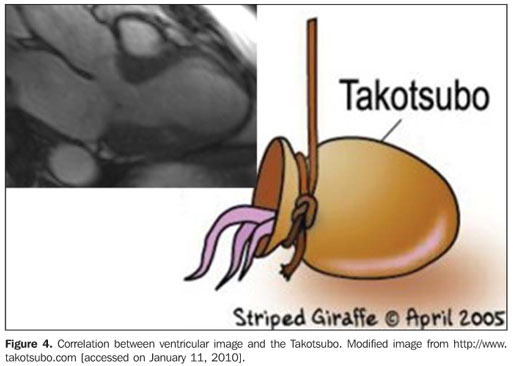
COMMENTS Firstly described by a Japanese group – Satoh et al.(1), early in the 1990's decade – as a condition affecting preferentially middle-aged women who, after going through high-degree stress, presented clinical findings similar to those of acute myocardial infarct (precordial pain, changes in cardiac enzymes, segmental involvement of the left ventricle), while the coronary vessels were normal(1,2). In stress-induced cardiomyopathy (Takotsubo syndrome), either a single or both ventricles may be compromised. Additionally, the condition may present as a reverse syndrome with mid-ventricular akinesia, and hypercontractility of the basal and apical segments(1–3). The precise physiopathology of this syndrome remains unknown; however the condition is associated with exaggerated sympathetic stimulation suggesting catecholamine release as a common pathway for this condition(3,4). Regional differences in the adrenergic anatomy and enervation may explain the different clinical presentations and segmental functional changes(3–5). The clinical presentation may be very similar to that of acute myocardial infarct because of (transient) left ventricular dysfunction, associated chest pain, electrocardiographic changes and mild enzyme elevation, mimicking an infarction(4,5). In cases mimicking acute coronary syndrome, catheterization is required but is negative for coronary occlusion. Cardiac ventriculography can identify left ventricular ballooning. In clinical cases where the likelihood of acute coronary syndrome is low, coronary CT angiography may be performed along with cardiac enzyme evaluation, as in the present case(1,3,4). Echocardiography, left ventriculography, cardiac CT angiography and magnetic resonance imaging demonstrate apical ballooning with hyperkinesia of the ventricular basal segment, resembling a fishing pot for trapping octopus utilized in Japan (Takotsubo) (Figure 4)(5).
Takotsubo syndrome may be triggered by quite variable factors, including stress. Multiple factors have already been reported as triggering factors: psychological conditions, exacerbation of systemic, pulmonary, neurogenic, gastrointestinal and renal diseases, besides other non-specific factors. Patients with pheochromocytoma or those submitted to echocardiogram with dobutamine may also develop this cardiomyopathy(6–8). Stress related syndrome is most frequent in women aged between 60 and 75 years of age. The most common symptom is retrosternal pain; however some clinical presentations may mimic an acute coronary syndrome with dyspnea, increased cardiac enzymes (troponin) and electrocardiographic abnormalities. More severe cases may progress with cardiogenic shock and respiratory failure as a result of acute pulmonary edema(2,3,6). Absence of significant coronary obstruction and reversibility of left ventricular dysfunction constitute relevant concepts to be taken into consideration for the diagnosis, with recovery of the ventricular function on average in up to 18 days, although it may take up to three months from the symptoms onset(1,3,4,7). Although the actual prevalence of this condition is still to be defined, retrospective surveys suggest that 2% of cases assisted as acute coronary syndrome are diagnosed as Takotsubo syndrome(1–3). Cardiac magnetic resonance imaging Cardiac magnetic resonance imaging with the delayed enhancement technique can characterize the absence of a significant myocardial lesion, allowing the detection of a possible ischemic lesion/infarct and the exclusion of myocarditis as a differential diagnosis(9,10,11). Magnetic resonance imaging can demonstrate changes in the ventricular contractility and is useful as follow-up study because of the absence of ionizing radiation or nephrotoxic contrast agent. Final considerations Cardiac magnetic resonance imaging should be performed in all patients with diagnostic suspicion for a correct characterization of the absence of myocyte lesion and follow-up of the disease. In the present case, the clinical and imaging follow-up with resolution of the change in the segmental contraction confirms the diagnosis. The condition management is based on hemodynamic support measures.
REFERENCES 1. Satoh H, Tateishi H, Uchida T, et al. Takotsubo-type cardiomyopathy due to multivessel spasm. In: Kodama K, Haze K, Hon M, editors. Clinical aspects of myocardial injury: from ischemia to heart failure. Tokyo: Kagakuhyouronsya Co.; 1990. p. 56–64. [ ] 2. Lemos AET, Araújo Junior AL, Lemos MT, et al. Síndrome do coração partido (síndrome de Takotsubo). Arq Bras Cardiol. 2008;90:e1–e3. [ ] 3. Vasconcelos JT, Martins S, Sousa JF, et al. Cardiomiopatia de Takotsubo: uma causa rara de choque cardiogênico simulando infarto agudo do miocárdio. Arq Bras Cardiol. 2005;85:128–30. [ ] 4. Ishikawa K. "Takotsubo" cardiomyopathy. A syndrome characterized by transient left ventricular apical ballooning that mimics the shape of bottle used for trapping octopus in Japan. Intern Med. 2004;43:275–6. [ ] 5. Simões MV, Marin-Neto JA, Romano MMD, et al. Disfunção ventricular esquerda transitória por cardiomiopatia induzida por estresse. Arq Bras Cardiol. 2007;89:e79–e83. [ ] 6. Vasconcelos Filho FJC, Gomes CAM, Queiroz OA, et al. Síndrome do coração partido (síndrome de Takotsubo) induzida por ecocardiograma de estresse com dobutamina. Arq Bras Cardiol. 2009;93:e5–e7. [ ] 7. Van de Walle SO, Gevaert SA, Gheeraert PJ, et al. Transient stress-induced cardiomyopathy with an "inverted Takotsubo" contractile pattern. Mayo Clin Proc. 2006;81:1499–502. [ ] 8. Sanchez-Recalde A, Costero O, Oliver JM, et al. Images in cardiovascular medicine. Pheochromocytoma-related cardiomyopathy: inverted Takotsubo contractile pattern. Circulation. 2006; 113:e738–9. [ ] 9. Teraoka K, Kiuchi S, Takada N, et al. Images in cardiovascular medicine. No delayed enhancement on contrast magnetic resonance imaging with Takotsubo cardiomyopathy. Circulation. 2005;111:e261–2. [ ] 10. Eitel I, Behrendt F, Schindler K, et al. Differential diagnosis of suspected apical ballooning syndrome using contrast-enhanced magnetic resonance imaging. Eur Heart J. 2008;29:2651–9. [ ]
Study developed at the Unit of Radiology and Diagnostic Imaging of Hospital Pró-Cardíaco, Rio de Janeiro, RJ, at Hospital Universitário Antônio Pedro da Universidade Federal Fluminense (HUAP-UFF), Niterói, RJ, and at Plani Diagnósticos Médicos por Imagem, São José dos Campos, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554