Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 1 - Jan. /Feb. of 2010
Vol. 43 nº 1 - Jan. /Feb. of 2010
|
ICONOGRAPHIC ESSAY
|
|
Magnetic resonance imaging of ankle impingement syndrome: iconographic essay |
|
|
Autho(rs): Claudio Marcio Amaral de Oliveira Lima, Erica Barreiros Ribeiro, Elisa Pompeu Dias Coutinho, Evandro Miguelote Vianna, Rômulo Côrtes Domingues, Antonio Carlos Coutinho Júnior |
|
|
Keywords: Magnetic resonance imaging, Syndrome, Impingement, Ankle |
|
|
Abstract:
IMD, Radiologist, Centro de Diagnóstico por Imagem Fátima Digittal, Nova Iguaçu, RJ, Brazil
INTRODUCTION Ankle impingement syndrome is a painful condition resulting from friction of joint tissues that is both cause and effect of an altered joint biomechanics. Main causes include post-traumatic lesions, particularly ligament lesions, resulting in chronic ankle pain. From the clinical and anatomical point of view, such syndrome is classified into anterolateral, anterior, anteromedial, posteromedial and posterior(1-3). The present study is aimed at illustrating, as an iconographic essay, the main magnetic resonance imaging (MRI) findings of ankle impingement syndrome.
MRI PROTOCOLS The patients are previously instructed to not utilize any type of substance (ointments, gel or cream) on the ankle, and before being submitted to MRI, they are interviewed by the clinical team on the presence, intensity and localization of the pain, type of trauma and respective dynamics (inversion, eversion, hyperextension or flexion, if either direct or indirect, etc.) previous history of surgery, endocrinopathy or rheumatologic diseases, either in association or not, and type of physical activity, if any. The sequences utilized in the protocol for study of the ankle, both with a 1.5 T unit (Magnetom Avanto; Siemens Medical Systems, Erlangen, Germany) and with a 3 T unit (Magnetom Trio; Siemens Medical Systems; Erlangen, Germany) are respectively: sagittal, T1-weighted (Avanto - FOV: 170; slice thickness: 4/25; matrix: 512 × 282; NEX: 1; acquisition time: 1.55 min; TR: 400; TE: 20. Trio - FOV: 160; thickness: 3/0.6; matrix: 384 × 307; NEX: 2; acquisition time: 1.16 min; TR: 641; TE: 11) and axial (Avanto - FOV: 160; thickness: 3/30; matrix: 384 × 214; NEX: 1; acquisition time: 1.21 min; TR: 552; TE: 24. Trio - FOV: 160; thickness: 3/0.3; matrix: 384 x 307; NEX: 2; acquisition time: 1.45 min; TR: 500; TE: 11), STIR sequences or proton density with fat suppression at sagittal plane (Avanto - FOV: 170; thickness: 4/25; matrix: 320 × 208; NEX: 1; acquisition time: 2.04 min; TR: 3000; TE: 33. Trio - FOV: 160; thickness: 3/0.6; matrix: 320 × 256; NEX: 2; acquisition time: 1.53 min; TR: 2500; TE: 44), sequences at proton density, coronal plane (Avanto - FOV: 170; thickness: 3/30; matrix: 320 × 146; NEX: 1; acquisition time: 2.29 min; TR: 4810; TE: 33. Trio - FOV: 160; thickness: 3/0.6; matrix: 320 × 256; NEX: 2; acquisition time: 1.45 min; TR: 2690; TE: 42) and axial plane (Avanto - FOV: 160; thickness: 3/30; matrix: 320 × 179; NEX: 1; acquisition time: 1.36 min; TR: 2600; TE: 25. Trio - FOV: 160; thickness: 3/0.3; matrix: 320 × 256; NEX: 2; acquisition time: 2.01 min; TR: 3100; TE: 42).
