Radiologia Brasileira - Publicação Científica Oficial do Colégio Brasileiro de Radiologia
AMB - Associação Médica Brasileira CNA - Comissão Nacional de Acreditação
 Vol. 43 nº 1 - Jan. /Feb. of 2010
Vol. 43 nº 1 - Jan. /Feb. of 2010
|
WHICH IS YOUR DIAGNOSIS?
|
|
Which is your diagnosis? |
|
|
Autho(rs): Ceci Obara Kurimori, Marcelo Bordalo-Rodrigues, Giovanni Guido Cerri |
|
|
IMD, Assistant Physician at Instituto de Ortopedia e Traumatologia - Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (IOT/HC-FMUSP), São Paulo, SP, Brazil
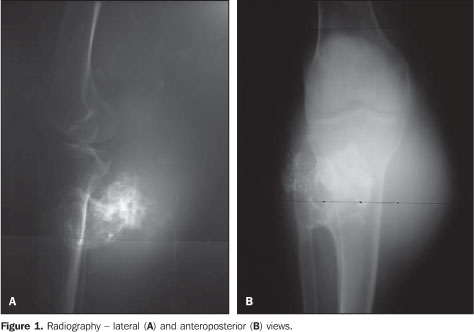
Male, 77-year-old patient. Incidental finding at radiography of left lower limb, with a progressive volumetric increase of the posterior face of the leg, after a fall from a roof two years ago.Images description Figure 1. Radiography - lateral (A) and anteroposterior (B) views demonstrating exostosis with irregular margins in association with soft tissues growth intermingled with chondroid calcifications in the posterior aspect of the leg.
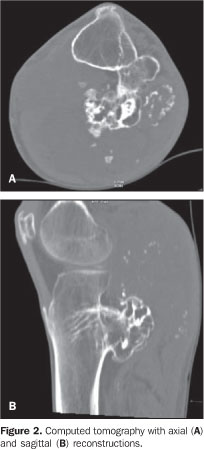
Figure 2. Computed tomography with axial (A) and sagittal (B) reconstructions demonstrating exostosis in the posterior face of the proximal tibial and fibular metaphysis, with irregular surface and voluminous soft parts component intermingled with chondroid calcifications.
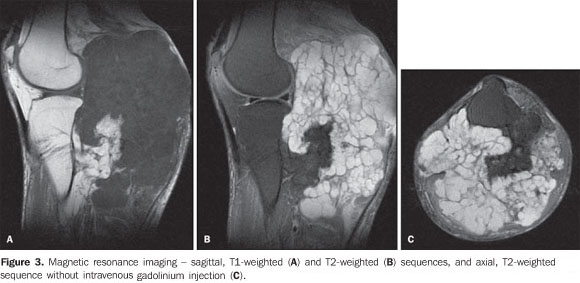
Figure 3. Magnetic resonance imaging - sagittal, T1-weighted (A) T2-weighted (B) sequences, and axial, T2-weighted sequence without intravenous gadolinium injection (C) demonstrating exostosis in the posterior face of the proximal tibial metaphysis, with irregular ill-defined surfaces in association with a voluminous soft-tissue mass with high signal intensity on the T2-weighted image, with lobulated margins and internal septa with low signal intensity (cartilaginous cap).
Diagnosis: Malignant degeneration to chondrosarcoma from a tibial pediculated osteochondroma.
COMMENTS Osteochondroma is the most common bone tumor, representing about 15% of all bone tumors and 20% of benign bone tumors. The radiological aspect of this entity is typical, reflecting its macroscopic appearance composed of medullary and cortical bone projecting from the adjacent bone and covered by a hyaline cartilaginous cap. Such tumors may be either solitary or multiple, the latest ones being generally associated with hereditary multiple exostosis. Some complications may be associated with osteochondromas as follows: bone deformity, fractures (particularly those related to pediculated osteochondromas), vascular alterations (pseudoaneurysms, vascular displacement and occlusion), neurologic compression and bursae formation. Malignant transformation is, however, the most feared complication related to osteochondromas, occurring in approximately 1% of cases of solitary lesions and with highest prevalence in hereditary multiple exostoses (3%-5% of cases)(1,2). Chondrosarcomas secondary to osteochondromas are generally solitary and low grade lesions. Lesions that begin to enlarge and become painful after the skeletal maturity are suspect for malignant transformation, considering that osteochondromas rarely develop after skeletal maturity(1). Generally, these lesions are found between the second and third decades of life, with higher prevalence in men, with slow and indolent growth, clinically presenting with pain and regional edema. The most frequent sites are the metaphyseal region of long bones, particularly femur and humerus(3). Radiological findings suggestive of malignancy include(1,4): 1. Development of osteochondroma in mature skeleton. 2. Irregular or indistinct surface. 3. Focal radiolucency within the lesion. 4. Erosion or destruction of adjacent bone. 5. Significant soft tissue mass containing irregular calcifications. Magnetic resonance imaging plays a useful role in the differentiation between osteochondromas and low-grade chondrosarcomas, the later ones generally presenting a massive, lobulated soft tissue component, with high signal intensity on T2-weighted images and septa with low signal intensity with post-contrast enhancement(2,3,5). The cartilaginous cap thickness represents an important criterion in the identification of malignant degeneration, so thickness > 1.5 cm after skeleton maturity should raise the suspicion of malignancy(1).
REFERENCES 1. Murphey MD, Choi JJ, Kransdorf MJ, et al. Imaging of osteochondroma: variants and complications with radiologic-pathologic correlation. Radiographics. 2000;20:1407-34. [ ] 2. Masciocchi C, Sparvoli L, Barile A. Diagnostic imaging of malignant cartilage tumors. Eur J Radiol. 1998;27(Suppl 1):S86-90. [ ] 3. Chaabane S, Bouaziz MC, Drissi C, et al. Periosteal chondrosarcoma. AJR Am J Roentgenol. 2009;192:W1-6. [ ] 4. Gomes ACN, Silveira CRS, Paiva RGS, et al. Condrossarcoma em paciente com osteocondromatose múltipla: relato de caso e revisão da literatura. Radiol Bras. 2006;39:449-51. [ ] 5. De Beuckeleer LHL, De Schepper AMA, Ramon F. Magnetic resonance imaging of cartilaginous tumors: is it useful or necessary? Skeletal Radiol. 1996;25:137-41. [ ] Study developed at Instituto de Ortopedia e Traumatologia (IOT) and Instituto de Radiologia (InRad) - Hospital das Clínicas da Faculdade de Medicina da Universidade de São Paulo (HC-FMUSP), São Paulo, SP, Brazil. |
|
Av. Paulista, 37 - 7° andar - Conj. 71 - CEP 01311-902 - São Paulo - SP - Brazil - Phone: (11) 3372-4544 - Fax: (11) 3372-4554