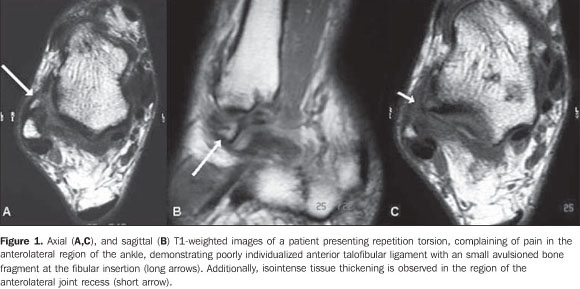
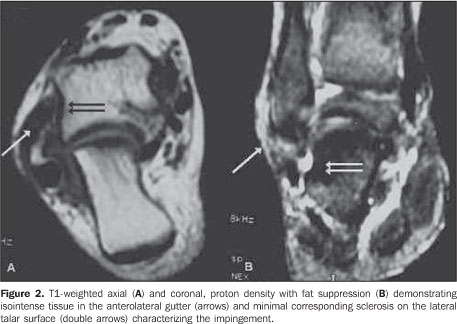
CLASSIFICATION Anterolateral ankle impingement Anterolateral ankle impingement is a common cause of chronic lateral pain in the ankle produced by hypertrophic synovial tissue entrapment in the anterolateral gutter of the ankle. It is estimated that approximately 3% of ankle sprains lead to anterolateral impingement(1-4) . The etiology is related to small repeated inversion traumas, initially with no significant mechanical instability. Microtraumas continuity results in inflammation, synovial hypertrophy and fibrosis, causing pain and mechanical instability. In the most advanced forms, an organized meniscal lesion develops with hypertrophic synovial tissue and fibrosis(1,4), as described by Wolin et al.(5). The anterior talofibular ligament and the tibiofibular ligament were implied as causes for such impingement(4). The presence of anterior or anterolateral bone impingement caused by osteophytes may exacerbate this condition. The accessory fascicle of the anterior tibiofibular ligament (Bassett's ligament)(6), that is a common anatomic variation, may present hypertrophy after repeated trauma, resulting in anterolateral impingement, particularly if other supporting structures of the region are involved(1,4). At MRI, the presence of soft tissue mass or fibrotic band in the anterolateral ankle gutter, different from the anterior talofibular ligament, suggests the diagnosis(1,4) (Figures 1 and 2). Conventional MRI accuracy still remains controversial, and many authors advocate the utilization of MRI only in the presence of a significant joint effusion. Magnetic resonance arthrography represents an excellent tool for diagnostic elucidation before arthroscopy, and a relevant finding is the absence of fluid in the recess between the soft tissues of the anterolateral region and the anterior fibular surface, because of the presence of adhesions and cicatricial tissue between the fibula and the joint capsule, preventing the fluid to enter the recess(1,4).
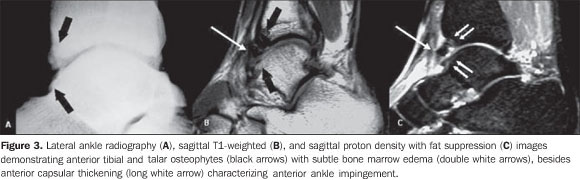
Anterior ankle impingement Anterior ankle impingement is well established and relatively common cause of chronic ankle pain, and may affect any athlete who is subjected to stress resulting from repeated dorsiflexion, especially soccer players and ballet dancers(1,3). It is widely recognized that dorsiflexion or supination injuries can cause damages to the anterior and medial edges of the joint cartilage, and it is believed that repair of such lesion with cicatricial tissue and proliferative fibrosis leads to the development of osteophytes and joint capsule avulsion. Also, another theory suggests that forced dorsiflexion results in repeated microtraumas on the tibia and talus, with consequential microfractures of the trabecular bone/periosteal hemorrhage, stimulating the formation of a new bone tissue. Anterior tibial and talar osteophytes impinge on each other, particularly at dorsiflexion, determining an impingement on the interposed soft tissues(1,3) (Figure 3).
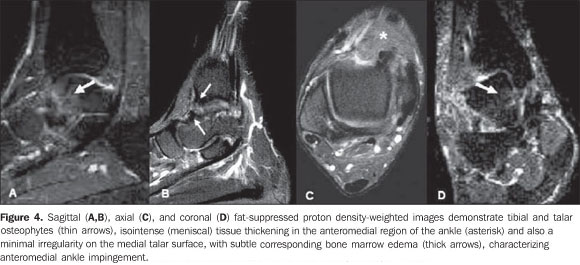
Remarkably in soccer players, at the moment of the kick, the Ball causes a direct trauma on the anterior tibiotalar joint, since at this moment the joint cartilage is covered only by the subcutaneous fat(1). A study has demonstrated that a significant percentage of professional athletes (45-59%) presented osteophytes at conventional radiography, with no symptom of previous impingement, which leads to the conclusion that the association of cicatrization and synovial thickening is more significant than simply the presence of osteophytes to produce the clinical syndrome(1,3). Conventional radiography demonstrates osteophytes and the conventional MRI allows the evaluation of soft tissues, visualization of tibiotalar osteophytes positioning in relation to the capsule, the synovitis in the anterior capsular recess, and the presence, although rare, of bone marrow edema. Synovial thickening usually presents hypointense signal on T1-weighted sequences, and low to intermediate signal intensity on T2-weighted sequences, more clearly outlined in the presence of joint effusion(1,3). Anteromedial ankle impingement Anteromedial ankle impingement is a clinical entity increasingly recognized in the orthopedic literature as an uncommon cause of chronic ankle pain(1). The exact mechanism of the anteromedial ankle impingement is still to be understood, however it is believed that it may be a result, initially, of a forced supination with a rotational component, leading to an injury of the anteromedial joint capsule. The repeated anterolateral impingement and subsequent microtrauma produce synovitis and joint capsule thickening. Additionally, bone and joint cartilage lesion may result in osteophytes formation, besides joint and synovial capsule thickening on the anteromedial surface. The result is a meniscal lesion represented by thickening of soft tissues anterior to the tibiotalar ligaments that may appear isolatedly or be secondary to a partial injury of the deltoid ligament(1,3). Another cause of impingement is thickening of the anterior tibiotalar ligament. Such thickening or the meniscal lesion determine impingement on the region corresponding to the anteromedial corner during ankle dorsiflexion, resulting in development of osteophytes, chondral lesion or both, commonly associated with an inversion mechanism with injury of lateral or medial ligament(1,3). Magnetic resonance imaging demonstrates the meniscal mass, chondral or osteochondral lesions, ligament thickening, besides osteophytes(1,3) (Figure 4), and conventional radiography demonstrates osteophytes, but, considering the uncommon nature of this condition, no extensive study reporting such imaging findings is available in the literature(4).
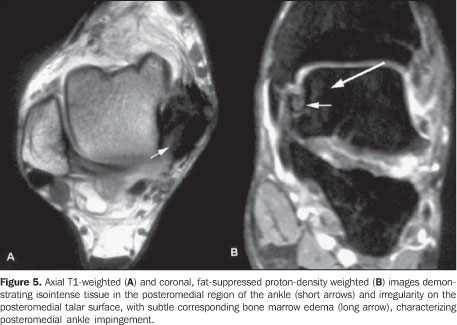
Posteromedial ankle impingement Posteromedial ankle impingement is a common cause of pain after a severe ankle inversion injury in which the deep posterior fibers of the deltoid ligament remain compressed between the medial wall of the talus and the medial malleolus(1,3). Initially, posteromedial symptoms are not noticeable as compared with the symptoms of lateral ligament rupture, and spontaneous resolution is achieved without a specific treatment. However, the inappropriate healing of the posterior deep fibers of the deltoid ligament leads to chronic inflammation, hypertrophic fibrosis and metaplasia. In many cases, such disorganized fibrotic tissue may lead to impingement between the medial wall of the talus and the posterior rim of the medial malleolus(1,3). Magnetic resonance imaging demonstrates the soft tissues thickening and the bone marrow edema of the medial talus and malleolus(1,3) (Figure 5).
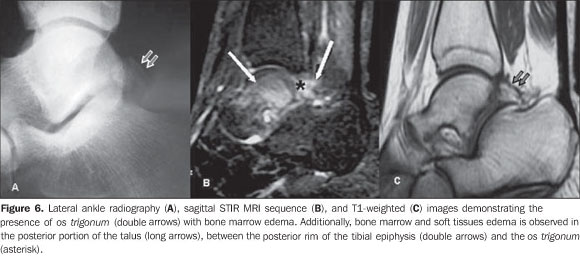
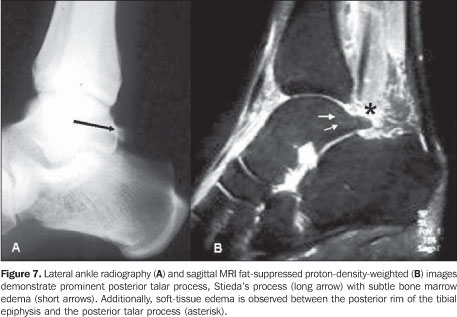
Posterior ankle impingement Posterior ankle impingement corresponds to a set of abnormalities resulting from forced repeated or acute plantar flexion. This syndrome is also called os trigonum syndrome, talar compression syndrome or posterior block of the ankle(1,3,7), and has been extensively described in professional soccer players as well as in classical ballet dancers(1,3). Such type of impingement develops as a result of significant acute injury, such as avulsion of the posterior talofibular ligament, talar fracture or accessory ossicles injury, but, in most of cases the syndrome onset is insidious in predisposed athletes. It is believed that repeated forced foot flexion results in chronic bone and soft tissue lesions. The injury mechanism is similar to a "nutcracker effect" where the posterior portion of the talus and adjacent soft tissues are compressed between the tibia and the calcaneus during the feet plantar flexion(1,3,7). The anatomy of the posterior region of the ankle is a key factor in the development of this type of impingement whose causes are divided into osseous and soft tissue causes. The most frequent cause is osseous in nature and is represented by the os trigonum that is an accessory ossicle of the posterior talar tubercle that may remain unfused in up to 7% of the general population, or by the Stiedas's process that is a prominent lateral talar tubercle. Among the causes originating in soft tissues, synovitis involving the flexor hallucis longus tendon sheath, the posterior intermalleolar ligament and the posterior synovial recess of the tibiotalar and subtalar joints(1,3,7). Such type of impingement may present as soft tissues inflammation in the posterior ankle, accessory ossicles injury or both. Bone lesions include fracture, fragmentation and pseudoarthrosis of accessory ossicles or lateral talar tubercle. Soft tissue lesions include posterior and subtalar synovitis, as well as tenosynovitis of the flexor hallucis longus(1). The hallucis longus flexor runs deeply in the gutter between the medial and lateral talar tubercles, and stenosing tenosynovitis may develop as it is involved in the posterior ankle impingement(1). MRI demonstrates findings such as os trigonum, prominent posterior talar process (Stieda) in association with bone marrow edema, as well as edema or synovitis in the posterior joint recess and adjacent soft tissues(1,3,7) (Figures 6 and 7).
Finally, MRI is an excellent method for demonstrating bone and soft tissues abnormalities in the different types of ankle impingement syndrome, providing useful information not only for confirming the diagnosis but also to differentiate from other causes of joint pain.
REFERENCES 1. Cerezal L, Abascal F, Canga A, et al. MR imaging of ankle impingement syndromes. AJR Am J Roentgenol. 2003;181:551-9. [ ] 2. Hauger O, Moinard M, Lasalarie JC, et al. Anterolateral compartment of the ankle in the lateral impingement syndrome: appearance on CT arthrography. AJR Am J Roentgenol. 1999;173:685-90. [ ] 3. Robinson P, White LM. Soft-tissue and osseous impingement syndromes of the ankle: role of imaging in diagnosis and management. Radiographics. 2002;22:1457-71. [ ] 4. Rosenberg ZS, Beltran J, Bencardino JT. MR imaging of the ankle and foot. Radiographics. 2000;20:S153-79. [ ] 5. Wolin I, Glassman F, Sideman S, et al. Internal derangement of the talofibular component of the ankle. Surg Gynecol Obstet. 1950;91:193-200. [ ] 6. Bassett FH 3rd, Gates HS 3rd, Billys JB, et al. Talar impingement by the anteroinferior tibiofibular ligament. A cause of chronic pain in the ankle after inversion sprain. J Bone Joint Surg Am. 1990;72:55-9. [ ] 7. Karasick D, Schweitzer ME. The os trigonum syndrome: imaging features. AJR Am J Roentgenol. 1996;166:125-9. [ ] Received October 12, 2009. * Study developed at Clínicas de Diagnóstico Por Imagem (CDPI)/Multi-Imagem, Rio de Janeiro, RJ, and Centro de Diagnóstico por Imagem Fátima Digittal, Nova Iguaçu, RJ, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554